Abstract
Background
A randomized controlled trial showed that patients with grade III or IV internal hemorrhoids had similar symptomatic relief of symptoms up to 3 months following dearterialization with mucopexy or hemorrhoidectomy albeit with less postoperative pain after the former. This study aimed to compare hemorrhoidal recurrence and chronic complications at 3-year follow-up.
Methods
This study was carried out on 40 patients with grade III or IV internal hemorrhoids previously enrolled to a randomized trial comparing dearterialization to hemorrhoidectomy. Recurrence was defined as internal hemorrhoids diagnosed on proctoscopy. Chronic complications were nonresolving adverse events related to surgery. Outcome measures included patient-reported outcomes and quality of life measured by brief pain inventory (BPI), SF-12, and fecal incontinence surveys.
Results
At median follow-up of 36 (27–43) months, 13 patients (32.5 %) were lost to follow-up. Patient-reported outcomes suggested no difference between dearterialization and hemorrhoidectomy in persistent symptoms, occurring in 1 (8.3 %) vs. 2 (13.3 %) patients (p = 0.681) and in symptom recurrence, occurring in 6 (50 %) vs. 4 (26.7 %) patients (p = 0.212). On proctoscopy, recurrence was seen in 2 (13.3 %) vs. 1 (6.7 %) patients (p = 0.411), all with index grade IV disease. One patient in each arm required reoperation (p = 0.869). Chronic complications were not seen in the dearterialization arm while they occurred in 2 (13.3 %) hemorrhoidectomy patients (p = 0.189) and included unhealed wound (n = 1), anal fissure (n = 1) and fecal incontinence (n = 1). There was a trend toward more patient reported than actual recurrence on proctoscopy (10 vs. 3, p = 0.259). There was no difference in BPI, SF-12, and fecal incontinence quality of life scores.
Conclusions
Recurrence rates did not differ significantly at 3-year follow-up and occurred in patients with index grade IV hemorrhoids. Chronic complications occurred only after hemorrhoidectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hemorrhoidal artery dearterialization was first described as a treatment for internal hemorrhoids in 1995 by Morinaga [1] and has been popularized over the last decade with the development of specialized anoscopes, which facilitate this procedure. However, there is still controversy and skepticism surrounding this procedure as an alternative to hemorrhoidectomy or stapled hemorrhoidopexy. While there is a sufficient short-term data in the surgical literature, long-term data and randomized data are lacking. While three quadrant excisional hemorrhoidectomy is considered the gold standard procedure for advanced hemorrhoidal disease, it is not a perfect operation. There is a significant pain and morbidity in the short term, and recurrence and chronic complications are reported in the long term. A British study with 17-year follow-up reported 26 % recurrence of hemorrhoids after excisional hemorrhoidectomy [2], and another study with median of 7-year follow-up reported that 40 % of patients complained of recurrent symptoms and 4 % developed anal strictures [3]. In 2013, we published the short-term results of a randomized controlled study treating grade III and IV internal hemorrhoids with either hemorrhoidal dearterialization with mucopexy or Ferguson hemorrhoidectomy [4]. The study found less postoperative pain in the dearterialization patients and similar resolution of preoperative symptoms with up to 3-month follow-up. The aim of this study is to report and characterize the long-term results of these two techniques.
Methods
Study design
This was a follow-up study performed by telephone survey of patients who underwent either hemorrhoidal dearterialization with mucopexy or excisional hemorrhoidectomy as part of a randomized double-blinded trial [4]. All the patients included in the study had grade III or IV internal hemorrhoids in a minimum of three quadrants. Grade III internal hemorrhoids prolapse but are reducible and grade IV internal hemorrhoids prolapse and are not reducible by the patient or do not remain reduced [5]. Diagnosis was established by examination and anoscopy or proctoscopy by a colorectal surgeon. As patients often present with anorectal symptoms, which may be due to causes other than internal hemorrhoids, only patients who were symptomatic and were found to have grade III or IV internal hemorrhoids on examination were included in the study. This assured a reproducible patient population. Patients were excluded if they had undergone surgery for hemorrhoids previously. The procedures were performed under general anesthesia or intravenous sedation with local anesthetic infiltration, in the ambulatory surgery setting. Hemorrhoidal dearterialization with mucopexy was performed using the THD kit (THD Italy, Corregio, Italy). The surgical technique involves identifying six hemorrhoidal arteries by Doppler guidance and suture ligating each one separately with a 2–0 absorbable suture. The same suture is then used to perform the mucopexy up to 1 cm proximal to dentate line. This technique was described by Ratto et al. [6]. The hemorrhoidectomy was performed as described by Ferguson and Heaton [7]. Each hemorrhoid was excised by an elliptical incision under exposure by an anal retractor. The incision was extended cephalad. The hemorrhoidal pedicle was suture ligated, and the incision was closed primarily. Patients were all discharged to home on the same day, with a prescription for hydrocodone or oxycodone and instructions to use stool softeners, water baths, and laxatives. They were seen 2 weeks after surgery and followed routinely up to 3 months. Following that period, they were seen on an as needed basis.
Institutional review board approval was obtained for this study. Patients were contacted by telephone and asked to participate in the survey. The telephone surveys were conducted by a blinded research assistant, who also reviewed the chart for additional data. Patients who reported continued or recurrent anal symptoms were asked to return to the office for examination by the surgeon.
Study endpoints
The primary endpoint for this study was rate of recurrence of internal hemorrhoids. Recurrence was defined as internal hemorrhoids seen by the colorectal surgeon on anoscopic or proctoscopic examination in patients who were symptomatic. Additional endpoints examined included chronic complications, need for reoperations, and patient-reported outcomes such as anal pain, anal bleeding, other anal symptoms, current level of pain, level of fecal continence, and overall quality of life. Chronic complications included anal stenosis, unhealed wounds, and anal fissures persistent since surgery, and fecal incontinence developing immediately after surgery. Current level of pain was measured using the brief pain inventory (BPI), which is a validated pain assessment tool based on the Wisconsin Brief Pain questionnaire [8–10]. Fecal continence was measured using the Fecal Incontinence Quality of Life tool [11]. Overall quality of life was measured using the SF-12 tool [12].
Statistical methods
Patient data were entered into a Microsoft Excel© spreadsheet. SPSS© software was used to analyze the data. Pearson’s chi-squared test was used for categorical data, and Student’s t test was used for continuous data. Significance was predetermined at α = 0.05.
Results
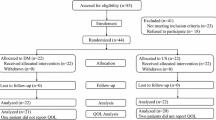
Of the original 40 patients, 12 were lost to follow-up and 1 dearterialization patient refused to participate, resulting in a 68 % retention rate. A total of 12 dearterialization patients and 15 hemorrhoidectomy patients were included in the study. The median follow-up was 35 months (range 27–43). The two arms of patients had similar demographics except for gender distribution (42 vs. 94 % male, p = 0.003). Demographics are summarized in Table 1.
All of the patients who reported recurrent or persistent anorectal symptoms on the telephone survey returned to the office for examination. Recurrence of internal hemorrhoids was found on physician examination in two dearterialization patients and one hemorrhoidectomy patient (16.7 vs. 6.7 %, p = 0.411). One dearterialization patient was found to have a single grade III internal hemorrhoid, which was treated with repeat dearterialization, and the other patient had recurrent grade IV hemorrhoids and opted for nonoperative management with stool softener and fiber supplementation. The patient who recurred after hemorrhoidectomy was found to have grade IV hemorrhoids and was treated with repeat hemorrhoidectomy. This patient had three very large prolapsing hemorrhoids at the index operation. On examination at the time of recurrence, he again had three large prolapsing hemorrhoids and significant bleeding requiring blood transfusion. These results are summarized in Table 2. All three patients who had a recurrence had grade IV internal hemorrhoids prior to the index surgery. Additional findings reported on physician examination were external residual skin tags in five dearterialization patients and one hemorrhoidectomy patient. Chronic complications were reported in no dearterialization patients and two hemorrhoidectomy patients (Table 3). These included an unhealed wound in one patient and a fissure and fecal incontinence in another.
In the telephone survey results, one dearterialization patient and two hemorrhoidectomy patients reported that the symptoms for which they had surgery never resolved (p = 0.681). Six dearterialization patients and four hemorrhoidectomy patients reported recurrent symptoms, including anal pain, bleeding, and itching (p = 0.212). (Table 4) These symptoms were treated with stool softeners, fiber supplements, warm water baths, and ointments, or suppositories. Interestingly, there was a difference between patient-reported recurrent symptoms (10) and actual confirmation of recurrent internal hemorrhoids (3) by a physician (p = 0.259), though it was not statistically significant.
The BPI was used to assess current pain in the patients. Results were similar in both pain severity (p = 0.481) and interference in lifestyle due to pain (p = 0.259) between the two arms. Quality of life was assessed both in terms of overall quality (SF-12) and in terms of incontinence (FIQOL). In both scales, the quality of life results were similar in both arms of the study. Results are summarized in Table 5.
Discussion
The gold standard surgical treatment for hemorrhoids is excisional hemorrhoidectomy. While this method seems to have the best long-term result in terms of recurrence of disease, it has several drawbacks. These include significant postoperative pain, bleeding, constipation, urinary retention, and long-term complications such as anal stenosis, nonhealing wounds, residual skin tags, and anal incontinence. Surgeons have developed several less invasive procedures in the search for a balance between acceptable relief of symptoms and less postoperative pain and other complications. As with all new procedures, long-term results take years to study, and the technology often becomes accepted into practice without knowing how the procedure will hold up to the test of time.
Hemorrhoidal artery dearterialization was described two decades ago, but did not become popular until more recently; therefore, long-term results are not widely available. Additionally, many different terms are used to describe essentially the same procedure in the literature. In order to identify studies reporting on this procedure, one must use multiple terms, including combinations of “transanal hemorrhoidal dearterialization (THD),” “Doppler-guided hemorrhoidal artery ligation (DGHAL),” “mucopexy,” “anopexy,” “suture mucosal pexy,” and “rectoanal repair.” Randomized trials or even comparative studies such as case–control retrospective series are rarely available.
Zampieri et al. [13] reported in 2012 on a randomized trial studying transanal hemorrhoidal dearterialization with proctopexy and ligasure hemorrhoidectomy. The study included 114 patients, and follow-up was 1 year. Follow-up was conducted by telephone interview. Patients included had at least grade III internal hemorrhoids. The primary-reported outcome was resolution of pain. At 6 months, THD patients had statistically significantly less pain than hemorrhoidectomy patients, but at 1 year, pain was similar between the two groups. Recurrence of internal hemorrhoids was not reported.
Another researcher randomized 40 patients to either THD with anopexy or hemorrhoidectomy [14]. All patients had grade II or III internal hemorrhoids. At 1-year follow-up, two patients who underwent THD had remaining grade III hemorrhoids and seven patients had grade II hemorrhoids, and one patient who underwent hemorrhoidectomy had remaining grade III hemorrhoids and three patients had Grade II hemorrhoids. This difference in residual hemorrhoids was not statistically significant between the groups.
Infantino et al. [15] randomized 167 patients to receive either stapled hemorrhoidopexy (PPH) or THD. All patients had grade III internal hemorrhoids. The authors report similar short-term complications, with long-term complications occurring only in the PPH group. They report persistence or recurrence of internal hemorrhoids in 14 % of THD patients and 7 % of PPH patients, which was not a statistically significant difference. The mean follow-up was 17 months.
Avital et al. [16] reported 5-year follow-up on 100 patients who underwent DGHAL without mucopexy by a single surgeon for grade II and III internal hemorrhoids. Ninety-six patients answered the survey at 1 year and 92 at 5 years. In total, 89 % were asymptomatic at 1 year and 73 % at 5 years. They found that most recurrences occurred during the first year after surgery, and there was a trend toward more recurrence in patients with grade III internal hemorrhoids.
Faucheron et al. [17] reported long-term results of 100 patients with grade IV internal hemorrhoids who underwent DGHAL with rectoanal repair. The patients were prospectively followed for a mean of 34 months. In total, 9 % had a recurrence of hemorrhoidal prolapse at 11 months. Treatment for recurrence included repeat DGHAL in three patients, hemorrhoidectomy in three patients, and nonoperative management in the other three patients.
De Nardi et al. [18] recently reported a randomized trial of 50 patients with grade III internal hemorrhoids who underwent either THD with mucopexy or hemorrhoidectomy. The study period was up to 24 months. The authors noted less pain in the THD arm in the first postoperative week, but no difference in pain thereafter. Regarding recurrent symptoms, both techniques were equivalent after 2 years of follow-up.
In this study, we report long-term results of a randomized trial of patients with grade III or IV internal hemorrhoids who underwent either transanal hemorrhoidal dearterialization (THD) with mucopexy or three quadrant excisional hemorrhoidectomy and were followed for a median of 35 months. The recurrence of internal hemorrhoids did not differ significantly between the two groups. Additionally, all the patients who recurred in both arms had grade IV internal hemorrhoids at the time of the index operation. Long-term complications, including unhealed wounds, fissures, and incontinence, were only found in patients who underwent hemorrhoidectomy, though this difference was not statistically significant. The patients themselves reported similar numbers of symptoms and recurrence in both arms, and quality of life and pain scores were similar in both arms as well.
This study has several weaknesses. We lost 13 patients from follow-up, which leads to lower numbers and selection bias. This is an unfortunate consequence of our patient population, which tends to change address or phone numbers frequently when compared to some European populations. However, this reflects the real-life scenario of any long-term follow-up study in the USA. The demographics of the patients were similar in both arms except for gender distribution. Additionally, there were no changes in surgical technique during the study period, and the two surgeons involved performed both operations during the entire period of time. As with any long-term study, the patients themselves choose whether to participate in the survey or not, so this may lead to some selection or reporting bias. This may lead to over or under reporting of recurrences or complications depending on which patients choose to answer the questions. The total number of patients was small, so it is possible that in a larger patient population, the difference in recurrence of hemorrhoids would have been statistically significant. However, the number of patients included is similar to other two-arm studies.
However, the study has significant strengths. We compared two surgical treatments for hemorrhoids. We had strict definitions of the severity of disease being treated, as well as definitions of complications. We used validated means of collecting patient-reported outcomes, such as the BPI, SF-12 scale, and FIQOL questionnaire. The length of the follow-up period is almost 3 years, which makes this one of the longer studies reporting on hemorrhoidal dearterialization in the literature. As reported in several other studies, most recurrences occur within the first postoperative year, so it is safe to assume that 3-year follow-up is an adequate measure of success for this technique.
In conclusion, this study suggests that hemorrhoidal dearterialization with suture mucopexy is as good as hemorrhoidectomy in the longer term, both in terms of actual recurrence of internal hemorrhoids and in terms of patient satisfaction. It may be more appropriate for grade III internal hemorrhoids, but may successfully be used in grade IV disease as well. In addition, dearterialization is a safe procedure, which not only provides less postoperative pain in the short term, but also enjoys a low occurrence of chronic complications.
References
Morinaga K, Hasuda K, Ikeda T (1995) A novel therapy for internal hemorrhoids: ligation of the hemorrhoidal artery with a newly devised instrument (Moricorn) in conjunction with a Doppler flowmeter. Am J Gastroenterol 90:610–613
Konsten J, Baeten CG (2000) Hemorrhoidectomy vs. Lord’s method: 17-year follow-up of a prospective, randomized trial. Dis Colon Rectum 43:503–506
Qarabaki MA, Mukhashavria GA, Mukhashavria GG, Giorgadze NG (2014) Circular vs. three-quadrant hemorrhoidectomy for end-stage hemorrhoids: short- and long-term outcomes of a prospective randomized trial. J Gastrointest Surg 18:808–815
Denoya PI, Fakhoury M, Chang K, Fakhoury J, Bergamaschi R (2013) Dearterialization with mucopexy versus haemorrhoidectomy for grade III or IV haemorrhoids: short-term results of a double-blind randomized controlled trial. Colorectal Dis 15:1281–1288
Corman ML (2013) Corman’s colon and rectal surgery. In: Editor (ed) Book corman’s colon and rectal surgery, 6 edn. City: Lippincott Williams & Wilkins, p 1564
Ratto C, Giordano P, Donisi L, Parello A, Litta F, Doglietto GB (2011) Transanal haemorrhoidal dearterialization (THD) for selected fourth-degree haemorrhoids. Tech Coloproctol 15:191–197
Ferguson JA, Heaton JR (1959) Closed hemorrhoidectomy. Dis Colon Rectum 2:176–179
Keller S, Bann CM, Dodd SL, Schein J, Mendoza TR, Cleeland CS (2004) Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain. Clin J Pain 20:309–318
Tan G, Jensen MP, Thornby JI, Shanti BF (2004) Validation of the brief pain inventory for chronic nonmalignant pain. J Pain 5:133–137
Daut RL, Cleeland CS, Flanery RC (1983) Development of the Wisconsin Brief Pain Questionnaire to assess pain in cancer and other diseases. Pain 17:197–210
Rockwood TH, Church JM, Fleshman JW et al (2000) Fecal Incontinence Quality of Life Scale: quality of life instrument for patients with fecal incontinence. Dis Colon Rectum 43:9–16; discussion 16-17
Ware JE Jr (2000) SF-36 health survey update. Spine (Phila Pa 1976) 25:3130–3139
Zampieri N, Castellani R, Andreoli R, Geccherle A (2012) Long-term results and quality of life in patients treated with hemorrhoidectomy using two different techniques: ligasure versus transanal hemorrhoidal dearterialization. Am J Surg 204:684–688
Elmer SE, Nygren JO, Lenander CE (2013) A randomized trial of transanal hemorrhoidal dearterialization with anopexy compared with open hemorrhoidectomy in the treatment of hemorrhoids. Dis Colon Rectum 56:484–490
Infantino A, Altomare DF, Bottini C et al (2012) Prospective randomized multicentre study comparing stapler haemorrhoidopexy with Doppler-guided transanal haemorrhoid dearterialization for third-degree haemorrhoids. Colorectal Dis 14:205–211
Avital S, Inbar R, Karin E, Greenberg R (2012) Five-year follow-up of Doppler-guided hemorrhoidal artery ligation. Tech Coloproctol 16:61–65
Faucheron JL, Poncet G, Voirin D, Badic B, Gangner Y (2011) Doppler-guided hemorrhoidal artery ligation and rectoanal repair (HAL-RAR) for the treatment of grade IV hemorrhoids: long-term results in 100 consecutive patients. Dis Colon Rectum 54:226–231
De Nardi P, Capretti G, Corsaro A, Staudacher C (2014) A prospective, randomized trial comparing the short- and long-term results of doppler-guided transanal hemorrhoid dearterialization with mucopexy versus excision hemorrhoidectomy for grade III hemorrhoids. Dis Colon Rectum 57:348–353
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Denoya, P., Tam, J. & Bergamaschi, R. Hemorrhoidal dearterialization with mucopexy versus hemorrhoidectomy: 3-year follow-up assessment of a randomized controlled trial. Tech Coloproctol 18, 1081–1085 (2014). https://doi.org/10.1007/s10151-014-1219-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-014-1219-8