Abstract
Background
Malignant tumor essentially implies structural heterogeneity. Analysis of medical imaging can quantify this structural heterogeneity, which can be a new biomarker. This study aimed to evaluate the usefulness of texture analysis of computed tomography (CT) imaging as a biomarker for predicting the therapeutic response of neoadjuvant chemoradiotherapy (nCRT) for locally advanced rectal cancer.
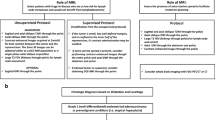
Methods
We enrolled 76 patients with rectal cancer who underwent curative surgery after nCRT. Texture analyses (Fractal analysis and Histogram analysis) were applied to contrast-enhanced CT images, and fractal dimension (FD), skewness, and kurtosis of the tumor were calculated. These CT-derived parameters were compared with the therapeutic response and prognosis.
Results
Forty-six of 76 patients were diagnosed as clinical responders after nCRT. Kurtosis was significantly higher in the responders group than in the non-responders group (4.17 ± 4.16 vs. 2.62 ± 3.19, p = 0.04). Nine of 76 patients were diagnosed with pathological complete response (pCR) after surgery. FD of the pCR group was significantly lower than that of the non-pCR group (0.90 ± 0.12 vs. 1.01 ± 0.12, p = 0.009). The area under the receiver-operating characteristics curve of tumor FD for predicting pCR was 0.77, and the optimal cut-off value was 0.84 (accuracy; 93.4%). Furthermore, patients with lower FD tumors tended to show better relapse-free survival and disease-specific survival than those with higher FD tumors (5-year, 80.8 vs. 66.6%, 94.4 vs. 80.2%, respectively), although it was not statistically significant (p = 0.14, 0.11).
Conclusions
CT-derived texture parameters could be potential biomarkers for predicting the therapeutic response of rectal cancer.





Similar content being viewed by others
Change history
11 October 2021
The original article has been revised due to removal underlined entries in Table 1.
References
Sauer R, Becker H, Hohenberger W et al (2004) Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 351(17):1731–1740. https://doi.org/10.1056/NEJMoa040694
Roh MS, Colangelo LH, O’Connell MJ et al (2009) Preoperative multimodality therapy improves disease-free survival in patients with carcinoma of the rectum: NSABP R-03. J Clin Oncol 27(31):5124–5130. https://doi.org/10.1200/jco.2009.22.0467
Habr-Gama A, Sabbaga J, Gama-Rodrigues J et al (2013) Watch and wait approach following extended neoadjuvant chemoradiation for distal rectal cancer: are we getting closer to anal cancer management? Dis Colon Rectum 56(10):1109–1117. https://doi.org/10.1097/DCR.0b013e3182a25c4e
Habr-Gama A, Gama-Rodrigues J, São Julião GP et al (2014) Local recurrence after complete clinical response and watch and wait in rectal cancer after neoadjuvant chemoradiation: impact of salvage therapy on local disease control. Int J Radiat Oncol Biol Phys 88(4):822–828. https://doi.org/10.1016/j.ijrobp.2013.12.012
Hashiguchi Y, Muro K, Saito Y et al (2020) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol 25(1):1–42. https://doi.org/10.1007/s10147-019-01485-z
Chee CG, Kim YH, Lee KH et al (2017) CT texture analysis in patients with locally advanced rectal cancer treated with neoadjuvant chemoradiotherapy: a potential imaging biomarker for treatment response and prognosis. PLoS One 12(8):e0182883. https://doi.org/10.1371/journal.pone.0182883
Cusumano D, Dinapoli N, Boldrini L et al (2018) Fractal-based radiomic approach to predict complete pathological response after chemo-radiotherapy in rectal cancer. Radiol Med (Torino) 123(4):286–295. https://doi.org/10.1007/s11547-017-0838-3
van Stiphout RG, Valentini V, Buijsen J et al (2014) Nomogram predicting response after chemoradiotherapy in rectal cancer using sequential PETCT imaging: a multicentric prospective study with external validation. Radiother Oncol 113(2):215–222. https://doi.org/10.1016/j.radonc.2014.11.002
Lino-Silva LS, Salcedo-Hernández RA, Ruiz-García EB et al (2016) Pre-operative neutrophils/lymphocyte ratio in rectal cancer patients with preoperative chemoradiotherapy. Medical archives (Sarajevo, Bosnia and Herzegovina) 70(4):256–260. https://doi.org/10.5455/medarh.2016.70.256-260
Miyakita H, Sadahiro S, Saito G et al (2017) Risk scores as useful predictors of perioperative complications in patients with rectal cancer who received radical surgery. Int J Clin Oncol 22(2):324–331. https://doi.org/10.1007/s10147-016-1054-1
Carruthers R, Tho LM, Brown J et al (2012) Systemic inflammatory response is a predictor of outcome in patients undergoing preoperative chemoradiation for locally advanced rectal cancer. Colorectal Dis 14(10):e701-707. https://doi.org/10.1111/j.1463-1318.2012.03147.x
Kim TG, Park W, Kim H et al (2019) Baseline neutrophil–lymphocyte ratio and platelet-lymphocyte ratio in rectal cancer patients following neoadjuvant chemoradiotherapy. Tumori 105(5):434–440. https://doi.org/10.1177/0300891618792476
Lopes-Ramos C, Koyama FC, Habr-Gama A et al (2015) Comprehensive evaluation of the effectiveness of gene expression signatures to predict complete response to neoadjuvant chemoradiotherapy and guide surgical intervention in rectal cancer. Cancer Genet 208(6):319–326. https://doi.org/10.1016/j.cancergen.2015.03.010
Marusyk A, Almendro V, Polyak K (2012) Intra-tumour heterogeneity: a looking glass for cancer? Nat Rev Cancer 12(5):323–334. https://doi.org/10.1038/nrc3261
Turner NC, Reis-Filho JS (2012) Genetic heterogeneity and cancer drug resistance. Lancet Oncol 13(4):e178-185. https://doi.org/10.1016/s1470-2045(11)70335-7
Gerlinger M, Rowan AJ, Horswell S et al (2012) Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N Engl J Med 366(10):883–892. https://doi.org/10.1056/NEJMoa1113205
Aker M, Ganeshan B, Afaq A et al (2019) Magnetic resonance texture analysis in identifying complete pathological response to Neoadjuvant treatment in locally advanced rectal cancer. Dis Colon Rectum 62(2):163–170. https://doi.org/10.1097/dcr.0000000000001224
Mahadevan LS, Zhong J, Venkatesulu B et al (2018) Imaging predictors of treatment outcomes in rectal cancer: an overview. Crit Rev Oncol Hematol 129:153–162. https://doi.org/10.1016/j.critrevonc.2018.06.009
Ma X, Shen F, Jia Y et al (2019) MRI-based radiomics of rectal cancer: preoperative assessment of the pathological features. BMC Med Imaging 19(1):86. https://doi.org/10.1186/s12880-019-0392-7
Hirata A, Hayano K, Ohira G et al (2020) Volumetric histogram analysis of apparent diffusion coefficient for predicting pathological complete response and survival in esophageal cancer patients treated with chemoradiotherapy. Am J Surg 219(6):1024–1029. https://doi.org/10.1016/j.amjsurg.2019.07.040
Hirata A, Hayano K, Ohira G et al (2020) Volumetric histogram analysis of apparent diffusion coefficient as a biomarker to predict survival of Esophageal cancer patients. Ann Surg Oncol 27(8):3083–3089. https://doi.org/10.1245/s10434-020-08270-7
Hayano K, Yoshida H, Zhu AX et al (2014) Fractal analysis of contrast-enhanced CT images to predict survival of patients with hepatocellular carcinoma treated with sunitinib. Dig Dis Sci 59(8):1996–2003. https://doi.org/10.1007/s10620-014-3064-z
Hayano K, Lee SH, Yoshida H et al (2014) Fractal analysis of CT perfusion images for evaluation of antiangiogenic treatment and survival in hepatocellular carcinoma. Acad Radiol 21(5):654–660. https://doi.org/10.1016/j.acra.2014.01.020
Marusina MY, Mochalina AP, Frolova EP et al (2017) MRI image processing based on fractal analysis. Asian Pac J Cancer Prev 18(1):51–55. https://doi.org/10.22034/apjcp.2017.18.1.51
Kurata Y, Hayano K, Ohira G et al (2018) Fractal analysis of contrast-enhanced CT images for preoperative prediction of malignant potential of gastrointestinal stromal tumor. Abdom Radiol (New York) 43(10):2659–2664. https://doi.org/10.1007/s00261-018-1526-z
Watanabe H, Hayano K, Ohira G et al (2020) Quantification of structural heterogeneity using fractal analysis of contrast-enhanced CT image to predict survival in gastric cancer patients. Dig Dis Sci. https://doi.org/10.1007/s10620-020-06479-w
Takahashi Y, Hayano K, Ohira G et al (2020) Histogram analysis of diffusion-weighted MR imaging as a biomarker to predict survival of surgically treated colorectal cancer patients. Dig Dis Sci. https://doi.org/10.1007/s10620-020-06318-y
Eisenhauer EA, Therasse P, Bogaerts J et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer (Oxford, England: 1990) 45(2):228–247. https://doi.org/10.1016/j.ejca.2008.10.026
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48(3):452–458. https://doi.org/10.1038/bmt.2012.244
Liu S, Jiang T, Xiao L et al (2021) Total Neoadjuvant Therapy (TNT) versus standard neoadjuvant chemoradiotherapy for locally advanced rectal cancer: a systematic review and meta-analysis. Oncologist. https://doi.org/10.1002/onco.13824
Hayano K, Ohira G, Hirata A et al (2019) Imaging biomarkers for the treatment of esophageal cancer. World J Gastroenterol 25(24):3021–3029. https://doi.org/10.3748/wjg.v25.i24.3021
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No author has any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Kurata, Y., Hayano, K., Ohira, G. et al. Computed tomography-derived biomarker for predicting the treatment response to neoadjuvant chemoradiotherapy of rectal cancer. Int J Clin Oncol 26, 2246–2254 (2021). https://doi.org/10.1007/s10147-021-02027-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-021-02027-2