Abstract
Background
There is a sex disparity in papillary thyroid cancer (PTC). Male sex is associated with a higher likelihood of advanced stage disease. This study aimed to examine the significance of sex for extranodal extension (ENE) in PTC.
Methods
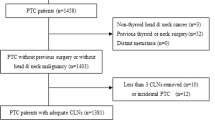
We reviewed the data of PTC patients who had undergone initial surgical resection from July 2012 to December 2014 (N = 1531). The effects of sex and other clinicopathological factors on ENE were investigated.
Results
Of 1531 patients identified, 377 (24.6%) were male, 816 (53.3%) had positive nodes, and 256 (16.7%) had ENE. Compared with female patients, male patients had a higher risk of ENE (P < 0.001). Multivariable analysis of clinicopathological factors revealed that male sex (odds ratio [OR], 1.98; 95% confidence interval [CI], 1.37–2.87; P < 0.001), age older than 60 years (OR, 1.93; 95% CI, 1.08–3.35; P = 0.023), extrathyroidal extension (OR, 3.52; 95% CI, 2.42–5.14; P < 0.001), bilateral multifocality (OR, 2.18; 95% CI, 1.53–3.13; P < 0.001), and more positive nodes were significantly associated with increased risk of ENE. Patients with 6–10 positive nodes were 16.45-fold higher to have ENE than patients with 5 positive nodes or less (95% CI, 11.07–24.68; P < 0.001).
Conclusion
Male PTC patients had a higher risk of ENE than female. Sex was an independent predictor of ENE. The underlying mechanism needs to be investigated further.

Similar content being viewed by others
References
Jeon MJ, Chun SM, Lee JY et al (2019) Mutational profile of papillary thyroid microcarcinoma with extensive lymph node metastasis. Endocrine 64(1):130–138. https://doi.org/10.1007/s12020-019-01842-y
Kim HI, Hyeon J, Park SY et al (2019) Impact of extranodal extension on risk stratification in papillary thyroid carcinoma. Thyroid 29(7):963–970. https://doi.org/10.1089/thy.2018.0541
Kim K, Zheng X, Kim JK et al (2020) The contributing factors for lateral neck lymph node metastasis in papillary thyroid microcarcinoma (PTMC). Endocrine 69(1):149–156. https://doi.org/10.1007/s12020-020-02251-2
Roh JL, Park JW, Jeong J et al (2017) Extranodal extension of lymph node metastasis as a prognostic indicator of recurrence and survival in papillary thyroid carcinoma. J Surg Oncol 116(4):450–458. https://doi.org/10.1002/jso.24713
Lang BH, Shek TW, Wan KY (2016) Impact of microscopic extra-nodal extension (ENE) on locoregional recurrence following curative surgery for papillary thyroid carcinoma. J Surg Oncol 113(5):526–531. https://doi.org/10.1002/jso.24180
Jonklaas J, Nogueras-Gonzalez G, Munsell M et al (2012) The impact of age and gender on papillary thyroid cancer survival. J Clin Endocrinol Metab 97(6):E878-887. https://doi.org/10.1210/jc.2011-2864
Nilubol N, Zhang L, Kebebew E (2013) Multivariate analysis of the relationship between male sex, disease-specific survival, and features of tumor aggressiveness in thyroid cancer of follicular cell origin. Thyroid 23(6):695–702. https://doi.org/10.1089/thy.2012.0269
Oyer SL, Smith VA, Lentsch EJ (2013) Sex is not an independent risk factor for survival in differentiated thyroid cancer. Laryngoscope 123(11):2913–2919. https://doi.org/10.1002/lary.24018
Micheli A, Ciampichini R, Oberaigner W et al (2009) The advantage of women in cancer survival: an analysis of EUROCARE-4 data. Eur J Cancer 45(6):1017–1027. https://doi.org/10.1016/j.ejca.2008.11.008
Liu C, Chen T, Zeng W et al (2017) Reevaluating the prognostic significance of male gender for papillary thyroid carcinoma and microcarcinoma: a SEER database analysis. Sci Rep 7(1):11412. https://doi.org/10.1038/s41598-017-11788-8
Wang F, Zhao S, Shen X et al (2018) BRAF V600E confers male sex disease-specific mortality risk in patients with papillary thyroid cancer. J Clin Oncol 36(27):2787–2795. https://doi.org/10.1200/jco.2018.78.5097
Kim HI, Hyeon J, Park SY et al (2019) Impact of extranodal extension on risk stratification in papillary thyroid carcinoma. Thyroid. https://doi.org/10.1089/thy.2018.0541
Renfro LA, Goldberg RM, Grothey A et al (2017) Clinical calculator for early mortality in metastatic colorectal cancer: an analysis of patients from 28 clinical trials in the aide et recherche en cancérologie digestive database. J Clin Oncol 35(17):1929–1937. https://doi.org/10.1200/jco.2016.71.5771
Harrell FE Jr (2015) Regression modeling strategies: with applications to linear models, logistic and ordinal regression, and survival analysis. Springer
Ito Y, Miyauchi A, Masuoka H et al (2020) Prognostic value of extranodal tumor extension in papillary thyroid carcinoma: proposal for upstaging of cases with extranodal tumor extension. World J Surg 44(2):638–643. https://doi.org/10.1007/s00268-019-05232-3
Wu MH, Shen WT, Gosnell J et al (2015) Prognostic significance of extranodal extension of regional lymph node metastasis in papillary thyroid cancer. Head Neck 37(9):1336–1343. https://doi.org/10.1002/hed.23747
Dong W, Horiuchi K, Tokumitsu H et al (2019) Time-varying pattern of mortality and recurrence from papillary thyroid cancer: lessons from a long-term follow-up. Thyroid 29(6):802–808. https://doi.org/10.1089/thy.2018.0128
Nam SH, Roh JL, Gong G et al (2018) Nodal factors predictive of recurrence after thyroidectomy and neck dissection for papillary thyroid carcinoma. Thyroid 28(1):88–95. https://doi.org/10.1089/thy.2017.0334
Kim JW, Roh JL, Gong G et al (2017) Extent of extrathyroidal extension as a significant predictor of nodal metastasis and extranodal extension in patients with papillary thyroid carcinoma. Ann Surg Oncol 24(2):460–468. https://doi.org/10.1245/s10434-016-5594-4
Barbosa MP, Momesso D, Bulzico DA et al (2017) Metastatic lymph node characteristics as predictors of recurrence/persistence in the neck and distant metastases in differentiated thyroid cancer. Arch Endocrinol Metabol 61(6):584–589. https://doi.org/10.1590/2359-3997000000307
Chéreau N, Buffet C, Trésallet C et al (2016) Recurrence of papillary thyroid carcinoma with lateral cervical node metastases: Predictive factors and operative management. Surgery 159(3):755–762. https://doi.org/10.1016/j.surg.2015.08.033
Lee HS, Park C, Kim SW et al (2016) Primary tumour characteristics predict the invasiveness of lymph node metastases in papillary thyroid carcinoma patients. J Laryngol Otol 130(3):302–308. https://doi.org/10.1017/s0022215115003382
Rowe ME, Ozbek U, Machado RA et al (2018) The Prevalence of extranodal extension in papillary thyroid cancer based on the size of the metastatic node: adverse histologic features are not limited to larger lymph nodes. Endocr Pathol 29(1):80–85. https://doi.org/10.1007/s12022-018-9518-7
Funding
This study was funded by Henan Health Commission (Grant number 2018020490).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by HH, BZ, WG and CZ. The first draft of the manuscript was written by HH and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have indicated that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Hei, H., Zhou, B., Gong, W. et al. Male patients with papillary thyroid cancer have a higher risk of extranodal extension. Int J Clin Oncol 27, 648–654 (2022). https://doi.org/10.1007/s10147-021-02109-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-021-02109-1