Abstract
Background
Chronic anal fissure is one of the most common anorectal diseases and is associated with reduced quality of life. The aim of this study was to investigate the effects of pelvic floor physical therapy on quality of life in patients with chronic anal fissure using the Short-Form 36 Health Survey (RAND-36).
Methods
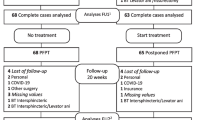
Adult patients, with chronic anal fissure and concomitant pelvic floor dysfunction, such as dyssynergia and increased pelvic floor muscle tone, were recruited at the Proctos Clinic in the Netherlands, between December 2018 and July 2021 and randomly assigned to an intervention group, receiving 8 weeks of pelvic floor physical therapy or assigned to a control group receiving postponed pelvic floor physical therapy (PAF trial). Quality of life and pain ratings were outcomes of the study and were measured at 8- and 20-week follow-up.
Results
One hundred patients (50 women and 50 men, median age 44.6 years [range 19–68 years]), completed the RAND-36 questionnaire and visual analog (VAS) pain scale score at admission. A significant improvement was found at 20-week follow-up in all domains of the RAND-36; physical functioning, pain, health change (p < 0.001); physical role, vitality, general health, social functioning, emotional role, mental health (p < 0.05). VAS pain was significantly reduced at 8 weeks (mean estimated difference 1.98; 95% CI 1.55–2.42, p < 0.001) and remained significant at 20-week follow-up (p < 0.001). The difference between the groups as regards change in the mean pain intensity scores at 8 weeks was 2.48 (95% CI − 3.20 to − 1.75; p < 0.001). Compared to the reference values of the general Dutch population, the patients in our study with a chronic anal fissure and pelvic floor dysfunction reported an impaired quality of life in 8 of 9 domains of the RAND-36. After treatment, significant lower scores were found in 2 out of 9 domains.
Conclusions
The results of this study provide evidence that treatment by pelvic floor physical therapy improves quality of life and reduces pain, making it an important tool in management of chronic anal fissure and concomitant pelvic floor dysfunction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic anal fissure (CAF) is a common proctological problem associated with reduced quality of life [1]. CAF is defined as a longitudinal ulcer in the squamous epithelium [2] and gives rise to distressing symptoms of pain and bleeding during and after defecation. The incidence of CAF is nearly 0.11% (1.1 cases per 1000 persons) and varies considerably according to age and sex [3]. Persistence of symptoms for long periods may lead to functional and psychosocial impairment [4], and seeking medical care is often delayed due to embarrassment [5]. Furthermore, in patients with CAF, there is a high degree of depression, anxiety and stress [1].
Health-related quality of life (QoL) can be influenced by physical, psychological and social factors, an individual’s life experience and general well-being [1, 6]. The purpose of health-related QoL evaluations is to move beyond clinical symptoms by examining how patients perceive and experience the impact on well-being and daily life [6, 7].
The most common generic instrument to measure QoL is the validated Medical Outcomes 36-Item Short-Form Health Survey (SF-36) used for decision-making for health care policies and clinical interventions [8]. Although there is a need to integrate aspects of functional and psychosocial impairment into medical care [9], only a few studies report on QoL in patients with CAF.
Recently, the Pelvic floor Anal Fissure study (PAF trial) was completed, which is a randomized controlled trial demonstrating the beneficial effects of pelvic floor physical therapy (PFPT) on an improvement of pelvic floor muscle tone and function, VAS pain scores, fissure healing and complaint reduction [10]. The aim of PFPT is to increase awareness and proprioception, to improve muscle relaxation, elasticity and function of the pelvic floor muscles, to restore abdominopelvic coordination, rectal sensitivity and reduce pain [11, 12].
In the PAF trial, we also hypothesized that treatment of PFPT will improve QoL. Here, we present the results of QoL measured with the Short-Form RAND-36 (RAND-36) [13] and visual analog scale (VAS) pain ratings in patients with CAF and pelvic floor dysfunction, who were included in the PAF trial. Furthermore, to better elucidate the results, the study compares baseline and post-treatment values with reference values of the RAND-36 of the general Dutch population [13].
Materials and methods
Study design
Quality of life was assessed with the RAND-36 in the PAF trial [14].
The PAF trial is a single-center, parallel, randomized controlled trial. The design involved allocation of all appropriate consecutive patients older than 18 years with CAF and pelvic floor dysfunction. Eligible patients were randomly assigned, after providing written informed consent to an intervention group receiving 8 weeks of PFPT or assigned to postponed PFPT (1:1 allocation).
Participants
Men and women aged 18 years or older presenting CAF and pelvic floor dysfunction were recruited by the surgeon at the Proctos Clinic in the Netherlands. CAF was defined as a longitudinal ulcer in the squamous epithelium with one or more signs of chronicity including hypertrophied anal papilla, sentinel tag and exposed internal sphincter muscle. Patients had fissure complaints of more than 6 weeks, and all patients failed in conservative treatment with fibers and/or laxatives and had applied the ointment (diltiazem or isosorbide di-nitrate) internally for at least 6 weeks. Pelvic floor dysfunction was defined by the presence of dyssynergia and/or increased pelvic floor muscle tone.
All patients had sufficient understanding of the Dutch language (reading and writing) and were able to complete the online questionnaires. Patients who were not able to undergo a digital rectal examination, patients with an abscess or fistula, Crohn’s disease or ulcerative colitis, anorectal malignancy, previous rectal or anal surgery, previous rectal radiation and pregnant patients were excluded from the trial.
Physical examination and questionnaires
The diagnosis of CAF was based on the patient’s medical history and a thorough local inspection of the anus. Resting anal sphincter pressure was measured by a careful digital rectal examination and scored as normal, weak (decreased), or increased [15]. Pelvic floor dysfunction was defined by the presence of dyssynergia and/or increased pelvic floor muscle tone. Pelvic floor muscle tone was measured with a digital rectal examination [16] and surface electromyography (μV) [16] with an intra-anal probe (Maple, ®Novuqare Pelvic Health B.V. CE 0344, Rosmalen, the Netherlands), which is validated for its purpose [17]. Pelvic floor dyssynergia was detected by digital rectal examination [18] and balloon expulsion test [19]. If necessary, proctoscopy was performed to exclude other pathology.
To access the impact of global QoL, the validated Dutch version of Short-Form RAND-36, Health Status Inventory, version 2 [13] was used. The RAND-36 consists of 36 items and 9 subscales: physical functioning, bodily pain, role limitation due to physical health problems, vitality, general health perception, social functioning, role limitation due to emotional problems, mental health, and health change perception. The RAND-36 consists of the same sets of items as the SF-36) [20], although the scoring procedure differs between the RAND-36 and SF-36 for the domains of general health and bodily pain. The score for each scale is obtained by the sum of the scores for each item linearly transformed into a range from 0 to 100. A higher score indicates more favorable QoL.
To quantify the average intensity of pain during defecation, a VAS from 0 (no pain) to 10 (most intense pain) was used [21]. Patients were requested to fill in the RAND-36 and VAS score at baseline, and at 8- and 20-week follow-up.
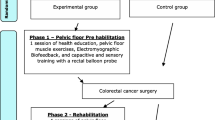
Interventions
At baseline, patients in both groups received information about the pelvic floor and related symptoms, explanation about relevant anatomy and defecation (patho)physiology, behavioral modifications and lifestyle advice. All patients continued their conservative measures including the use of ointment (diltiazem or isosorbide di-nitrate).
PFPT consisted of 5 face-to-face appointments of 45 min in a period of 8 consecutive weeks, using a treatment protocol. Details of this treatment protocol were described earlier [14]. Patients who were assigned to postponed PFPT did not receive additional treatment besides their conservative measures and the use of ointment until first follow-up at 8 weeks after inclusion. Patients from the postponed PFPT group followed the same treatment protocol after first follow-up.
Data collection of the RAND-36 was facilitated by a secure online system called Castor EDC [22]. Patients received the questionnaire by e-mail through the Castor system at 3 time points: at baseline, at 8- and 20-week follow-up.
Outcome measures
The primary outcome measure of this study was QoL in patients with CAF and pelvic floor dysfunction before and after PFPT and compared to reference values of the general Dutch population. The other outcome measure was the average pain intensity during defecation on a VAS-scale.
The sample size of the PAF-study was based on the primary endpoint, the tone at rest during electromyographic registration of the pelvic floor and consisted of 140 patients [14]. The data from the questionnaires that were at least 75% completed at baseline and follow-up were used for analysis.
Statistical analysis
Data were analyzed using Statistical Packages for Social Sciences (SPSS, Chicago, II, USA, version 28.0). Descriptive methods were used to assess quality of data, homogeneity of treatment groups and endpoints. Normality of the data was analyzed with histograms. Data are presented using mean (SD), median (range) for the numeric and non-normal variables and frequency (percentages) for categorical variables. A paired t test or Wilcoxon signed-rank test was used to compare continuous variables within groups. An independent T test or Mann–Whitney U test for quantitative data was performed to analyze statistical differences between groups. For each of the dimensions of the RAND-36, items scores were coded, summed and transformed on to a scale of 0–100. Statistical analyses consisted of estimating means and standard deviations for each of the RAND-36 scale scores. Comparison between groups for continuous variables was made by repeated measure analysis of variance using a mixed model after transformation of the data to enhance normality, with treatment, time (categorical) and their interaction as fixed effects and with random patient effects. To acquire an indication of the QoL of life of patients with CAF as compared to the reference group of the Dutch population, we calculated for each dimension the significance from the norm score [13] with the one-sample t test.
In case of missing data, we excluded that specific case from further analyses when less than 75% of the questionnaire was filled out. All p values were two-tailed, and statistical significance was taken as a p value of less than 0.05.
Results
Between December 2018 and July 2021, 140 patients were randomized to PFPT or postponed PFPT. After randomization, 3 patients withdrew.
The RAND-36 was adequately completed by 100 patients at baseline, of whom 50 women and 50 men with a median age of 44.6 years (range 19–68 years). The results from the questionnaires at baseline of 37 patients were excluded because less than 75% of the form had been completed.
The participants’ demographic and clinical characteristics of the total group of patients from the PAF-study, those who completed the baseline questionnaire adequately and individual treatment groups, are presented in Table 1. There were no significant differences in terms of demographic or clinical parameters between the groups at baseline (Table 1).
The non-response rate at 20-week follow-up was 31%. The results of the mean RAND-36 sub-scores from the different domains and the mean VAS pain scores, per time point from the total group and individual treatment groups, are presented in Table 2.
QoL pre- and post-treatment
For the group who adequately completed the questionnaire, the mean scores significantly improved in all domains of the RAND-36 from baseline to 20-week follow-up; physical functioning, bodily pain, health change (p < 0.001); physical role, vitality, general health, social functioning, emotional role and mental health (p < 0.05) (Table 2, Fig. 1).
QoL pre- and post-treatment for individual treatment groups
At 8-week follow-up, the PFPT group had significantly improved as regards bodily pain (p < 0.001), physical role, social functioning, mental health, and health change (p < 0.05) and the effect remained significant at 20-week follow-up. No significant improvement was found in vitality, general health and emotional role at 8- and 20-week follow-up (Table 2).
The postponed PFPT group significantly improved in the domains, bodily pain (p < 0.001), physical functioning, physical role, mental health, and health change (p < 0.05) at 8-week follow-up and remained significant at 20-week follow-up. At 20 weeks, the postponed group significantly improved in general health and emotional role (p < 0.05) post treatment. No significant improvements were found in the postponed group in the domain vitality and social functioning at this time point (Table 2).
According to the mean estimated difference between groups at 8-week follow-up, no significant differences were found in the different domains of the RAND-36 (Table 2).
Repeated measurement analysis showed more improvement in all domains in time from baseline to follow-up at 20 weeks in the PFPT group compared to postponed PFPT group although these differences were not significant (Fig. 2).
Pain
For the group as a whole, the VAS was significantly reduced from baseline to follow-up at 8 weeks (mean estimated difference 1.98; 95% CI 1.55–2.42, p < 0.001) and remained significant at 20-week follow-up (p < 0.001) (Table 2).
The VAS pain score was significantly reduced in both the PFPT and the postponed PFPT group at 8 weeks from baseline (p < 0.001). At 20-week follow-up, the VAS pain score in the PFPT group and postponed PFPT group further decreased and remained significant compared to baseline (p < 0.001). The difference between the groups as regards change in the mean pain intensity scores at 8 weeks from baseline was 2.48 (95% CI − 3.20 to − 1.75; p < 0.001) favoring the PFPT group. At 20 weeks, no significant mean difference in VAS scores was found between groups (p = 0.269).
QoL in the total group compared to the Dutch population
Compared to the reference group of the general Dutch population based on a mean age of 44 years [13], patients with CAF scored significantly lower on the subscales bodily pain, physical role, vitality, social functioning, mental health (p < 0.001) and general health, emotional role, and health change (p < 0.05). No significant difference was found in the domain physical functioning (p = 0.633) (Fig. 3).
Results showed that patients had higher post-treatment scores at 20-week follow-up compared to the Dutch reference values on physical functioning and health change (p < 0.001), but the scores in vitality and mental health were still significantly lower (p < 0.001). No significant difference was found between the whole groups compared to the normal Dutch population on the other domains at this time point.
Discussion
Health-related QoL measured by the RAND-36 significantly improved in all dimensions in all patients at 20-week follow-up and confirm the efficacy of PPFT on quality of life in patients with CAF from the PAF trial. The literature on the RAND-36 shows that very small differences in the range of 3–5 points on the survey could be interpreted as clinically important [23, 24]. In all domains of the RAND-36, the minimal clinical importance was higher than 3 points, which could be interpreted as indicating that the treatment was meaningful to the patient.
Furthermore, compared to the reference values of the general Dutch population, patients with CAF and pelvic floor dysfunction reported an impaired QoL in 8 of 9 domains of the RAND-36. After treatment, significantly lower scores were found in 2 out of 9 domains.
The positive effect of PFPT on QoL in patients with other anorectal complaints [25, 26] is already known but has never been investigated in patients with CAF.
In our study, the PFPT group significantly improved in 5 of 9 domains of the RAND-36 at 8-week follow-up. Interestingly, the postponed PFPT group also improved in 5 of 9 domains. An important aspect of treatment is re-education and improving understanding of defecation disorders [27]. It is likely that the information all patients receive about their complaints, instruction about toilet behavior and lifestyle advice also are reflected in an improvement in QoL in the postponed PFPT group, explaining our results.
Neither group improved in the domains, general health, vitality and emotional role at 8- and 20-week follow-up. One of the reasons could be that RAND-36 is not sensitive enough to pick up changes in these domains in a relatively short period of time (i.e., 20 weeks). More studies with a long-term follow-up are needed to confirm this.
In the domain bodily pain, all patients significantly improved post treatment compared to baseline. The same results were found for VAS pain scores. Reduction of pain is likely to have a positive reflection on QoL. Results from a study by Griffin et al. [4] in patients with CAF who were treated with topical ointment, confirm this assumption. Higher VAS pain scores were associated with worse outcome in all aspects of health-related QoL, with pain influencing many psychosocial and functional activities. A study by Tsunoda et al. [28] examining the treatment of CAF with diltiazem found that pain had a negative impact on the domains bodily pain and social functioning at baseline. Patients with healed fissures after treatment, reported an improvement in bodily pain, vitality, general health, and mental health. The PAF-study [10] found that the fissure was healed in 60% of all patients at 20-week follow-up. Significant lower scores were found in patients with non-healed fissures in the domains, bodily pain, social functioning, and emotional role at that time point. In a study by Bagul et al. [29] of patients with CAF who received Botulinum toxin injections, pain scores improved in 74% of the patients. QoL improved in patients in the domains of physical functioning, bodily pain, social functioning and mental health. The study demonstrated that pain was a significant factor influencing the outcome of QoL scores. Another study investigating Qol after lateral internal sphincterotomy in 58 patients [30] found improvement in pain symptoms although not all domains of health-related QoL were similarly positively affected. Smaller gains were reported among younger participants, women, participants with no comorbidities and those participants who waited the longest for their surgery.
Patients with CAF in our study scored lower overall than the reference group of the Dutch population. One of the reasons could be the chronicity of the problem. In our population, 65% of the patients had complaints for more than 6 months, which would have a negative influence on the patient, family members and other relations [31]. Other factors influencing the outcome of treatment should be investigated in further studies with a long-term follow-up.
The conclusions of this study are strengthened by the response rate of 71% at baseline, the high sample size and prospective design of the study. We enrolled patients of all ages and both sexes from different parts of the Netherlands. Thus, the results may be generalizable to the CAF population at large.
This study has some limitations. Currently, there is no disease-specific tool for assessing QoL in patients with CAF and therefore a generic instrument was used. The RAND-36 was chosen because it is one of the most used questionnaires measuring QoL, and it is translated in Dutch [13]. Its reliability has been proven in a post-rehabilitation Dutch population [32] but may not be specific enough to fully analyze the QoL in patients with CAF.
The non-response rate was 31% at 20-week follow-up. This may have caused bias if non-or partial respondents differ from respondents as concerns QoL or its determinants or confounders [33]. Reasons for non-completion at 20-week follow-up were surgery including Botulinum toxin, fissurectomy, fistulotomy, sclerodermy and other surgery (breastcancer). Other reasons were COVID-19, pregnancy, loss of follow-up for logistical reasons (distance, insurance, other) and personal. We did not find significant baseline differences between those followed up and those lost to follow-up.
Although the results show a significant improvement in a short period of time (e.g., 20 weeks), it is unknown what the long-term outcome of PFPT on QoL will be. In the PAF trial, patients also visited the clinic at 1-year follow-up. At the time of submitting this manuscript, the results of the 1-year follow-up were not completed. Hence, they could not be incorporated.
Conclusions
The results of this study provide evidence that PFPT is effective in the improvement of QoL and positively influences pain in patients with CAF and pelvic floor dysfunction Patients with CAF and concomitant pelvic floor dysfunction reported an impaired QoL compared to the reference values of the general population in the Netherlands.
References
Arısoy Ö, Şengül N, Çakir A (2016) Stress and psychopathology and its impact on quality of life in chronic anal fissure (CAF) patients. Int J Colorectal Dis 32(6):921–924. https://doi.org/10.1007/s00384-016-2732-1
Nelson RL (2014) Anal fissure (chronic). BMJ Clin Evid 2014:0407. https://www.ncbi.nlm.nih.gov/pubmed/25391392. Accesssed 12 Nov 2014
Mapel DW, Schum M, Von Worley A (2014) The epidemiology and treatment of anal fissures in a population-based cohort. BMC Gastroenterol 14:129. https://doi.org/10.1186/1471-230X-14-129
Griffin N, Acheson AG, Tung P, Sheard C, Glazebrook C, Scholefield JH (2004) Quality of life in patients with chronic anal fissure. Colorectal Dis 6(1):39–44. https://doi.org/10.1111/j.1463-1318.2004.00576.x
Gilani A, Tierney G (2022) Chronic anal fissure in adults. BMJ 376(1756–1833 (Electronic)):e066834. https://doi.org/10.1136/bmj-2021-066834
Glise H, Wiklund I (2002) Health-related quality of life and gastrointestinal disease. J Gastroenterol Hepatol 17(Suppl no. 0815-9319 (Print)):S72-84. https://doi.org/10.1046/j.1440-1746.17.s1.6.x
Fitzpatrick R, Fletcher A, Gore S, Jones D, Spiegelhalter D, Cox D (1992) Quality of life measures in health care. I: Applications and issues in assessment, (in eng). BMJ 305(6861):1074–1077. https://doi.org/10.1136/bmj.305.6861.1074
Nilsson E, Kristenson M (2010) Psychological factors related to physical, social, and mental dimensions of the SF-36: a population-based study of middle-aged women and men. Patient Relat Outcome Meas 1(1179–271X (Print)):153–162. https://doi.org/10.2147/PROM.S13209
Mentes BB, Tezcaner T, Yilmaz U, Leventoglu S, Oguz M (2006) Results of lateral internal sphincterotomy for chronic anal fissure with particular reference to quality of life. Dis Colon Rectum 49(7):1045–1051. https://doi.org/10.1007/s10350-006-0527-0
van Reijn-Baggen DA, Elzevier HW, Putter H, Pelger RCM, Han-Geurts IJM (2022) Pelvic floor physical therapy in patients with chronic anal fissure: a randomized controlled trial. Tech Coloproctol 26(7):571–582. https://doi.org/10.1007/s10151-022-02618-9
van Reijn-Baggen DA, Han-Geurts IJM, Voorham-van der Zalm PJ, Pelger RCM, Hagenaars-van Miert C, Laan ETM (2022) Pelvic floor physical therapy for pelvic floor hypertonicity: a systematic review of treatment efficacy. Sex Med Rev 10(2):209–230. https://doi.org/10.1016/j.sxmr.2021.03.002
Bocchini R et al (2019) Pelvic floor rehabilitation for defecation disorders. Tech Coloproctol 23(2):101–115. https://doi.org/10.1007/s10151-018-1921-z
VanderZee KI, Sanderman R, Heyink JW, de Haes H (1996) Psychometric qualities of the RAND 36-Item Health Survey 1.0: a multidimensional measure of general health status. Int J Behav Med 3(2):104–122. https://doi.org/10.1207/s15327558ijbm0302_2
van Reijn-Baggen DA, Elzevier HW, Pelger RCM, Han-Geurts IJM (2021) Pelvic floor physical therapy in the treatment of chronic anal fissure (PAF-study): Study protocol for a randomized controlled trial. Contemp Clin Trials Commun 24(2451–8654 (Electronic)):100874. https://doi.org/10.1016/j.conctc.2021.100874
Rao SSC (2018) Rectal exam: yes, it can and should be done in a busy practice! Am J Gastroenterol 113(5):635–638. https://doi.org/10.1038/s41395-018-0006-y
Frawley H et al (2021) An International Continence Society (ICS) report on the terminology for pelvic floor muscle assessment. Neurourol Urodyn 40(5):1217–1260. https://doi.org/10.1002/nau.24658
Voorham-van der Zalm PJ et al (2013) Reliability and differentiation of pelvic floor muscle electromyography measurements in healthy volunteers using a new device: the Multiple Array Probe Leiden (MAPLe). Neurourol Urodyn 32(4):341–348
Tantiphlachiva K, Rao A, Fau-Attaluri P, Attaluri SSC, Fau-Rao A, Rao SS (2010) Digital rectal examination is a useful tool for identifying patients with dyssynergia, (in eng). Clin Gastroenterol Hepatol 8(11):955–960
Chiarioni G, Kim SM, Vantini I, Whitehead WE (2014) Validation of the balloon evacuation test: reproducibility and agreement with findings from anorectal manometry and electromyography. Clin Gastroenterol Hepatol 12(12):2049–2054. https://doi.org/10.1016/j.cgh.2014.03.013
The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection Med Care. 1992 Jun;30(6):473-83.
Dworkin RH et al (2008) Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain 9(2):105–121. https://doi.org/10.1016/j.jpain.2007.09.005
Castor Electronic Data Capture (EDC):https://www.castoredc.com.
Samsa G, Edelman D, Rothman ML, Williams GR, Lipscomb J, Matchar D (1999) Determining clinically important differences in health status measures: a general approach with illustration to the health utilities index mark II. Pharmacoeconomics 15(2):141–155. https://doi.org/10.2165/00019053-199915020-00003
Hays RD, Morales LS (2001) The RAND-36 measure of health-related quality of life. Ann Med 33(5):350–357. https://doi.org/10.3109/07853890109002089
Bartlett L, Sloots K, Nowak M, Ho YH (2015) Supplementary home biofeedback improves quality of life in younger patients with fecal incontinence. J Clin Gastroenterol 49(5):419–428. https://doi.org/10.1097/MCG.0000000000000143
Cadeddu F, Salis F, De Luca E, Ciangola I, Milito G (2015) Efficacy of biofeedback plus transanal stimulation in the management of pelvic floor dyssynergia: a randomized trial. Tech Coloproctol 19(6):333–338. https://doi.org/10.1007/s10151-015-1292-7
Beaty JS, Shashidharan M (2016) Anal Fissure, (in eng). Clin Colon Rectal Surg 29(1):30–37. https://doi.org/10.1055/s-0035-1570390
Tsunoda A, Kashiwagura Y, Hirose K, Sasaki T, Kano N (2012) Quality of life in patients with chronic anal fissure after topical treatment with diltiazem, (in eng). World J Gastrointest Surg 4(11):251–255. https://doi.org/10.4240/wjgs.v4.i11.251
Bagul A, Carter P (2019) Quality of life in patients receiving botulinum a toxin treatment for symptomatic anal fissure. World J Surg Surgical Res 2:1130
Sutherland JA-O et al (2020) Health and quality of life among a cohort of patients having lateral internal sphincterotomy for anal fissures, (in eng). Colorectal Dis 22(1463–1318 (Electronic)):1658–1666
Navarro-Sánchez A et al (2021) Sexuality, quality of life, anxiety, depression, and anger in patients with anal fissure a case-control study. LID. https://doi.org/10.3390/jcm10194401
Krops LA, Wolthuizen L, Dijkstra PU, Jaarsma EA, Geertzen JHB, Dekker R (2018) Reliability of translation of the RAND 36-item health survey in a post-rehabilitation population, (in eng). Int J Rehabil Res 41(2):128–137. https://doi.org/10.1097/MRR.0000000000000265
Coste J, Quinquis E, Fau-Audureau L, Audureau J, Fau-Pouchot E, Pouchot J (2013) Non response, incomplete and inconsistent responses to self-administered health-related quality of life measures in the general population: patterns, determinants and impact on the validity of estimates - a population-based study in France using the MOS SF-36. Health Qual Life Outcomes. 2013 Mar 13;11:44. https://doi.org/10.1186/1477-7525-11-44.
Funding
No funding of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have neither competing interests nor conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
van Reijn-Baggen, D.A., Elzevier, H.W., Braak, J.P.B.M. et al. Pelvic floor physical therapy in the treatment of chronic anal fissure (PAF trial): quality of life outcome. Tech Coloproctol 27, 125–133 (2023). https://doi.org/10.1007/s10151-022-02741-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-022-02741-7