Abstract
The development of novel antitumor agents and accompanying biomarkers has improved survival across several tumor types. Previously, we developed recommendations for tumor-agnostic treatments in patients with solid tumors with DNA mismatch repair deficient or neurotrophic receptor tyrosine kinase fusions. Recently, immune checkpoint inhibitors have shown efficacy in patient with tumor mutation burden-high (TMB-H) solid tumors and have been established as a third tumor-agnostic agent, making it necessary to develop the guideline prioritized for these patients. Clinical questions regarding medical care were formulated for patients with TMB-H advanced solid tumors. Relevant publications were searched by PubMed and Cochrane Database. Critical publications and conference reports were added manually. Systematic reviews were performed for each clinical question for the purpose of developing clinical recommendations. The committee members identified by Japan Society of Clinical Oncology (JSCO), Japanese Society of Medical Oncology (JSMO), and Japanese society of pediatric hematology/oncology (JSPHO) voted to determine the level of each recommendation considering the strength of evidence, expected risks and benefits to patients, and other related factors. Thereafter, a peer review by experts nominated from JSCO, JSMO, and JSPHO, and the public comments among all societies' members was done. The current guideline describes three clinical questions and seven recommendations for whom, when, and how TMB should be tested, and what is recommended for patients with TMB-H advanced solid tumors. In this guideline, the committee proposed seven recommendations for performing TMB testing properly to select patients who are likely to benefit from immunotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the field of cancer drug therapy, treatment outcomes and prognosis have improved as effective novel drug therapies have emerged [1, 2]. At the same time, the development of biomarkers to identify groups in which efficacy is likely prior to treatment also has contributed to improvements in cancer treatment outcomes. Conventional cancer treatment has involved a multifaceted assessment that encompasses the pathological diagnosis of the disease and an evaluation of its stage, the benefits and disadvantages of treatment, and the preferences of the patient. In diagnosing the disease, identifying the primary tumor and determining the tissue type have yielded important information that has been key to establishing a treatment plan. Recent advances in molecular biology have elucidated a variety of biological characteristics of tumors, resulting in the clinical development and regulatory approval of tumor-agnostic drugs that transcend the organic characteristics of the disease.
An anti-programmed cell death protein 1 (PD-1) antibody drug, pembrolizumab, for advanced/recurrent deficient DNA mismatch repair (dMMR) solid cancers and tropomyosin receptor kinase (TRK) inhibitors against neurotrophic receptor tyrosine kinase (NTRK) fusion gene-positive advanced solid cancers were approved in tumor-agnostic therapy [3]. Moreover, the efficacy of pembrolizumab against tumor mutation burden-high (TMB-H) solid tumors was demonstrated, and the US Food and Drug Administration (FDA) approved it in 2020 [3]. In Japan, pembrolizumab was approved for patients with TMB-H solid tumors, which was the third tumor-agnostic drug approved.
This article is a summary of the part describing TMB-H in “Clinical Practice Guidelines for Tumor-Agnostic Treatments in Adult and Pediatric Patients with Advanced Solid Tumors toward Precision Medicine (in Japanese)”. The part regarding dMMR and NTRK fusion has already been reported elsewhere [4, 5].
The present guidelines provide a guide to diagnosis and treatment and should be utilized in clinical practice according to the recommendation levels described and by adjusting them for individual patients. They are expected to contribute to improving treatment outcomes in patients with solid cancer by utilizing them to perform appropriate tests and treatments on appropriate patients at appropriate timing.
Materials and methods
The current guidelines systematically describe the items to be considered when treating patients with TMB-H solid tumors, including the timing and methods of testing TMB score and the positioning of immunotherapy. In the clinical setting in Japan, if appropriate tests are performed on appropriate patients and the patients receive appropriate treatment at appropriate timing based on the recommended levels described in the present guidelines, treatment outcomes in patients with solid tumors are expected to be improved.
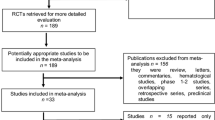
In the preparation of these guidelines, clinical questions (CQs) were set, and regarding evidence that provides the basis for the answers to those questions, the literature was collected by hand searches and subjected to a systematic review. In setting the CQs, the working group of the Clinical Practice Guidelines for Tumor-Agnostic Genomic Medicine in Adult and Pediatric Patients with Advanced Solid Tumors (3rd edition) prepared draft CQs and decided which ones would be included in the guidelines.
Keywords related to each CQ were selected and sent to the Japan Medical Library Association, which generated queries used to perform comprehensive literature searches. The PubMed, Ichushi Web, and Cochrane Library databases were used in the searches. Important reports by various academic societies also were collected by hand searches and used in the guidelines. Primary and secondary screenings and systematic reviews were performed by persons in charge (SM/YN) of the working group of the Clinical Practice Guidelines for Tumor-Agnostic Genomic Medicine in Adult and Pediatric Patients with Advanced Solid Tumors (3rd edition). The recommendation levels specified for the CQs were determined by voting by the committee members (Table 1). The levels, which were determined based on factors such as the strength of the evidence and the expected benefits and disadvantages for patients, are as follows: strongly recommended (SR), recommended (R), expert consensus opinion (ECO), and not recommended (NR). The status of regulatory approval and insurance coverage in Japan for the treatments (including indications for testing and treatment) was not considered during the voting, but was indicated in the remarks section as needed. The overall assessments based on voting were as follows: (1) SR if ≥ 70% of the votes were for SR; (2) R if criterion (1) was not met and SR votes + R votes accounted for ≥ 70% of the total; (3) ECO if criteria (1) and (2) were not met and SR votes + R votes + ECO votes accounted for ≥ 70% of the total; and (4) NR if NR accounted for ≥ 50% of the total regardless of whether criteria (1), (2), or (3) were met. If all of the criteria (1)–(4) were not met, the assessment was "no recommendation level."
The recommendations for the CQs include recommendations that are not currently based on strong evidence. As new evidence accumulates, the information and recommendations in these guidelines may change significantly. Although these guidelines will be updated as appropriate, in using a drug clinically, the latest medical information should be reviewed, and every effort made to ensure the drug is used properly.
Results
Solid tumors with a high tumor mutation burden (TMB-H)
A characteristic of cancer cells is that they have more genetic mutations than normal cells due to external factors such as exposure to ultraviolet light or smoking, therapeutic interventions such as temozolomide administration, or inborn or acquired genetic causes related to the DNA repair mechanism [6, 7]. The tumor mutation burden (TMB) refers to the quantity of somatic mutations in cancer cells and is expressed in the unit “mut/Mb,” which represents mutations per 1 million bases (1 megabase, or Mb). In preclinical studies, it was found that new peptides produced as a result of non-synonymous mutations, among the passenger gene mutations in cancer cells, are presented as neoantigens by the major histocompatibility complex (MHC) of the surface of antigen-presenting cells and may be recognized as non-self by infiltrating immune cells [8, 9]. Next-generation sequencing technology and calculation methods for predicting antigen peptide presentation by MHC have been developed, and the presence of neoantigens recognized by T cells has been reported in high-TMB mouse tumors, which are similar to high-TMB human tumors [9]. Moreover, immunogenicity associated with increased TMB has been confirmed in nonclinical studies, suggesting that those biological characteristics are applicable across cancer types [10, 11]. Furthermore, a review by Schumacher and Schreiber suggested that in tumors with somatic mutations in excess of 10 mut/Mb (equivalent to 150 non-synonymous mutations), neoantigens that are recognized by the immune system may be produced [12].
TMB testing
TMB has previously been evaluated by whole genome sequencing (WGS) or whole exome sequencing (WES). However, target sequencing panels (gene panel tests) have also recently been found to enable TMB to be assayed with high sensitivity [13,14,15,16]. Because TMB scores obtained by gene panel tests in which genome sequencing of a 1.1 Mb TMB analysis region is performed correlate with WES TMB scores, these panel tests can measure TMB accurately. However, with a region of ≤ 0.5 Mb, a lower correlation has been reported [13]. The algorithms used in calculating the TMB value (TMB score) are designed to be optimal for each gene panel. This is problematic because they are the intellectual property of each panel and therefore not openly disclosed, resulting in variability (Table 2) [17]. TMB harmonization is currently being pursued in a TMB harmonization project led by the Friends of Cancer Research (FoCR). FoCR verifies the correlations between TMB scores calculated based on each gene panel test and WES TMB scores. Although there is variability depending on the type of cancer, good correlations have been reported (Spearman’s correlation coefficients of 0.79–0.88). In Japan, testing can be performed as part of comprehensive genomic profiling under the national health insurance coverage. TMB measured by the FoundationOne® CDx assay was found to be highly correlated with WES TMB [10]. A strong correlation was also reported for the NCC Oncopanel [18] (Fig. 1). In the future, FoCR plans to retrospectively analyze the clinical specimens of patients administered immune checkpoint inhibitors in clinical studies with the aim of making TMB testing available in clinical setting.
Comparison of tumor mutation burden measured by whole exome sequencing versus comprehensive genomic profiling [13, 18]. Comparison of tumor mutation burden measured by whole exome sequencing versus comprehensive genomic profiling (left: FoundationOne CDx, right: NCC Oncopanel). The line y = x is plotted in red
Pembrolizumab was found to be effective in TMB-H solid tumors in the phase II KEYNOTE-158 study, which used biomarkers to evaluate pembrolizumab efficacy in patients with unresectable advanced or recurrent solid tumors who were refractory or intolerant to prior treatment [18]. In this study, patients with TMB-H ≥ 10 mut/Mb, as analyzed by the FoundationOne® CDx assay, were defined as being TMB-H patients. Based on the results of this study, the FDA approved pembrolizumab for the treatment of TMB-H solid tumors and FoundationOne® CDx as a companion diagnostic for pembrolizumab. In Japan, FoundationOne® CDx was approved on November 15, 2021 to assist in determining whether a drug is indicated for a solid tumor with a high-TMB score.
The conventional method of calculating TMB involves an analysis of tumor tissue. Consequently, in cases such as when a tumor is unresectable and only previously collected surgical specimens can be obtained, TMB analysis using FoundationOne® CDx may not reflect tumor status at the point when systemic treatment is administered. Efforts have therefore been made to evaluate TMB by analyzing circulating tumor DNA (ctDNA) from the blood. As compared with tumor tissue analysis, ctDNA analysis requires less time [19] and may detect intratumoral genetic heterogeneity [20].
Frequency of TMB-H by cancer type
The frequency of somatic mutations by cancer type is indicated in Fig. 2. The frequency varies widely depending on the cancer type, ranging from more than 100 mut/Mb (e.g., melanoma, lung squamous cell carcinoma/lung adenocarcinoma) to a low 0.1 mut/Mb. Even within the same cancer type, differences of 1000-fold or more are seen [21].
Whole-exome somatic mutation frequencies observed in exomes from tumor–normal pairs [21]. AML acute myeloid leukemia, CLL chronic lymphocytic leukemia, DLBCL diffuse large B-cell lymphoma. Each dot corresponds to a tumor–normal pair, with vertical position indicating the total frequency of somatic mutations in the exome. Mutation frequencies vary more than 1,000-fold between lowest and highest across different cancers and also within several tumor types. The bottom panel shows the relative proportions of the six different possible base-pair substitutions, as indicated in the legend on the left
The incidence of cancers with TMB scores ≥ 10 mut/Mb as determined using the FoundationOne® CDx assay (see “TMB testing” for more information) was reported in a review by Chan et al. (Fig. 3) [22]. The percentage of the top 30 types of cancer with TMB scores ≥ 10 mut/Mb ranged from approximately 10% to 60% and represented 13.3% of solid tumors as a whole. At a joint meeting of the Japanese Society of Medical Oncology (JSMO), European Society for Medical Oncology (ESMO), American Society of Clinical Oncology (ASCO), and Taiwan Oncology Society (TOS) organized by the Japan Society of Clinical Oncology (JSCO), the incidence of TMB-H tumors in the FoundationOne database was reported using a TMB-H cutoff of TMB ≥ 20 mut/Mb (Table 3) [23]. The percentages in the 30 cancer types with the highest incidences ranged from 0.93 to 54.60%. TMB-H solid tumors have been reported to have a poor prognosis [24].
Prevalence of solid tumors with TMB ≥ 10 mut/Mb [22]. NOS not otherwise specified. Analysis of top 30 solid tumor types selected from 104,814 total cases sorted by percent of cases with TMB ≥ 10 mut/Mb according to the Foundation Medicine database
Effort also has been made to evaluate TMB by cancer type using ctDNA analysis. Foundation Medicine Inc. developed an assay to evaluate blood TMB (bTMB) by analyzing blood ctDNA. Pretherapy baseline bTMB in blood specimens was evaluated in the prospective POPLAR and OAK studies, which evaluated the efficacy of atezolizumab as compared with that of docetaxel in non-small cell lung cancer [25]. Tissue TMB (tTMB) also was analyzed at the same time in these studies using tumor tissue, and the sensitivity and specificity of bTMB as compared with tTMB were found to be 64% and 88%, respectively. FoundationOne® Liquid CDx developed by Foundation Medicine Inc. was approved in Japan in March 2021 for comprehensive genomic profiling of solid tumors using blood specimens.
The incidences of tTMB-H (≥ 10 mut/Mb), analyzed in tumor tissue using the FoundationOne® CDx assay, and bTMB-H (≥ 10 mut/Mb), analyzed in blood using the FoundationOne® Liquid CDx assay, have been reported by cancer type (Fig. 4) [26]. Sixteen cancer types in 167,332 patients were analyzed. The incidence of tTMB-H was 19%, and the cancer types with the highest incidences of tTMB-H were, in descending order of incidence, malignant melanoma (53%), small cell lung cancer (41%), non-small cell lung cancer (40%), bladder cancer (39%), and endometrial cancer (23%). In the bTMB analysis, which examined 16 cancer types in 9312 patients, the incidence of bTMB-H was 13%. The prevalence by cancer type was correlated with prevalence of elevated tissue TMB (r = 0.81). While there are some reports of high correlation in lung cancer, there are also reports of low correlation and concordance rates in gastrointestinal cancer, and differences by metastatic organ have also been reported [27, 28]. Further investigation of bTMB is needed.
Prevalence of solid tumors with TMB ≥ 10 mut/Mb and bTMB ≥ 10 mut/Mb [25]. NSCLC non-small cell lung cancer. Pan-cancer, TMB ≥ 10 was detected in 19% of tissue cases (31,272/167,332) and was common in melanoma (53%), small cell (41%), NSCLC (40%), bladder (39%), and endometrium (23%). bTMB ≥ 10 was detected in 13% of liquid biopsies (1195/9312); prevalence by cancer type was correlated with prevalence of elevated tissue TMB (r = 0.81)
Efficacy of anti-PD-1/PD-L1 antibody drugs against TMB-H solid tumors
In preclinical studies, novel peptides produced by amino acid substitutions resulting from DNA mutations among the passenger gene mutations of cancer cells were presented as neoantigens, causing an antitumor immune response [8, 9]. Mouse tumors with high TMB have been reported to have neoantigens that are recognized by T cells [9]. Moreover, immunogenicity associated with increased TMB has been confirmed in nonclinical studies [10, 11, 29], suggesting that an increase in neoantigens resulting from increased TMB in tumor cells may promote tumor recognition by T cells. Immune checkpoint inhibitors are therefore likely to have an antitumor effect in TMB-H solid tumors by facilitating T-cell activation. The KEYNOTE-028 study was a phase Ib study that examined the safety and efficacy of pembrolizumab in advanced solid tumors positive for PD-L1 expression. As an exploratory endpoint, the study examined the relationship between TMB and PD-L1. WES TMB was analyzed for 16 cancer types in 77 patients (only 1 of whom was MSI-H), and a stronger tumor regression effect and prolongation of PFS were seen in patients with high TMB [30]. TMB was investigated using the MSK-IMPACT platform in 1662 patients who received immune checkpoint inhibitor monotherapy or combination therapy at the Memorial Sloan Kettering Cancer Center in the United States. A comparison of patients with the highest 20% of TMB scores and the other patients by cancer type showed that OS was significantly longer in the former group (HR: 0.52; p = 1.6 × 10−6) [31]. In addition to these studies, many others have also found TMB to be a useful factor for predicting the efficacy of immune checkpoint inhibitors. When the objective response rate (ORR) seen with immune checkpoint inhibitor monotherapy (anti-PD-1 or anti-PD-L1 antibody) was plotted against the median TMB for 27 cancer types, a significant correlation between ORR and TMB was observed (Fig. 5) [32].
Correlation between TMB and ORR with anti-PD-1/PD-L1 therapy in various cancer types [32]. MMRd mismatch repair deficient, NSCLC non-small cell lung cancer. Shown is the median number of coding somatic mutations per megabase (MB) of DNA in 27 tumor types or subtypes among patients who received inhibitors of programmed death 1 (PD-1) protein or its ligand (PD-L1), as described in published studies for which data regarding the objective response rate are available. The number of patients who were evaluated for the objective response rate is shown for each tumor type (size of the circle), along with the number of tumor samples that were analyzed to calculate the tumor mutational burden (degree of shading of the circle). Data on the x axis are shown on a logarithmic scale
The KEYNOTE-158 study was a multicenter, non-randomized, open-label, multicohort phase II study that evaluated the efficacy and safety of pembrolizumab in patients with unresectable or metastatic solid tumors who were refractory or intolerant to prior treatment. The study evaluated various biomarkers that predict pembrolizumab efficacy in a variety of cancer types. TMB was designated in advance as an exploratory biomarker and was analyzed retrospectively using the FoundationOne® CDx assay. As a post-marketing requirement for FDA approval in the United States, Group M was subsequently added as prospectively enrolled cohort of patients with TMB-H solid tumors. The primary endpoint of the study was ORR, and the secondary endpoints were the duration of response, progression-free survival (PFS), and overall survival (OS). TMB data were obtained for 790 of the 1050 patients in the efficacy analysis set. Using a TMB-H cutoff of ≥ 10 mut/Mb, 102 patients were classified as TMB-H and 688 as TMB-Low (TMB-L, < 10 mut/Mb). Pembrolizumab showed a higher ORR in the TMB-H group than in the TMB-L group (29% vs. 6%). With MSI-H patients and those whose MSI status was unknown excluded, the ORR in 81 patients in the TMB-H group was 28%, which was comparable. PD-L1 expression was also evaluated in this study. No correlation was seen between TMB score and PD-L1 expression (combined positive score: CPS), and ORR was 35% for PD-L1-positive patients (CPS ≥ 1) in the TMB-H group and 21% for PD-L1-negative patients (CPS < 1) in this group [33]. Based on the results of this study, the FDA approved pembrolizumab for the treatment of TMB-H solid tumors.
The Targeted Agent and Profiling Utilization Registry (TAPUR) study, which was conducted by ASCO, was a phase II basket study that evaluated the antitumor effects of approved targeted drugs in specific genomic alterations. The results for a TMB-H cohort in the study also were reported. An examination of 27 patients with colorectal cancer with TMB ≥ 9 (25 MSS patients, 2 patients with unknown microsatellite status) showed an antitumor effect, with an ORR of 11% (95% CI 2–29%) median PFS of 9.3 weeks (95% CI 7.3–16.1), and median OS of 51.9 weeks (95% CI 18.7–NR) [34]. A similar examination was conducted in breast cancer with TMB ≥ 9 and an antitumor effect was also seen, with the ORR of 37% (95% CI 21–50%), median PFS of 10.6 weeks (95% CI 7.7–21.1), and median OS of 30.6 weeks (95% CI 18.3–103.3) [35].
Even since the FDA approved pembrolizumab for TMB-H solid tumors, debate has continued regarding the TMB-H cutoff and differences in efficacy in each type of cancer. Immune checkpoint inhibitors showed a strong antitumor effect (ORR: 39.8%; 95% CI 34.9–44.8) in TMB-H tumors for cancer types in which tissue invasive CD8 T-cell levels showed a positive correlation with neoantigen levels, such as malignant melanoma, lung cancer, and bladder cancer. The ORR in TMB-H tumors was significantly higher than in TMB-L tumors [odds ratio (OR): 4.1; 95% CI 2.9–5.8; p < 2 × 10−16]. However, in cancer types for which there was no correlation between CD8 T-cell levels and neoantigen levels, such as breast cancer, prostate cancer, and glioma, the ORR of immune checkpoint inhibitors in TMB-H tumors was 15.3% (95% CI 9.2–23.4; p = 0.95), which was significantly lower than in TMB-L tumors (OR: 0.46; 95% CI 0.24–0.88; p = 0.02) [36]. This suggested that, depending on the cancer type, it may not be possible to predict the efficacy of immune checkpoint inhibitors based on TMB. It has also been suggested that the optimal TMB cutoff may differ depending on cancer type [37]. In gliomas, temozolomide therapy results in an increase in TMB, although the mechanism of that change is unknown. However, in an examination of the efficacy of an immune checkpoint inhibitor in 11 patients with TMB-H and dMMR gliomas that included such patients (5 untreated and 6 posttreatment patients), the best therapeutic effect was disease progression in 82%, with no significant difference seen as compared with TMB-L gliomas [38]. These findings indicate a need for further investigation regarding the optimal method of measuring TMB and the TMB cutoff for each cancer type.
Efforts have also been made to evaluate TMB by ctDNA analysis. In 69 patients with solid tumors who were administered an immune checkpoint inhibitor, ctDNA from the blood was analyzed using the Guardant360 assay, a ctDNA testing method. The results showed that PFS was significantly longer in patients with more than 3 variants of unknown significance (VUS) [39]. Moreover, in the OAK and POPLAR studies, which examined the superiority of atezolizumab versus docetaxel in non-small cell lung cancer, ctDNA analysis using the FoundationOne bTMB assay showed that atezolizumab efficacy was greatest in patients whose bTMB score was ≥ 16 [25].
CQs
The following requirements have been prepared regarding the TMB testing performed to select patients who are likely to benefit from PD-1/PD-L1 inhibitors and the administration of them. The clinical recommendations propose the following 7 requirements in 3 CQs regarding the TMB testing performed to select patients who are likely to benefit from anti-PD-1/PD-L1 antibody drugs.
-
1.
For patients with solid tumors who are undergoing standard drug therapy or for whom standard treatment is difficult to administer, other than those for which immune checkpoint inhibitors can be used clinically irrespective of the TMB score, TMB testing is recommended to determine whether immune checkpoint inhibitors are indicated.
-
2.
For patients with unresectable solid tumors for which immune checkpoint inhibitors can already be used clinically irrespective of the TMB score, TMB testing should be considered to determine whether immune checkpoint inhibitors are indicated.
-
3.
For patients with solid tumors that are curable with local treatment, TMB testing is not recommended to determine whether immune checkpoint inhibitors are indicated.
-
4.
For patients with unresectable solid tumors for which an immune checkpoint inhibitor has already been used, TMB testing is not recommended to determine again whether immune checkpoint inhibitors are indicated.
-
5.
As TMB testing to determine whether immune checkpoint inhibitors are indicated, an NGS test whose analytical validity has been established (by receiving regulatory approval, etc.) is recommended.
-
6.
For unresectable/metastatic/recurrent solid tumors with TMB-H, the use of immune checkpoint inhibitors is recommended.
-
7.
The use of immune checkpoint inhibitors is recommended for unresectable/metastatic/recurrent solid tumors that have progressed after chemotherapy.
Please keep in mind that these clinical recommendations will be revised in a timely manner, along with continuously and steadily advancing cancer treatment and new knowledge on biomarkers.
We will explain each CQ in detail.
CQ1: Targets of TMB testing
PubMed was searched using the following queries: “Mutation and Tumor Burden or burden * or TMB,” “neoplasm,” and “tested or diagnos* or detect*.” The same queries were used to search Cochrane Library. For the search period from January 1980 to January 2021, 585 articles were extracted from PubMed and 26 from Cochrane Library. In the primary screening, 233 articles were extracted, and 208 were extracted in the secondary screening. A qualitative systematic review of these articles was then performed.

The KEYNOTE-158 study examined the efficacy of pembrolizumab in advanced or recurrent solid tumors that progressed after chemotherapy. The TMB score was measured using the FoundationOne® CDx assay, and ≥ 10 mut/Mb was used as the TMB-H cutoff. The results showed that the ORR of pembrolizumab was higher in the TMB-H group than in the TMB-L group (29% vs. 6%) [17]. Based on the results of this study, the United States FDA granted the expedited approval of pembrolizumab for unresectable or metastatic TMB-H (≥ 10 mut/Mb) solid tumors on June 16, 2020. In addition, FoundationOne® CDx was approved as a pembrolizumab companion diagnostic. TMB is therefore considered a valid biomarker for immune checkpoint inhibitor use and is also recommended in Japan.

TMB testing is generally considered unnecessary in solid tumors for which immune checkpoint inhibitors can be used irrespective of the TMB score, because determining whether such use is indicated does not depend on the TMB score. However, in solid tumors for which determination regarding whether immune checkpoint inhibitors are indicated is based on PD-L1 expression or a biomarker such as dMMR, an immune checkpoint inhibitor is likely to be effective if the biomarker test was negative. In the KEYNOTE-158 study, ORR was 28% and efficacy was seen regardless of PD-L1 expression (ORR was 35% in PD-L1-positive patients and 21% in PD-L1-negative patients) in the patients with TMB-H after the exclusion of MSI-H patients and patients whose MSI status was unknown [33]. Based on the above findings, in solid tumors for which determination regarding whether immune checkpoint inhibitors are indicated is based on a biomarker, TMB testing is recommended if the biomarker test was negative.

In malignant melanoma, an anti-PD-1 antibody drug has been shown to be effective as postoperative adjuvant therapy and has been approved (KEYNOTE-054 study [40], ONO-4538–21 study [41]). In the multicenter, double-blind, randomized, placebo-controlled phase III PACIFIC study, an anti-PD-L1 antibody drug was administered sequentially in patients with unresectable, locally advanced (Stage III) non-small cell lung cancer that did not progress following curative concurrent chemoradiotherapy (CRT) using a platinum drug. Based on the results of that study, anti-PD-L1 antibody therapy received regulatory approval [42]. In the Checkmate-577 study, the efficacy of nivolumab as postoperative adjuvant therapy was shown in Stage II/III esophageal and gastroesophageal junction cancer that was resected after neoadjuvant chemoradiotherapy [43]. However, because no differences in efficacy according to TMB score were reported in these studies, pretreatment TMB testing is generally unnecessary. Moreover, because the efficacy of immune checkpoint inhibitors as perioperative therapy has not been established for other solid tumors, TMB testing for treatment selection is generally unnecessary for such cancers if the cancer can be cured with local treatment. Based on the above considerations, TMB testing is currently not recommended to determine whether immune checkpoint inhibitors are indicated for patients with solid tumors that are not locally advanced and have not metastasized.

Immune checkpoint inhibitors have been approved for use in some solid tumors irrespective of the TMB score. The effectiveness of using a different immune checkpoint inhibitor when one has already been administered has not been demonstrated. Therefore, TMB testing is not recommended for the purpose of using an immune checkpoint inhibitor in patients with solid tumors for which an immune checkpoint inhibitor has already been used.
CQ2: Testing methods of TMB
PubMed was searched using the following queries: "Mutation and Tumor Burden or burden * or TMB," and "next-generation sequencing or NGS or Whole-exome sequencing or WES." The same queries were used to search Cochrane Library. For the search period from January 1980 to January 2021, 387 articles were extracted from PubMed and 22 from Cochrane Library. In the primary screening, 215 articles were extracted, and 204 were extracted in the secondary screening. A qualitative systematic review of these articles was then performed.

FoundationOne® CDx was approved in Japan on December 27, 2018 for the purpose of obtaining comprehensive genomic profiles of tumor tissue in patients with solid tumors and for the purpose of detecting somatic gene alterations in order to determine whether some molecularly targeted drugs are indicated in such patients. FoundationOne® CDx also includes TMB score information. The KEYNOTE-158 study measured TMB scores using the FoundationOne® CDx assay and examined the efficacy of pembrolizumab in advanced or recurrent solid tumors that progressed after chemotherapy, with a TMB-H cutoff of ≥ 10 mut/Mb. The results showed that the ORR of pembrolizumab was higher in the TMB-H group than in the TMB-L group [17]. Based on the results of this study, the FDA granted expedited approval of pembrolizumab for unresectable or metastatic TMB-H (≥ 10 mut/Mb) solid tumors on June 16, 2020. In addition, FoundationOne® CDx was approved as a pembrolizumab companion diagnostic. In Japan, FoundationOne® CDx was approved on November 15, 2021 to assist in determining whether drugs for solid tumors with high-TMB scores are indicated.
In addition to FoundationOne® CDx, OncoGuide™ NCC Oncopanel System was approved in Japan as a comprehensive genomic profiling test for tumor tissue in patients with solid tumors. As with the FoundationOne® CDx assay, a strong correlation with WES has been reported for this test [15], indicating that it can predict the therapeutic benefit of an immune checkpoint inhibitor. However, as of June 2021, there had been no reports of studies examining the efficacy of an immune checkpoint inhibitor using the OncoGuide™ NCC Oncopanel System. The algorithm used to calculate TMB scores varies depending on the gene panel used, and attention must therefore be paid to the resulting variability. The FoCR is currently performing a retrospective analysis of clinical specimens from patients administered immune checkpoint inhibitors in clinical studies, and it is anticipated that uniform TMB scores obtained with different gene panels will be available in clinical setting.
In addition, the FoundationOne® Liquid CDx Cancer Genome Profile was approved as a comprehensive genomic profiling test for solid tumors using blood specimens on March 22, 2021, and an application for marketing approval of Guardant360CDx was filed on January 28, 2021. Thus, opportunities to perform measurements in clinical practice are expected to increase. The OAK and POPLAR studies, which examined the superiority of atezolizumab versus docetaxel in non-small cell lung cancer, analyzed blood specimens using a bTMB assay and found that atezolizumab efficacy was greater in patients with bTMB scores ≥ 16 [25]. It is anticipated that the efficacy of atezolizumab is verified in other cancer types.
Based on the above findings, an NGS test whose analytical validity has been established using tissue is recommended as TMB testing to determine whether immune checkpoint inhibitors are indicated.
CQ3: Treatment for TMB-H cancer
PubMed was searched using the following queries: "Mutation and Tumor Burden or burden * or TMB," "PD-1 or PD-L1 *," and "treat*." The same queries were used to search Cochrane Library. For the search period from January 1980 to January 2021, 323 articles were extracted from PubMed and 10 from Cochrane Library. In the primary screening, 74 articles were extracted, and 71 were extracted in the secondary screening. A qualitative systematic review of these articles was then performed.

The KEYNOTE-158 study measured TMB scores using the FoundationOne® CDx assay and examined the efficacy of pembrolizumab in advanced or recurrent solid tumors that progressed after chemotherapy, with a TMB-H cutoff of ≥ 10 mut/Mb. The results showed that the pembrolizumab ORR was higher in the TMB-H group than in the TMB-L group (29% vs. 6%) [33]. Immune checkpoint inhibitors have been shown to have a tumor-agnostic therapeutic effect in TMB-H tumors. It should be noted, however, that the reported sample sizes have been limited for some cancer types and that immune checkpoint inhibitors have shown no efficacy in some cancer types (see "4 Efficacy of anti-PD-1/PD-L1 antibody drugs against TMB-H solid tumors").

The efficacy of immune checkpoint inhibitors in treating TMB-H solid tumors was shown in the KEYNOTE-158 study, which examined advanced or recurrent solid tumors that progressed after chemotherapy. Therefore, it is currently not the first-line therapy of choice. In view of the turnaround time (TAT) required for TMB testing, it is generally considered preferable to start the first-line therapy established for each organ (standard treatment) without waiting for the results of TMB testing. However, TMB is an important biomarker for investigating subsequent therapy, and testing for it and other biomarkers should therefore be considered at an early stage.
Conclusion
Immune checkpoint inhibitors significantly prolongs patient survival in many types of cancers; however, significant resistance to this therapeutic modality has been reported. Thus, to identify patients who are more likely to benefit from this therapy, various biomarkers, including TMB, have been examined. However, there are some issues related to administering immune checkpoint inhibitors for TMB-H tumors in the clinical setting. In this guideline, the panel recommends the requirements for performing TMB testing properly to select patients who are likely to benefit from immune checkpoint inhibitors.
References
Looney AM, Nawaz K, Webster RM (2020) Tumour-agnostic therapies. Nat Rev Drug Discov 19(6):383–384
Davis AA, McKee AE, Kibbe WA et al (2018) Complexity of delivering precision medicine: opportunities and challenges. Am Soc Clin Oncol Educ Book 38:998–1007
Chakravarty D, Johnson A, Sklar J et al (2022) Somatic genomic testing in patients with metastatic or advanced cancer: ASCO provisional clinical opinion. J Clin Oncol 40(11):1231–1258
Mishima S, Taniguchi H, Akagi K et al (2019) Japan Society of Clinical Oncology provisional clinical opinion for the diagnosis and use of immunotherapy in patients with deficient DNA mismatch repair tumors, cooperated by Japanese Society of Medical Oncology, first edition. Int J Clin Oncol 25(2):217–239
Naito Y, Mishima S, Akagi K et al (2020) Japan society of clinical oncology/Japanese society of medical oncology-led clinical recommendations on the diagnosis and use of tropomyosin receptor kinase inhibitors in adult and pediatric patients with neurotrophic receptor tyrosine kinase fusion-positive advanced solid tumors, cooperated by the Japanese society of pediatric hematology/oncology. Int J Clin Oncol 25(3):403–417
Alexandrov LB, Nik-Zainal S, Wedge DC et al (2013) Signatures of mutational processes in human cancer. Nature 500(7463):415–421
Zehir A, Benayed R, Shah RH et al (2017) Mutational landscape of metastatic cancer revealed from prospective clinical sequencing of 10,000 patients. Nat Med 23(6):703–713
Castle JC, Kreiter S, Diekmann J et al (2012) Exploiting the mutanome for tumor vaccination. Cancer Res 72(5):1081–1091
Matsushita H, Vesely MD, Koboldt DC et al (2012) Cancer exome analysis reveals a T-cell-dependent mechanism of cancer immunoediting. Nature 482(7385):400–404
Old LJ, Boyse EA, Clarke DA et al (1962) Antigenic properties of chemically induced tumors. Ann N Y Acad Sci 101(1):80–106
Baldwin RW (1955) Immunity to methylcholanthrene-induced tumours in inbred rats following atrophy and regression of the implanted tumours. Br J Cancer 9(4):652–657
Schumacher TN, Schreiber RD (2015) Neoantigens in cancer immunotherapy. Science 348(6230):69–74
Chalmers ZR, Connelly CF, Fabrizio D et al (2017) Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med 9(1):34
Drilon A, Wang L, Arcila ME et al (2015) Broad, hybrid capture-based next-generation sequencing identifies actionable genomic alterations in lung adenocarcinomas otherwise negative for such alterations by other genomic testing approaches. Clin Cancer Res 21(16):3631–3639
Garofalo A, Sholl L, Reardon B et al (2016) The impact of tumor profiling approaches and genomic data strategies for cancer precision medicine. Genome Med 8(1):79
Roszik J, Haydu LE, Hess KR et al (2016) Novel algorithmic approach predicts tumor mutation load and correlates with immunotherapy clinical outcomes using a defined gene mutation set. BMC Med 14(1):168
Merino DM, McShane LM, Fabrizio D et al (2020) Establishing guidelines to harmonize tumor mutational burden (TMB): in silico assessment of variation in TMB quantification across diagnostic platforms: phase I of the Friends of Cancer Research TMB Harmonization Project. J Immunother Cancer 8(1):e000147
Sunami K, Ichikawa H, Kubo T et al (2019) Feasibility and utility of a panel testing for 114 cancer-associated genes in a clinical setting: a hospital-based study. Cancer Sci 110:1480–1490
Bachet JB, Bouché O, Taieb J et al (2018) RAS mutation analysis in circulating tumor DNA from patients with metastatic colorectal cancer: the AGEO RASANC prospective multicenter study. Ann Oncol 29(5):1211–1219
Parikh AR, Leshchiner I, Elagina L et al (2019) Liquid versus tissue biopsy for detecting acquired resistance and tumor heterogeneity in gastrointestinal cancers. Nat Med 25:1415–1421
Lawrence MS, Stojanov P, Polak P et al (2013) Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature 499(7457):214–218
Chan TA, Yarchoan M, Jaffee E et al (2019) Development of tumor mutation burden as an immunotherapy biomarker: utility for the oncology clinic. Ann Oncol 30(1):44–56
Yoshino T, Pentheroudakis G, Mishima S et al (2020) JSCO-ESMO-ASCO-JSMO-TOS: international expert consensus recommendations for tumour-agnostic treatments in patients with solid tumours with microsatellite instability or NTRK fusions. Ann Oncol 31(7):861–872
Haricharan S, Bainbridge MN, Scheet P et al (2014) Somatic mutation load of estrogen receptor-positive breast tumors predicts overall survival: an analysis of genome sequence data. Breast Cancer Res Treat 146:211–220
Gandara DR, Paul SM, Kowanetz M et al (2018) Blood-based tumor mutational burden as a predictor of clinical benefit in non-small-cell lung cancer patients treated with atezolizumab. Nat Med 24(9):1441–1448
Yoshino T, Tukachinsky H, Lee JK et al (2021) Genomic immunotherapy (IO)biomarkers detected on comprehensive genomic profiling (CGP)of tissue and circulating tumor DNA (ctDNA). J Clin Oncol 39(suppl 15):abstr2541
Sturgill E, Misch A, Jones C et al (2021) Concordance of blood and tissue TMB from NGS testing in real-world settings and their ability to predict response to immunotherapy. J Clin Oncol 39(suppl 15):abstr1540
Oh Y, Park J, Chung L et al (2022) Exploring real-world concordance of tumor mutation burden (TMB) from blood and tissue in patient. JITC 10(suppl 2):abstr14
Rooney MS, Shukla SA, Wu CJ et al (2015) Molecular and genetic properties of tumors associated with local immune cytolytic activity. Cell 160(1–2):48–61
Ott PA, Bang YJ, Piha-Paul SA et al (2019) T-cell-inflamed gene-expression profile, programmed death ligand 1 expression, and tumor mutational burden predict efficacy in patients treated with pembrolizumab across 20 cancers: KEYNOTE-028. J Clin Oncol 37(4):318–327
Samstein RM, Lee CH, Shoushtari AN et al (2019) Tumor mutational load predicts survival after immunotherapy across multiple cancer types. Nat Genet 51(2):202–206
Yarchoan M, Hopkins A, Jaffee EM (2017) Tumor mutational burden and response rate to PD-1 inhibition. N Engl J Med 377(25):2500–2501
Marabelle A, Fakih M, Lopez J et al (2020) Association of tumour mutational burden with outcomes in patients with advanced solid tumours treated with pembrolizumab: prospective bio- marker analysis of the multicohort, open-label, phase 2 KEYNOTE-158 study. Lancet Oncol 21(10):1353–1365
Meiri E, Garret-Mayer E, Halabi S et al (2020) Pembrolizumab (P) in patients (Pts) with colorectal cancer (CRC) with high tumor mutational burden (HTMB): Results from the Targeted Agent and Profiling Utilization Registry (TAPUR) Study. J Clin Oncol 38(suppl 4):abstr133
Alva AS, Manget PK, Garrett-Mayer E et al (2021) Pembrolizumab in patients with metastatic breast cancer with high tumor mutational burden: results from the targeted agent and profiling utilization registry (TAPUR) study. J Clin Oncol 39(22):2443–2451
McGrail DJ, Pilié PG, Rashidd NU et al (2021) High tumor mutation burden fails to predict immune checkpoint blockade response across all cancer types. Ann Oncol 32(5):661–672
Valero C, Lee M, Hoen D et al (2021) Response rates to anti-PD-1 immunotherapy in microsatellite-stable solid tumors with 10 or more mutations per megabase. JAMA Oncol 7(5):739–743
Touat M, Li YY, Boynton AN et al (2020) Mechanisms and therapeutic implications of hypermutation in gliomas. Nature 580(7804):517–523
Khagi Y, Goodman AM, Daniels GA et al (2017) Hypermutated circulating tumor DNA: correlation with response to checkpoint inhibitor-based immunotherapy. Clin Cancer Res 23:5729–5736
Eggermont AMM, Blank CU, Mandala M et al (2018) Adjuvant pembrolizumab versus placebo in resected stage III melanoma. N Engl J Med 378(19):1789–1801
Romano E, Scordo M, Dusza SW et al (2010) Site and timing of first relapse in stage III melanoma patients: implications for follow-up guidelines. J Clin Oncol 28(18):3042–3047
Antonia SJ, Villegas A, Daniel D et al (2018) Overall survival with durvalumab after chemoradiotherapy in stage III NSCLC. N Engl J Med 379(24):2342–2350
Kelly RJ, Ajani JA, Kuzdzal J et al (2021) Adjuvant nivolumab in resected esophageal or gastroesophageal junction cancer. N Engl J Med 384(13):1191–1203
Acknowledgements
This guideline was led by Japan Society of Clinical Oncology (JSCO)/Japanese Society of Medical Oncology (JSMO)/Japanese Society of Pediatric Hematology/Oncology (JSPHO). The authors would like to thank Prof. Ishioka, the President of JSMO, and Ms. Nishizawa at the secretariat of JSMO for their on-site assistance. The authors would like to thank Prof. Doki, the President of JSCO, and the secretariat of JSCO. The authors would like to thank Prof. Ohga, the President of JSPHO, and the secretariat of JSPHO. The authors would like to thank BIC (www.bic.co.jp) for the English language review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All committee members and peer review members were nominated by each society, and the conflict of interest (COI) control is conducted by each society’s regulation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Mishima, S., Naito, Y., Akagi, K. et al. Japanese Society of Medical Oncology/Japan Society of Clinical Oncology/Japanese Society of Pediatric Hematology/Oncology-led clinical recommendations on the diagnosis and use of immunotherapy in patients with high tumor mutational burden tumors. Int J Clin Oncol 28, 941–955 (2023). https://doi.org/10.1007/s10147-023-02360-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-023-02360-8