Abstract
Purpose
Papillary thyroid microcarcinoma (PTMC) has an excellent prognosis due to its indolent features. Only few studies have assessed the clinical factors that can predict lateral neck lymph node metastasis (LLNM) in patients with PTMC. This study aimed to examine the clinicopathological factors associated with LLNM in patients with PTMC.
Methods
We reviewed medical records of 3578 patients with PTMC that was ≤1 cm in diameter on final pathology at Yonsei University Hospital between January 2015 and December 2017. The patients were divided into two groups (metastasis group [n = 157] and no metastasis group [n = 3421]).
Results
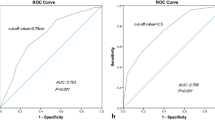
The proportion of patients with multifocality, extrathyroidal extension (ETE), and central node metastasis was significantly higher in metastasis group (p < 0.001, p < 0.001 and p < 0.001, respectively), and the mean tumor size was relatively larger in metastasis group than in no metastasis group (0.7 ± 0.2 vs. 0.6 ± 0.2 cm, p < 0.001). However, no statistically significant differences were observed in the tumors harboring BRAF mutation between the two groups (84.8% vs. 80.6%, p = 0.199). Multivariate analysis indicated that the significant risk factors of LLNM include ETE (odds ratio [OR]: 1.904, 95% confidence interval [CI]: 1.267–2.861), multifocality (OR: 2.255, 95% CI: 1.544–3.293), and central node metastasis (OR: 7.768, 95% CI: 4.869–12.395), but not BRAF mutation (OR: 0.542, 95% CI: 0.337–0.874).
Conclusion
Approximately 4.4% of patients with PTMC presented with LLNM at the time of diagnosis. Moreover, the significant risk factors of LLNM include central node metastasis, ETE, and multifocal disease but not BRAF mutation.
Similar content being viewed by others
References
G. Pellegriti, F. Frasca, C. Regalbuto, S. Squatrito, R. Vigneri, Worldwide increasing incidence of thyroid cancer: update on epidemiology and risk factors. J. Cancer Epidemiol. 2013, 965212 (2013)
J.D. Cramer, P. Fu, K.C. Harth, S. Margevicius, S.M. Wilhelm, Analysis of the rising incidence of thyroid cancer using the Surveillance, Epidemiology and End Results national cancer data registry. Surgery 148(6), 1147–1153 (2010)
A.Y. Chen, A. Jemal, E.M. Ward, Increasing incidence of differentiated thyroid cancer in the United States, 1988–2005. Cancer 115(16), 3801–3807 (2009)
L. Davies, H.G. Welch, Increasing incidence of thyroid cancer in the United States, 1973–2002. Jama 295(18), 2164–2167 (2006)
J. Schönberger, J. Marienhagen, A. Agha, S. Rozeboom, E. Bachmeier, H. Schlitt, C. Eilles, Papillary microcarcinoma and papillary cancer of the thyroid ≤1 cm. Nuklearmedizin 46(04), 115–120 (2007)
C. Hedinger, E. Dillwyn Williams, L.H. Sobin, The WHO histological classification of thyroid tumors: a commentary on the second edition. Cancer 63(5), 908–911 (1989)
A. Toniato, I. Boschin, D. Casara, R. Mazzarotto, D. Rubello, M. Pelizzo, Papillary thyroid carcinoma: factors influencing recurrence and survival. Ann. Surg. Oncol. 15(5), 1518–1522 (2008)
I. Sugitani, K. Toda, K. Yamada, N. Yamamoto, M. Ikenaga, Y.Fujimoto, Three distinctly different kinds of papillary thyroid microcarcinoma should be recognized: our treatment strategies and outcomes. World J. Surg. 34(6), 1222–1231 (2010)
W. Lang, H. Borrusch, L. Bauer, Occult carcinomas of the thyroid: evaluation of 1,020 sequential autopsies. Am. J. Clin. Pathol. 90(1), 72–76 (1988)
Y. Yamamoto, T. Maeda, K. Izumi, H. Otsuka, Occult papillary carcinoma of the thyroid. A study of 408 autopsy cases. Cancer 65(5), 1173–1179 (1990)
N. Wada, Q.-Y. Duh, K. Sugino, H. Iwasaki, K. Kameyama, T. Mimura, K. Ito, H. Takami, Y. Takanashi, Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann. Surg. 237(3), 399 (2003)
J.-L. Roh, J.-M. Kim, C.I. Park, Central cervical nodal metastasis from papillary thyroid microcarcinoma: pattern and factors predictive of nodal metastasis. Ann. Surg. Oncol. 15(9), 2482 (2008)
Y.K. So, Y.-I. Son, S.D. Hong, M.Y. Seo, C.-H. Baek, H.-S. Jeong, M.K. Chung, Subclinical lymph node metastasis in papillary thyroid microcarcinoma: a study of 551 resections. Surgery 148(3), 526–531 (2010)
J.Y. Kwak, E.-K. Kim, M.J. Kim, E.J. Son, W.Y. Chung, C.S. Park, K.-H. Nam, Papillary microcarcinoma of the thyroid: predicting factors of lateral neck node metastasis. Ann. Surg. Oncol. 16(5), 1348 (2009)
Y.S. Kim, Patterns and predictive factors of lateral lymph node metastasis in papillary thyroid microcarcinoma. Otolaryngol. Head. Neck Surg. 147(1), 15–19 (2012)
B.R. Haugen, E.K. Alexander, K.C. Bible, G.M. Doherty, S.J. Mandel, Y.E. Nikiforov, F. Pacini, G.W. Randolph, A.M. Sawka, M. Schlumberger, K.G. Schuff, S.I. Sherman, J.A. Sosa, D.L. Steward, R.M. Tuttle, L. Wartofsky, 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26(1), 1–133 (2016)
C.R. McHenry, I.B. Rosen, P.G. Walfish, Prospective management of nodal metastases in differentiated thyroid cancer. Am. J. Surg. 162(4), 353–356 (1991)
L.A. Akslen, T. Haldorsen, S.Ø. Thoresen, E. Glattre, Survival and causes of death in thyroid cancer: a population-based study of 2479 cases from Norway. Cancer Res. 51(4), 1234–1241 (1991)
H. Namba, M. Nakashima, T. Hayashi, N. Hayashida, S. Maeda, T.I. Rogounovitch, A. Ohtsuru, V.A. Saenko, T. Kanematsu, S. Yamashita, Clinical implication of hot spot BRAF mutation, V599E, in papillary thyroid cancers. J. Clin. Endocrinol. Metab. 88(9), 4393–4397 (2003)
K.H. Kim, D.W. Kang, S.H. Kim, I.O. Seong, D.Y. Kang, Mutations of the BRAF gene in papillary thyroid carcinoma in a Korean population. Yonsei Med. J. 45, 818–821 (2004)
E. Puxeddu, S. Moretti, R. Elisei, C. Romei, R. Pascucci, M. Martinelli, C. Marino, N. Avenia, E.D. Rossi, G. Fadda, BRAFV599E mutation is the leading genetic event in adult sporadic papillary thyroid carcinomas. J. Clin. Endocrinol. Metab. 89(5), 2414–2420 (2004)
K.T. Robbins, J.E. Medina, G.T. Wolfe, P.A. Levine, R.B. Sessions, C.W. Pruet, Standardizing neck dissection terminology: official report of the Academy’s Committee for Head and Neck Surgery and Oncology. Arch. Otolaryngol. Head. Neck Surg. 117(6), 601–605 (1991)
J. Lee, T.-Y. Sung, K.-H. Nam, W.Y. Chung, E.-Y. Soh, C.S.Park, Is level IIb lymph node dissection always necessary in N1b papillary thyroid carcinoma patients? World J. Surg. 32(5), 716–721 (2008)
N. Caron, Y. Tan, J. Ogilvie, F. Triponez, E. Reiff, E. Kebebew, Q. Duh, O.H.Clark, Selective modified radical neck dissection for papillary thyroid cancer-is level I, II and V dissection always necessary? World J. Surg. 30(5), 833–840 (2006
H.S. Ahn, H.J. Kim, H.G. Welch, Korea’s thyroid-cancer “epidemic”—screening and overdiagnosis. N. Engl. J. Med. 371(19), 1765–1767 (2014)
N. Besic, J. Zgajnar, M. Hocevar, Extent of thyroidectomy and lymphadenectomy in 254 patients with papillary thyroid microcarcinoma: a single-institution experience. Ann. Surg. Oncol. 16(4), 920–928 (2009)
M. Goran, T. Pekmezovic, I. Markovic, N. Santrac, M. Buta, D. Gavrilovic, N. Besic, Y. Ito, I. Djurisic, G. Pupic, Lymph node metastases in clinically N0 patients with papillary thyroid microcarcinomas-a single institution experience. J. BUON 22(1), 224–231 (2017)
S.Y. Choi, H. Park, M.K. Kang, D.K. Lee, K.D. Lee, H.S. Lee, S.W. Kim, E.N. Lee, J.C. Hong, The relationship between the BRAF V600E mutation in papillary thyroid microcarcinoma and clinicopathologic factors. World J. Surg. Oncol. 11(1), 291 (2013)
T.Y. Kim, W.B. Kim, J.Y. Song, Y.S. Rhee, G. Gong, Y.M. Cho, S.Y. Kim, S.C. Kim, S.J. Hong, Y.K. Shong, The BRAFV600E mutation is not associated with poor prognostic factors in Korean patients with conventional papillary thyroid microcarcinoma. Clin. Endocrinol. (Oxf.) 63(5), 588–593 (2005)
J.Y. Kwak, E.-K. Kim, W.Y. Chung, H.J. Moon, M.J. Kim, J.R. Choi, Association of BRAFV600E mutation with poor clinical prognostic factors and US features in Korean patients with papillary thyroid microcarcinoma. Radiology 253(3), 854–860 (2009)
K.-L. Lin, O.-C. Wang, X.-H. Zhang, X.-X. Dai, X.-Q. Hu, J.-M. Qu, The BRAF mutation is predictive of aggressive clinicopathological characteristics in papillary thyroid microcarcinoma. Ann. Surg. Oncol. 17(12), 3294–3300 (2010)
Y. Chen, P.M. Sadow, H. Suh, K.E. Lee, J.Y. Choi, Y.J. Suh, T.S. Wang, C.C. Lubitz, BRAFV600E is correlated with recurrence of papillary thyroid microcarcinoma: a systematic review, multi-institutional primary data analysis, and meta-analysis. Thyroid 26(2), 248–255 (2016)
X. Liu, S. Qu, R. Liu, C. Sheng, X. Shi, G. Zhu, A.K. Murugan, H. Guan, H. Yu, Y. Wang, TERT promoter mutations and their association with BRAF V600E mutation and aggressive clinicopathological characteristics of thyroid cancer. J. Clin. Endocrinol. Metab. 99(6), E1130–E1136 (2014)
X. Zheng, S. Wei, Y. Han, Y. Li, Y. Yu, X. Yun, X. Ren, M. Gao, Papillary microcarcinoma of the thyroid: clinical characteristics and BRAFV600E mutational status of 977 cases. Ann. Surg. Oncol. 20(7), 2266–2273 (2013)
A.U. Bastos, G. Oler, B.H.N. Nozima, R.A. Moysés, J.M. Cerutti, BRAF V600E and decreased NIS and TPO expression are associated with aggressiveness of a subgroup of papillary thyroid microcarcinoma. Eur. J. Endocrinol. 173(4), 525–540 (2015)
J.R. George, Y.C. Henderson, M.D. Williams, D.B. Roberts, H. Hei, S.Y. Lai, G.L. Clayman, Association of TERT promoter mutation, but not BRAF mutation, with increased mortality in PTC. J. Clin. Endocrinol. Metab. 100(12), E1550–E1559 (2015)
Y. Ito, H. Yoshida, R. Maruo, S. Morita, T. Takano, M. Hirokawa, T. Yabuta, M. Fukushima, H. Inoue, C. Tomoda, BRAF mutation in papillary thyroid carcinoma in a Japanese population: its lack of correlation with high-risk clinicopathological features and disease-free survival of patients. Endocr. J. 56(1), 89–97 (2009)
A. Nasirden, T. Saito, Y. Fukumura, K. Hara, K. Akaike, A. Kurisaki-Arakawa, M. Asahina, A. Yamashita, R. Tomomasa, T. Hayashi, In Japanese patients with papillary thyroid carcinoma, TERT promoter mutation is associated with poor prognosis, in contrast to BRAF V600E mutation. Virchows Arch. 469(6), 687–696 (2016)
S. Moon, Y.S. Song, Y.A. Kim, J.A. Lim, S.W. Cho, J.H. Moon, S. Hahn, D.J. Park, Y.J. Park, Effects of coexistent BRAFV600E and TERT promoter mutations on poor clinical outcomes in papillary thyroid cancer: a meta-analysis. Thyroid 27(5), 651–660 (2017)
J.-H. Lee, R.-Y. Song, J.W. Yi, H.W. Yu, H. Kwon, S.-j Kim, Y.J. Chai, J.Y. Choi, J.H. Moon, K.E. Lee, Case–control study of papillary thyroid carcinoma on urinary and dietary iodine status in South Korea. World J. Surg. 42(5), 1424–1431 (2018)
H.J. Kim, H.K. Park, D.W. Byun, K. Suh, M.H. Yoo, Y.-K. Min, S.W. Kim, J.H. Chung, Iodine intake as a risk factor for BRAF mutations in papillary thyroid cancer patients from an iodine-replete area. Eur. J. Nutr. 57(2), 809–815 (2018)
M. Wang, W.-D. Wu, G.-M. Chen, S.-L. Chou, X.-M. Dai, J.-M. Xu, Z.-H. Peng, Could tumor size be a predictor for papillary thyroid microcarcinoma: a retrospective cohort study. Asian Pac. J. Cancer Prev. 16(18), 8625–8628 (2015)
Y. Gong, G. Li, J. Lei, J. You, K. Jiang, Z. Li, R. Gong, J. Zhu, A favorable tumor size to define papillary thyroid microcarcinoma: an analysis of 1176 consecutive cases. Cancer Manag. Res. 10, 899 (2018)
C. Liu, S. Wang, W. Zeng, Y. Guo, Z. Liu, T. Huang, Total tumour diameter is superior to unifocal diameter as a predictor of papillary thyroid microcarcinoma prognosis. Sci. Rep. 7(1), 1846 (2017)
A.A. Tam, D. Özdemir, N. Çuhacı, H. Başer, A. Dirikoç, C. Aydın, A.K. Yazgan, R. Ersoy, B. Çakır, Can ratio of the biggest tumor diameter to total tumor diameter be a new parameter in the differential diagnosis of agressive and favorable multifocal papillary thyroid microcarcinoma? Oral. Oncol. 65, 1–7 (2017)
Q. Zhao, J. Ming, C. Liu, L. Shi, X. Xu, X. Nie, T. Huang, Multifocality and total tumor diameter predict central neck lymph node metastases in papillary thyroid microcarcinoma. Ann. Surg. Oncol. 20(3), 746–752 (2013)
N.G. Iyer, A.R. Shaha, Central compartment dissection for well differentiated thyroid cancer… and the band plays on. Curr. Opin. Otolaryngol. Head. Neck Surg. 19(2), 106–112 (2011)
S.E. Carty, D.S. Cooper, G.M. Doherty, Q.-Y. Duh, R.T. Kloos, S.J. Mandel, G.W. Randolph, Jr,B.C. Stack, D.L. Steward, D.J. Terris, Consensus statement on the terminology and classification of central neck dissection for thyroid cancer: the American thyroid association surgery working group with participation from the American association of endocrine surgeons, American academy of otolaryngology—head and neck surgery, and American head and neck society. Thyroid 19(11), 1153–1158 (2009)
Acknowledgements
This study was supported by a faculty research grant of Yonsei University College of Medicine (6–2018–0044).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Kim, K., Zheng, X., Kim, J.K. et al. The contributing factors for lateral neck lymph node metastasis in papillary thyroid microcarcinoma (PTMC). Endocrine 69, 149–156 (2020). https://doi.org/10.1007/s12020-020-02251-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-020-02251-2