Abstract
Background
The aim of this review was to explore the role of three-dimensional (3D) printing in colorectal surgical education and procedural simulation, and to assess the effectiveness of 3D-printed models in anatomic and operative education in colorectal surgery.
Methods
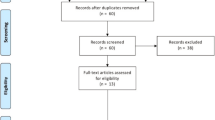
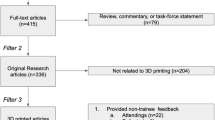
A systematic review of the literature was performed following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to identify relevant publications relating to the use of 3D-printed models in colorectal surgery in an educational context. The search encompassed OVID Medline, Web of Science and EMBASE including papers in English published from 1 January 1995 to 1 January 2023. A total of 1018 publications were screened, and 5 met the criteria for inclusion in this review.
Results
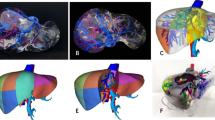
Four distinct 3D models were described across five studies. Two models demonstrated objective benefits in the use of 3D-printed models in anatomical education in academic outcomes at all levels of learner medical experience and were well accepted by learners. One model utilised for preoperative visualisation demonstrated improved operative outcomes in complete mesocolic excision compared with preoperative imaging review, with a 22.1% reduction in operative time (p < 0.001), 9.2% reduction in surgical duration (p = 0.035) and 37.3% reduction in intraoperative bleeding volume amongst novice surgeons (p < 0.01). Technical simulation has been demonstrated in a feasibility context in one model but remains limited in scope and application on account of the characteristics of available printing materials.
Conclusions
3D printing is well accepted and effective for anatomic education and preoperative procedural planning amongst colorectal surgeons, trainees and medical students but remains a technology in the early stages of its possible application. Technological advancements are required to improve the tissue realism of 3D-printed organ models to achieve greater fidelity and provide realistic colorectal surgical simulations.
Similar content being viewed by others
Data Availability
The datasets generated during and analysed during the current study are available from the corresponding author on reasonable request.
References
Emile SH, Wexner SD (2018) Systematic review of the applications of three-dimensional printing in colorectal surgery. Colorectal Dis Codi. https://doi.org/10.1111/codi.14480
Chen JV, Dang ABC, Dang A (2021) Comparing cost and print time estimates for six commercially-available 3D printers obtained through slicing software for clinically relevant anatomical models. 3D Print Med. https://doi.org/10.1186/s41205-020-00091-4
Hamabe A, Ishii M, Kamoda R et al (2022) Artificial intelligence-based technology to make a three-dimensional pelvic model for preoperative simulation of rectal cancer surgery using <scp>MRI</scp>. Ann Gastroenterol Surg 6:788–794. https://doi.org/10.1002/ags3.12574
Tack P, Victor J, Gemmel P, Annemans L (2016) 3D-printing techniques in a medical setting: a systematic literature review. Biomed Eng Online 15:115. https://doi.org/10.1186/s12938-016-0236-4
Hojo D, Nishikawa T, Takayama T et al (2019) 3D printed model-based simulation of laparoscopic surgery for descending colon cancer with a concomitant abdominal aortic aneurysm. Tech Coloproctol 23:793–797. https://doi.org/10.1007/s10151-019-02060-4
Povey M, Powell S, Howes N et al (2021) Evaluating the potential utility of three-dimensional printed models in preoperative planning and patient consent in gastrointestinal cancer surgery. Ann R Coll Surg Engl 103:615–620. https://doi.org/10.1308/rcsann.2020.7102
Chen C, Cai L, Zheng W et al (2019) The efficacy of using 3D printing models in the treatment of fractures: a randomised clinical trial. BMC Musculoskelet Disord 20:65. https://doi.org/10.1186/s12891-019-2448-9
Tominaga T, Takagi K, Takeshita H et al (2016) Usefulness of three-dimensional printing models for patients with stoma construction. Case Rep Gastroenterol 10:61–66. https://doi.org/10.1159/000442663
Nassar AK, Al-Manaseer F, Knowlton LM, Tuma F (2021) Virtual reality (VR) as a simulation modality for technical skills acquisition. Ann Med Surg 71:102945. https://doi.org/10.1016/j.amsu.2021.102945
Pietersen PI, Bjerrum F, Tolsgaard MG et al (2022) Standard setting in simulation-based training of surgical procedures. Ann Surg 275:872–882. https://doi.org/10.1097/SLA.0000000000005209
Aydın A, Ahmed K, Abe T et al (2022) Effect of simulation-based training on surgical proficiency and patient outcomes: a randomised controlled clinical and educational trial. Eur Urol 81:385–393. https://doi.org/10.1016/j.eururo.2021.10.030
Li A, Tang R, Rong Z et al (2018) The use of three-dimensional printing model in the training of choledochoscopy techniques. World J Surg 42:4033–4038. https://doi.org/10.1007/s00268-018-4731-6
Langridge B, Momin S, Coumbe B et al (2018) Systematic review of the use of 3-Dimensional printing in surgical teaching and assessment. J Surg Educ 75:209–221. https://doi.org/10.1016/j.jsurg.2017.06.033
Costello DM, Huntington I, Burke G et al (2022) A review of simulation training and new 3D computer-generated synthetic organs for robotic surgery education. J Robot Surg 16:749–763. https://doi.org/10.1007/s11701-021-01302-8
Papazarkadas X, Spartalis E, Patsouras D et al (2019) The Role of 3D printing in colorectal surgery: current evidence and future perspectives. In Vivo (Brooklyn) 33:297–302. https://doi.org/10.21873/invivo.11475
Przedlacka A, Pellino G, Fletcher J et al (2021) Current and future role of three-dimensional modelling technology in rectal cancer surgery: a systematic review. World J Gastrointest Surg 13:1754–1769. https://doi.org/10.4240/wjgs.v13.i12.1754
Bangeas P (2019) Three-dimensional printing as an educational tool in colorectal surgery. Front Biosci 11:844. https://doi.org/10.2741/e844
Chen Y, Bian L, Zhou H et al (2020) Usefulness of three-dimensional printing of superior mesenteric vessels in right hemicolon cancer surgery. Sci Rep 10:11660. https://doi.org/10.1038/s41598-020-68578-y
Hojo D, Murono K, Nozawa H et al (2020) Utility of a three-dimensional printed pelvic model for lateral pelvic lymph node dissection. Int J Colorectal Dis 35:905–910. https://doi.org/10.1007/s00384-020-03534-w
Hojo D, Murono K, Nozawa H et al (2019) Utility of a three-dimensional printed pelvic model for lateral pelvic lymph node dissection education: a randomized controlled trial. J Am Coll Surg 229:552-559e3. https://doi.org/10.1016/j.jamcollsurg.2019.08.1443
Yiasemidou M, Mushtaq F, Basheer M et al (2021) Patient-specific mental rehearsal with three-dimensional models before low anterior resection: randomized clinical trial. BJS Open. https://doi.org/10.1093/bjsopen/zraa004
Fleming C, Sadaghiani MS, Stellon MA, Javan R (2020) Effectiveness of three-dimensionally printed models in anatomy education for medical students and resident physicians: systematic review and meta-analysis. J Am Coll Radiol 17:1220–1229. https://doi.org/10.1016/j.jacr.2020.05.030
Jin Z, Li Y, Yu K et al (2021) 3D printing of physical organ models: recent developments and challenges. Adv Sci (Weinh) 8:e2101394. https://doi.org/10.1002/advs.202101394
Tejo-Otero A, Buj-Corral I, Fenollosa-Artés F (2020) 3D printing in medicine for preoperative surgical planning: a review. Ann Biomed Eng 48:536–555. https://doi.org/10.1007/s10439-019-02411-0
Smektala T, Goląb A, Królikowski M, Slojewski M (2016) Low cost silicone renal replicas for surgical training—technical note. Arch Esp Urol 69:434–436
Kuroda S, Kihara T, Akita Y et al (2020) Simulation and navigation of living donor hepatectomy using a unique three-dimensional printed liver model with soft and transparent parenchyma. Surg Today 50:307–313. https://doi.org/10.1007/s00595-019-01868-9
Sayed Aluwee SAZB, Zhou X, Kato H et al (2017) Evaluation of pre-surgical models for uterine surgery by use of three-dimensional printing and mold casting. Radiol Phys Technol 10:279–285. https://doi.org/10.1007/s12194-017-0397-2
Ye Z, Dun A, Jiang H et al (2020) The role of 3D printed models in the teaching of human anatomy: a systematic review and meta-analysis. BMC Med Educ 20:335. https://doi.org/10.1186/s12909-020-02242-x
Pan JJ, Chang J, Yang X et al (2011) Graphic and haptic simulation system for virtual laparoscopic rectum surgery. Int J Med Robot. https://doi.org/10.1002/rcs.399
Sui Y, Pan JJ, Qin H et al (2017) Real-time simulation of soft tissue deformation and electrocautery procedures in laparoscopic rectal cancer radical surgery. Int J Med Robot 13:e1827. https://doi.org/10.1002/rcs.1827
Acknowledgments
K.L. would like to acknowledge the financial support of the Australian Government through the professional practice research training scholarship program.
Funding
No other funding was received for the preparation of this manuscript. The material in the manuscript is the original work of the authors and has not been presented or submitted elsewhere for publication.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by G.T. and J.H. The first draft of the manuscript was written by G.T. and J.H. who contributed equally to this manuscript and should be considered joint first authors for this publication. All authors commented on previous versions of the manuscript and read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1: Search strategy
-
1.
3D.mp. [mp = ti, ab, hw, tn, ot, dm, mf, dv, kf, fx, dq, nm, ox, px, rx, an, ui, sy]
-
2.
Three-dimensional.mp. [mp = ti, ab, hw, tn, ot, dm, mf, dv, kf, fx, dq, nm, ox, px, rx, an, ui, sy]
-
3.
3D model.mp. [mp = ti, ab, hw, tn, ot, dm, mf, dv, kf, fx, dq, nm, ox, px, rx, an, ui, sy]
-
4.
Three-dimensional model.mp. [mp = ti, ab, hw, tn, ot, dm, mf, dv, kf, fx, dq, nm, ox, px, rx, an, ui, sy]
-
5.
Colorectal*.mp. [mp = ti, ab, hw, tn, ot, dm, mf, dv, kf, fx, dq, nm, ox, px, rx, an, ui, sy]
-
6.
Rectal*.mp. [mp = ti, ab, hw, tn, ot, dm, mf, dv, kf, fx, dq, nm, ox, px, rx, an, ui, sy]
-
7.
Surg*.mp. [mp = ti, ab, hw, tn, ot, dm, mf, dv, kf, fx, dq, nm, ox, px, rx, an, ui, sy]
-
8.
Teaching.mp. [mp = ti, ab, hw, tn, ot, dm, mf, dv, kf, fx, dq, nm, ox, px, rx, an, ui, sy]
-
9.
Education.mp. [mp = ti, ab, hw, tn, ot, dm, mf, dv, kf, fx, dq, nm, ox, px, rx, an, ui, sy]
-
10.
Sim*.mp. [mp = ti, ab, hw, tn, ot, dm, mf, dv, kf, fx, dq, nm, ox, px, rx, an, ui, sy]
-
11.
5 or 6
-
12.
7 and 11
-
13.
1 or 2 or 3 or 4
-
14.
8 or 9 or 10
-
15.
12 and 13 and 14
-
16.
Limit 15 to English language
-
17.
Limit 16 to yr = “1995-Current”
Web of Science: 667 records identified.
Medline + EMBASE: 570 records identified.
Appendix 2: Newcastle–Ottawa quality assessment scale for the included studies
No. | Criterion | Question | Score (* = 1, no * = 0) | ||||
|---|---|---|---|---|---|---|---|
Studies | Bangeas et al. (2019) | Chen et al. (2020) | Hojo et al. (2019) | Hojo et al. (2020) | Yiasemidou et al. (2021) | ||
Selection | |||||||
1 | Adequacy of case definition | a) Yes, with independent validation* b) Yes, e.g., record linkage or based on self-reports c) No description | a* | a* | a* | a* | a* |
2 | Representativeness of cases | a) Consecutive or obviously representative series of cases * b) Potential for selection biases or not stated | a* | a* | a* | a* | a* |
3 | Selection of controls | a) Community controls* b) Hospital controls c) No description | a* | a* | a* | c | a* |
4 | Definition of controls | a) No history of disease (endpoint)* b) No description of source | a* | a* | a* | a* | a* |
Comparability | |||||||
1 | Comparability of cases and controls on basis of design or analysis | a) Study controls for (select the most important factor)* b) Study controls for any additional factor* | a* | N/A | a* | N/A | a* |
Exposure | |||||||
1 | Ascertainment of exposure | a) Secure record (e.g. surgical records)* b) Structured interview where blind to case/control status* c) Interview not blinded to case/control status d) Written self-report or medical record only e) No description | c | c | c | c | c |
2 | Same method of ascertainment for cases and controls | a) Yes* b) No | a* | a* | a* | a* | a* |
3 | Non-response rate | a) Same rate for both groups* b) Non-respondents described c) Rate different and no designation | a* | a* | a* | a* | a* |
Score: | 7 | 6 | 7 | 5 | 7 | ||
Appendix 3: Preferred reporting items for systematic reviews and meta-analyses (PRISMA) diagram of article selection process

Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
To, G., Hawke, J.A., Larkins, K. et al. A systematic review of the application of 3D-printed models to colorectal surgical training. Tech Coloproctol 27, 257–270 (2023). https://doi.org/10.1007/s10151-023-02757-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-023-02757-7