Abstract
Background
Cancer of unknown primary site (CUP) is a heterogeneous group of tumors for which the origin remains unknown. Clinical outcomes might be influenced by regulatory processes in its microenvironment. Microsatellite instability (MSI) is a predictive biomarker for cancer immunotherapy and its status, as well as co-occurrence with PD-L1 expression, is poorly evaluated. We aim to evaluate the expression of PD-L1 and the status of MSI in CUP and their possible associations with clinical–pathological features.
Methods
The combined positive score (CPS) PD-L1 expression was evaluated by immunohistochemistry. MSI status was assessed using a hexa-plex marker panel by polymerase chain reaction followed by fragment analysis.
Results
Among the 166 cases, MSI analysis was conclusive in 120, with two cases being MSI positive (1.6%). PD-L1 expression was positive in 18.3% of 109 feasible cases. PD-L1 expression was significantly associated with non-visceral metastasis and a dominance of nodal metastasis. The median overall survival (mOS) was 3.7 (95% CI 1.6–5.8) months and patients who expressed PD-L1 achieved a better mOS compared to those who did not express PD-L1 (18.7 versus 3.0 months, p-value: < .001). ECOG-PS equal to or more than two and PD-L1 expression were independent prognostic factors in multivariate analysis (2.37 and 0.42, respectively).
Conclusion
PD-L1 is expressed in a subset (1/5) of patients with CUP and associated with improved overall survival, while MSI is a rare event. There is a need to explore better the tumor microenvironment as well as the role of immunotherapy to change such a bad clinical outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer of unknown primary site (CUP) is a group of malignant neoplasms diagnosed by biopsy of metastasis, but with no primary cancer identified after a comprehensive clinical and radiological assessment [1, 2]. They account for 3% up to 5% of the most common tumors in developed countries, and the average diagnosis is at 60 years old, with a similar incidence between men and women [2]. Five histological subtypes are frequently identified, and the large majority are adenocarcinomas, mainly well or moderately differentiated [2]. Immunohistochemistry is a fundamental part of the diagnosis workup, yet it can fail to define the precise origin of the tumor [3, 4]. Moreover, even new image resources such as FDG-PET/CT (Fluorodeoxyglucose positron emission tomography computed tomography) lack better sensitivity and specificity to detect the primary site [5].
Chromosome abnormalities and overexpression of genes such as EGFR, Kit/PDGFR, RAS, BCL2, and ERBB2 are described in CUPs [6, 7]. CUPs have substantial mutational heterogeneity. TP53, MUC16, KRAS, LRP1B and CSMD3 are the most frequently mutated genes, along with FGFR2 being the most common gene involved in fusion events [8]. In the last decade, genomic profiling has been assessed to define the histology of the primary site, and druggable molecular targets have been described [9,10,11]. There are several molecular signatures to predict the tissue of origin in CUPs with variable accuracy, but yet some uncertainties of their benefits exist in routine clinical use [12, 13].
A wide variety of clinical presentations might be noted in patients with CUPs, and their biological behavior is commonly aggressive and somehow unpredictable, leading to a worse prognosis [14]. There is no standard treatment regimen, but some benefits in response rate and survival can be observed from taxane- or platin-based chemotherapy [15, 16].
The immune checkpoint molecule programmed death-1 (PD-1) plays a role in self–nonself discrimination by the immune system [17]. PD-1 expression is high on T cells in the tumor microenvironment, and its primary ligand, PD-L1, is variably expressed on tumor cells and antigen-presenting cells within tumors, providing a potent inhibitory effect within the tumor microenvironment [18]. In the last decade, immune checkpoint inhibitors, such as anti-PD-1 or anti-PD-L1 drugs, have been largely explored as a therapeutic strategy in oncology [19, 20]. Microsatellite instability (MSI) is a marker of genetic instability, mainly due to epigenetic or genetic silencing of mismatch repair pathway genes [21]. Based on the significative overall response rate, FDA approved pembrolizumab (anti-PD-1) to treat patients, in an agnostic way, whose solid tumor harbors mismatch repair deficiency [22]. The PD-L1 expression and the presence of MSI in the CUP microenvironment have been underexplored.
Herein, we aim to explore the expression of PD-L1 and the frequency of MSI in a representative cohort of CUP.
Patients and methods
Study population and selection of cases
We identified 166 cases of CUP patients who presented to Barretos Cancer Hospital between 2002 and 2016. Clinical–pathological features were retrieved from the medical records and collected using REDCap electronic data capture tool [23]. All included patients underwent immunohistochemistry in accordance with appropriate diagnostic guidelines and immunohistochemical analysis and the results failed to define the primary site [24]. All men underwent thorough image tests with no diagnosis of primary site. All patients included had been tested for prostate-specific antigen (PSA) and human chorionic gonadotropin (HCG) in cases of undifferentiated carcinoma. We excluded patients with exclusive head and neck squamous cell carcinoma in the lymph nodes, women with exclusive axillary adenocarcinoma in the lymph nodes or peritoneum involvement of adenocarcinoma, and midline tumors in young adults. Histology such as neuroendocrine tumors, melanoma, and small-cell tumors were excluded, as well as patients with chronic immunosuppression history.
This study was approved by the local IRB under Protocol No. 1055/2015.
PD-L1 Immunohistochemistry
The immunohistochemistry reaction was performed using BenchMark Ventana Ultra™ (Ventana, Tucson, AZ, USA) platform, through multimer linked to horse radish peroxidase, to detect PD-L1 protein, as previously reported [25]. The anti-PD-L1 (E1L3N®) XP® Rabbit mAb, Cell Signaling Technology, was used as primary antibody and we used the OptiView DAB IHC Detection Kit, following manufacturer’s guidelines. Placental syncytiotrophoblast was used as positive control tissue. The combined positive score (CPS) was used to measure the expression of PD-L1. CPS corresponds to the ratio between the total of PD-L1 positive cells (tumor cell, lymphocytes and macrophages) and the total of viable tumor cells, multiplied by 100 [26]. Considering the experience of appropriateness of CPS cutoff in other types of tumors and no agreement of CPS cutoff for CUPs, we used CPS ≥ 1 in our study [27].
DNA isolation and microsatellite instability (MSI) assay
Tumor DNA was isolated from FFPE sections using QIAamp DNA Micro Kit (Qiagen, Germany), as previously reported [28]. Briefly, the MSI assay was performed using HT-MSI + kit (Cellco, São Carlos, Brazil) composed of six quasi-monomorphic mononucleotide repeat markers (NR27, NR21, NR24, BAT25, BAT26, and HSP110), following the manufacturer’s guideline. The analysis was performed using 3500 Genetic Analyzer automated sequencer (Applied Biosystems, USA) and analyzed by the GeneMapper software (Applied Biosystems, USA), according to manufacturer's recommendations. Cases with the presence of two or more markers out of the quasimonomorphic variation range (QMVR) were classified as MSI positive (MSI +), and cases without markers out of QMVR were classified as MSI negative (MSI −).
Statistical analysis
Univariate analysis was used to associate sample variables in relation to PD-L1 expression, using the χ2 test or Fisher’s exact test, according to the characteristics of the sample. Survival curves were plotted using the Kaplan–Meier method and the event of interest (death) was considered for the outcome of overall survival (OS). Alive patients and those lost to follow-up were censored. Univariate and multivariate analysis were performed using Cox regression method. Statistical analyses were performed using IBM SPSS Statistics for Mac OS, Version 2.0 (IBM). P values < 0.05 were considered statistically significant.
Results
Clinical–pathological characterization of CUP patients
One hundred and sixty-six cases of CUPs were identified according to selection criteria (Table 1). The mean age was around 60 years, and gender, tobacco exposure, and cancer family history did not correlate with PDL1 status. Most patients were non-alcohol drinkers and were diagnosed with adenocarcinoma, lymph node metastasis, visceral metastasis as a dominant site, and good performance status. Less than half of the patients received first-line chemotherapy and the majority were treated with carboplatin/paclitaxel combination. During the pathological assessment by immunohistochemistry, 33 different tissue biomarkers were used considering the whole series, and CK7, CK20, TTF-1, vimentin, and CEA were the most common (93.5%, 88.0%, 78.7%, 71.3% and 65.7%, respectively). Serum biomarkers such as CEA, CA 19.9, CA 15.3, or alpha-fetoprotein were requested in 49.4% of cases and at least one of them was altered in 78% of those cases.
PD-L1 expression and outcomes
Fifty-seven cases were excluded from immunohistochemistry analysis, due to technical issues or unavailable biological material. A total of 109 cases were analyzed for PD-L1 expression. Using the CPS score, it was found that 18.3% expressed PD-L1 (Fig. 1).
PD-L1 expression was significantly associated with non-visceral metastasis and a dominance of nodal metastasis, as well as biopsies from lymph nodes (Table 2).
The median overall survival was only 3.7 (95% CI 1.6–5.8) months and patients who expressed PD-L1 obtained better median overall survival compared to those who did not express it (18.7 versus 3.0 months, p-value: < 0.001)(Fig. 2). The presence of visceral metastasis and PS ECOG equal to or more than two were associated with increased risk of death, while PD-L1 expression was a protective factor in univariate analysis (Table 3). However, in the multivariate analysis, only PS ECOG equal to or more than two and PD-L1 expression were independent prognostic factors (HR: 2.37 and 0.42, respectively) (Table 3).
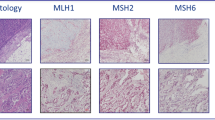
Microsatellite instability analysis
MSI analysis was conclusive in 120 cases, with 46 being excluded due to insufficient/inappropriate DNA quality or biological material unavailability. We found that only 2 out of the 120 cases (1,6%) were MSI positive (Fig. 3). One patient was a 46-year-old woman with a family history of breast cancer, diagnosed with metastatic adenocarcinoma in lymph nodes, the sole site of metastasis. She received chemotherapy comprising a combination of carboplatin and paclitaxel, achieving 8 months of progression-free time. The patient received gemcitabine as second-line treatment with no response in 3 months and died 14 months after diagnosis. The tumor did not express PD-L1. The other MSI-positive patient was a 40-year-old woman, smoker, and alcohol drinker, with a family history of prostate cancer, colorectal cancer, and lung cancer. The patient was diagnosed with metastatic adenocarcinoma in the lymph nodes, the dominant site of metastasis, and had liver metastasis. The patient received chemotherapy combining carboplatin and paclitaxel and achieved only 6 months of progression-free time. She received doxorubicin as second-line treatment with limiting toxicity and obtained no response. She died 18 months after diagnosis. The tumor highly expressed PD-L1 with CPS of 25.
Discussion
Despite the breakthroughs in cancer therapeutics in the last decades, CUP remains a difficult prognostic disease. In the present study, we analyzed a significant number of CUP cases, following strict selection criteria, to explore the role of PD-L1 and MSI.
Our cohort is in line with other reports that demonstrated a mean age around 60s and poor overall survival [29, 30]. In a large Canadian registry study, the median overall survival of CUP achieved only 2 months and was even poor for those that were unable to receive any treatment [31]. In our series, only half of the cases were able to receive first-line chemotherapy and the median overall survival was less than 4 months. None of the included patients received treatment with immune checkpoint inhibitors.
The PD-L1 expression has been well explored in tumors, but few studies have investigated it in CUPs. Haratani et al. showed that the expression of immune checkpoint biomarkers seems to be similar to that in other solid tumors that commonly respond to immune checkpoint inhibitors [32]. Twenty-eight percent of CUPs harbor some immune checkpoint biomarker such as MSI, PD-L1, or high tumor mutational burden, as well as around 22% of CUPs express PD-L1 using a 5% cutoff [33]. We found 18.3% of CUPs expressing PD-L1 using 1% cutoff with the E1L3N® immune assay antibody. Despite different cutoffs, immune assay antibodies and platforms (e.g., Dako, Roche Diagnostics, Ventana) have been used in different studies to assess PD-L1 expression [34, 35]. Koomen et al. addressed this issue in a systematic review and observed agreement among the different immune assays, including those that used E1L3N® immune assay antibody. [36] Although PD-L1 has been investigated in several types of tumors as a therapeutic predictive biomarker, even patients who do not express it might benefit from immune checkpoint inhibitors [37, 38].
We found a reduction of 58% on relative risk of death associated with PD-L1 expression in our study. At variance, some studies have associated PD-L1 expression to worse prognosis, putatively by promoting tumor immune evasion and consequent disease progression [39,40,41]. Other factors not yet evaluated in the tumor microenvironment might explain such outcome discrepancies. Huang et al. found that PD-L1 expression was associated with short survival in breast cancer. However, it is worth noting that PD-L1 expressed only in tumor infiltrated lymphocytes (TILs) and resulted in better survival, achieving a reduction of 59% on relative risk of death [42]. We did not investigate TILs in our study, and other studies have also reported different outcomes in different tumor types associated with PD-L1 expression [43, 44]. Different forms of extracellular PD-L1, such as on exosomes or as a freely soluble protein, have been described. Alongside other mechanisms, these might shed light on a better understanding of CUP microenvironment and clinical outcomes.
MSI is a genomic instability biomarker that is commonly associated with high tumor mutational burden [45]. Cancers with high frequency of MSI are likely to be immunogenic and led to FDA approving the immune checkpoint inhibitor pembrolizumab as an agnostic agent for all tumors harboring MSI [45]. We found only 1.8% of our cases harboring MSI, in line with frequencies reported by Gatalica et al. on 384 CUP cases [46]. Furthermore, the CUPISCO trial (NCT03498521) has been using comprehensive genomic profiling (CGP) to assign patients with CUP to targeted or immunotherapy treatment, and just 3 out of 96 cases were MSI positive (1%) [47]. Despite being rare, MSI in CUPs might open the opportunity to use immunotherapy, mainly in chemotherapy-refractory cases.
Our findings point toward immunotherapy as a potential therapeutic strategy for CUPs as is already seen in some early clinical trial results [48, 49]. Another aspect to point out is that over a half of the patients did not undergo chemotherapy, primarily due to their low clinical performance at diagnosis, highlighting the need for strategies aimed at earlier diagnosis and a shorter interval between diagnosis and the initiation of systemic treatment.
The present work has some limitations: it has a retrospective design and the number of patients was not large enough to allow statistical power, which may raise issues related to selection bias. Another issue is the single-institution nature, as issues concerning patient referral, treatment access, and service protocols might influence clinical outcomes, thus limiting the generalizability of the findings. Nevertheless, we employed a validated immunohistochemistry protocol, using strict selection criteria to maximize sample homogeneity and assembled a relevant case series, given the acknowledged rarity of the CUPs.
In conclusion, PD-L1 is expressed in a subset (circa 20%) of patients with cancer of unknown primary site and is an independent predictor of overall survival in a sample not exposed to immune checkpoint inhibitors. MSI is a rare event in these patients. The analysis of these two immune biomarkers can identify a group of CUP patients, who could benefit from immunotherapy approaches.
References
Greco FA (2019) Cancer of unknown primary site. DeVita, hellman, and rosenberg’s cancer: principles & practice of oncology. 11th edition. Wolters Kluwer, Philadelphia, pp 1720–37
Losa F, Soler G, Casado A et al (2018) SEOM clinical guideline on unknown primary cancer (2017). Clin Transl Oncol 20(1):89–96
Oien KA (2009) Pathologic evaluation of unknown primary cancer. Semin Oncol 36(1):8–37
Wick MR (2008) Immunohistochemical approaches to the diagnosis of undifferentiated malignant tumors. Ann Diagn Pathol 12(1):72–84
Fatima N, Zaman MU, Zaman A et al (2020) Detection efficiency of (18)F-flourodeoxyglucose positron emission tomography/computed tomography for primary tumors in patients with carcinoma of unknown primary. World J Nucl Med 19(1):47–51
van de Wouw AJ, Jansen RL, Speel EJ et al (2003) The unknown biology of the unknown primary tumour: a literature review. Ann Oncol 14(2):191–196
Kamposioras K, Pentheroudakis G, Pavlidis N (2013) Exploring the biology of cancer of unknown primary: breakthroughs and drawbacks. Eur J Clin Invest 43(5):491–500
Mohrmann L, Werner M, Oles M et al (2022) Comprehensive genomic and epigenomic analysis in cancer of unknown primary guides molecularly-informed therapies despite heterogeneity. Nat Commun 13(1):4485
Handorf CR, Kulkarni A, Grenert JP et al (2013) A multicenter study directly comparing the diagnostic accuracy of gene expression profiling and immunohistochemistry for primary site identification in metastatic tumors. Am J Surg Pathol 37(7):1067–1075
Ross JS, Wang K, Gay L et al (2015) Comprehensive genomic profiling of carcinoma of unknown primary site: new routes to targeted therapies. JAMA Oncol 1(1):40–49
Gatalica Z, Millis SZ, Vranic S et al (2014) Comprehensive tumor profiling identifies numerous biomarkers of drug response in cancers of unknown primary site: analysis of 1806 cases. Oncotarget 5(23):12440–12447
Kato S, Alsafar A, Walavalkar V et al (2021) Cancer of unknown primary in the molecular era. Trends Cancer 7(5):465–477
Dermawan JK, Rubin BP (2021) The role of molecular profiling in the diagnosis and management of metastatic undifferentiated cancer of unknown primary(✰): molecular profiling of metastatic cancer of unknown primary. Semin Diagn Pathol 38(6):193–198
Pavlidis N (2003) Cancer of unknown primary: biological and clinical characteristics. Ann Oncol 14(Suppl 3):11–8
Amela EY, Lauridant-Philippin G, Cousin S et al (2012) Management of “unfavourable” carcinoma of unknown primary site: synthesis of recent literature. Crit Rev Oncol Hematol 84(2):213–223
Pentheroudakis G, Stoyianni A, Pavlidis N (2011) Cancer of unknown primary patients with midline nodal distribution: midway between poor and favourable prognosis? Cancer Treat Rev 37(2):120–126
Ishida Y (2020) PD-1: its discovery, involvement in cancer immunotherapy, and beyond. Cells. https://doi.org/10.3390/cells9061376
Balar AV, Weber JS (2017) PD-1 and PD-L1 antibodies in cancer: current status and future directions. Cancer Immunol Immunother 66(5):551–564
Darvin P, Toor SM, Sasidharan Nair V et al (2018) Immune checkpoint inhibitors: recent progress and potential biomarkers. Exp Mol Med 50(12):1–11
Shiravand Y, Khodadadi F, Kashani SMA et al (2022) Immune checkpoint inhibitors in cancer therapy. Curr Oncol 29(5):3044–3060
Li K, Luo H, Huang L et al (2020) Microsatellite instability: a review of what the oncologist should know. Cancer Cell Int 20:16
Marcus L, Lemery SJ, Keegan P et al (2019) FDA approval summary: pembrolizumab for the treatment of microsatellite instability-high solid tumors. Clin Cancer Res 25(13):3753–3758
Harris PA, Taylor R, Thielke R et al (2009) Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381
Massard C, Loriot Y, Fizazi K (2011) Carcinomas of an unknown primary origin–diagnosis and treatment. Nat Rev Clin Oncol 8(12):701–710
De Marchi P, Leal LF, Duval da Silva V et al (2021) PD-L1 expression by tumor proportion score (TPS) and Combined Positive Score (CPS) are similar in non-small cell lung cancer (NSCLC). J Clin Pathol 74(11):735–40
Kulangara K, Zhang N, Corigliano E et al (2019) Clinical utility of the combined positive score for programmed death ligand-1 expression and the approval of pembrolizumab for treatment of gastric cancer. Arch Pathol Lab Med 143(3):330–337
Xie T, Zhang Z, Zhang X et al (2021) Appropriate PD-L1 Cutoff value for gastric cancer immunotherapy: a systematic review and meta-analysis. Front Oncol 11:646355
Carcano FM, Lengert AH, Vidal DO et al (2016) Absence of microsatellite instability and BRAF (V600E) mutation in testicular germ cell tumors. Andrology 4(5):866–872
Pavlidis N, Briasoulis E, Hainsworth J et al (2003) Diagnostic and therapeutic management of cancer of an unknown primary. Eur J Cancer 39(14):1990–2005
Greco FA, Pavlidis N (2009) Treatment for patients with unknown primary carcinoma and unfavorable prognostic factors. Semin Oncol 36(1):65–74
Kim CS, Hannouf MB, Sarma S et al (2018) Survival outcome differences based on treatments used and knowledge of the primary tumour site for patients with cancer of unknown and known primary in Ontario. Curr Oncol 25(5):307–316
Ribas A, Wolchok JD (2018) Cancer immunotherapy using checkpoint blockade. Science 359(6382):1350–1355
Hainsworth JD, Greco FA (2018) Cancer of unknown primary site: new treatment paradigms in the era of precision medicine. Am Soc Clin Oncol Educ Book 38:20–25
Patel SP, Kurzrock R (2015) PD-L1 expression as a predictive biomarker in cancer immunotherapy. Mol Cancer Ther 14(4):847–856
Kerr KM, Tsao MS, Nicholson AG et al (2015) Programmed death-ligand 1 immunohistochemistry in lung cancer: in what state is this art? J Thorac Oncol 10(7):985–989
Koomen BM, Badrising SK, van den Heuvel MM et al (2020) Comparability of PD-L1 immunohistochemistry assays for non-small-cell lung cancer: a systematic review. Histopathology 76(6):793–802
Grossman JE, Vasudevan D, Joyce CE et al (2021) Is PD-L1 a consistent biomarker for anti-PD-1 therapy? The model of balstilimab in a virally-driven tumor. Oncogene 40(8):1393–1395
Davis AA, Patel VG (2019) The role of PD-L1 expression as a predictive biomarker: an analysis of all US food and drug administration (FDA) approvals of immune checkpoint inhibitors. J Immunother Cancer 7(1):278
Wen Y, Chen Y, Duan X et al (2019) The clinicopathological and prognostic value of PD-L1 in urothelial carcinoma: a meta-analysis. Clin Exp Med 19(4):407–416
Zhou ZJ, Zhan P, Song Y (2015) PD-L1 over-expression and survival in patients with non-small cell lung cancer: a meta-analysis. Transl Lung Cancer Res 4(2):203–208
Gajewski TF, Schreiber H, Fu YX (2013) Innate and adaptive immune cells in the tumor microenvironment. Nat Immunol 14(10):1014–1022
Huang W, Ran R, Shao B et al (2019) Prognostic and clinicopathological value of PD-L1 expression in primary breast cancer: a meta-analysis. Breast Cancer Res Treat 178(1):17–33
Wang X, Teng F, Kong L et al (2016) PD-L1 expression in human cancers and its association with clinical outcomes. Onco Targets Ther 9:5023–5039
Pyo JS, Kang G, Kim JY (2017) Prognostic role of PD-L1 in malignant solid tumors: a meta-analysis. Int J Biol Markers 32(1):e68–e74
Chalmers ZR, Connelly CF, Fabrizio D et al (2017) Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med 9(1):34
Gatalica Z, Xiu J, Swensen J et al (2018) Comprehensive analysis of cancers of unknown primary for the biomarkers of response to immune checkpoint blockade therapy. Eur J Cancer 94:179–186
Ross JS, Sokol ES, Moch H et al (2021) Comprehensive genomic profiling of carcinoma of unknown primary origin: retrospective molecular classification considering the CUPISCO study design. Oncologist 26(3):e394–e402
Naing A, Meric-Bernstam F, Stephen B et al (2020) Phase 2 study of pembrolizumab in patients with advanced rare cancers. J Immunother Cancer 8(1):e000347
Tanizaki J, Yonemori K, Akiyoshi K et al (2020) NivoCUP: An open-label phase II study on the efficacy of nivolumab in cancer of unknown primary. J Clin Oncol 38(15):106
Acknowledgements
We would like to thank all our patients who contributed to this study.
Funding
This study was partially supported by the Public Ministry of Labor Campinas (Research, Prevention, and Education of Occupational Cancer—15ª zone, Campinas, Brazil). RMR was supported by the National Council for Scientific and Technological Development (CNPq, Brazil) as Research Productivity Scholarship—Level 1B; FMC was supported by PAIP (Researcher Support Program) from Barretos Cancer Hospital; MEL was supported by the National Council for Scientific and Technological Development (CNPq, Brazil) as novice scientific grantee; CP was supported by the National Council for Scientific and Technological Development (CNPq, Brazil) as Research Productivity Scholarship—Level 2 (309998/2019-0 and 308085/2022-1).
Author information
Authors and Affiliations
Contributions
FMC, RMR, and CP designed the study and critically revised the results. JNJ and MEL retrieved the clinicopathological data of patients from medical records. JNJ and VDS analyzed the histological sections and performed the immunohistochemical readings. MB and GNB supervised the MSI experiments and analyzed the results. FMC, JNJ, and MAL analyzed the data and performed the statistics. JNJ and DAP wrote the manuscript draft. FMC, RMR, CP, and VDS revised the final manuscript. All authors agreed to be accountable for the content of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Junior, J.N.A., Preto, D.D., Lazarini, M.E.Z.N. et al. PD-L1 expression and microsatellite instability (MSI) in cancer of unknown primary site. Int J Clin Oncol 29, 726–734 (2024). https://doi.org/10.1007/s10147-024-02494-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-024-02494-3