Abstract
This systematic review and meta-analysis aimed to assess the prognostic value of preoperative hematologic biomarkers in patients with urothelial carcinoma of the bladder treated with radical cystectomy. PUBMED, Web of Science, Cochrane Library, and Scopus databases were searched in September 2019 according to the Preferred Reporting Items for Systematic Review and Meta-analysis statement. Studies were deemed eligible if they compared cancer-specific survival in patients with urothelial carcinoma of the bladder with and without pretreatment laboratoryabnormalities. Formal meta-analyses were performed for this outcome. The systematic review identified 36 studies with 23,632 patients, of these, 32 studies with 22,224 patients were eligible for the meta-analysis. Several preoperative hematologic biomarkers were significantly associated with cancer-specific survival as follows: neutrophil − lymphocyte ratio (pooled hazard ratio [HR]: 1.20, 95% confidence interval [CI]: 1.11–1.29), hemoglobin (pooled HR: 0.87, 95% CI 0.82–0.94), C-reactive protein (pooled HR: 1.44, 95% CI 1.26–1.66), De Ritis ratio (pooled HR: 2.18, 95% CI 1.37–3.48), white blood cell count (pooled HR: 1.05, 95% CI 1.02–1.07), and albumin-globulin ratio (pooled HR: 0.26, 95% CI 0.14–0.48). Several pretreatment laboratory abnormalities in patients with urothelial carcinoma of the bladder were associated with cancer-specific mortality. Therefore, it might be useful to incorporate such hematologic biomarkers into prognostic tools for urothelial carcinoma of the bladder. However, given the study limitations including heterogeneity and retrospective nature of the primary data, the conclusions should be interpreted with caution.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urothelial carcinoma of the bladder (UCB) is the ninth most commonly diagnosed cancer worldwide [1]. Radical cystectomy (RC) with lymph node dissection is the mainstay treatment for very high-risk non-muscle-invasive and muscle-invasive UCB [2, 3]. Despite definitive therapy with curative intent, the 5-year overall survival of patients remains below 60% [4, 5]. Thus, various clinical and pathologic factors have been identified to assist in the risk stratification of UCB patients, thereby facilitating clinical decision-making regarding treatment intensification, follow-up and patient counselling [6, 7]. Currently, the majority of these factors are pathological features such as tumor stage, grade, lymph node status, concomitant carcinoma in situ, variant histology, surgical margin status, and lymphovascular invasion. Unfortunately, the accuracy of outcome prediction with these factors remains suboptimal, probably due to their failure to capture the full biologic potential of host-tumor interactions [8]. In addition, clinical, radiologic, and pre-RC pathologic factors have significant limitations, and do not allow for optimal clinical decision making [6, 9]. Therefore, there remains a need to identify other potential prognostic markers, in particular preoperatively, to improve the stratification of patients with muscle-invasive UCB.
Recently, there has been a surge of interest in the prognostic role of hematologic biomarkers in patients undergoing RC. Current research has suggested that hematologic biomarkers, such as neutrophil–lymphocyte ratio (NLR), C-reactive protein (CRP), lymphocyte-monocyte ratio (LMR), platelet-lymphocyte ratio (PLR), and hemoglobin (Hb), may have prognostic value in patients with UCB [3, 10]. However, the prognostic significance of hematologic biomarkers remains to be established in UCB treated with RC. Therefore, this systematic review and meta-analysis were conducted to summarize the available evidence as well as to determine whether preoperative hematologic biomarkers may help predict oncological outcomes in patients with UCB treated with RC. If such biomarkers are predictive of outcomes in this patient population, a panel of these markers could help identify and classify patients, as well as aid in the selection of patients for novel therapies that rely heavily on host-tumor interaction.
Methods
Search strategy
The systematic review and meta-analysis were performed according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement [11]. The PubMed, Web of Science, Cochrane Library, and Scopus databases were searched in September 2019 to identify reports on the prognostic value of blood-based biomarkers in UCB. The keywords used in our search strategy were: (cystectomy) AND (multivariate OR multivariable) AND (survival OR mortality): The primary outcome of interest was cancer-specific survival (CSS). Initial screening was performed independently by two investigators based on the titles and abstracts to identify ineligible reports, and reasons for exclusions were noted. Potentially relevant reports were subjected to a full-text review and the relevance of the reports was also confirmed after the data extraction process. Disagreements were resolved via consensus with the additional investigator.
Inclusion and exclusion criteria
Studies were included if they investigated patients treated for UCB with preoperative laboratory abnormalities (Patients) who had received radical cystectomy (Intervention) compared to those without preoperative laboratory abnormalities (Comparison) to assess the independent predictive value of blood-based biomarkers on CSS (Outcome) utilizing multivariate Cox regression analysis (Study design) in nonrandomized observational, randomized, or cohort studies. We excluded reviews, letters, editorials, meeting abstracts, replies from authors, case reports and articles not published in English. In cases of duplicate publications, the higher quality or the most recent publication was selected. References of included manuscripts were further scanned for additional studies of interest.
Data extraction
Two investigators independently extracted the following information from the included articles: first author’s name, publication year, recruitment country, period of patient recruitment, number of patients, age, sex, study design, disease stage, oncological outcome, follow-up duration, pathological T stage, adjuvant chemotherapy, neoadjuvant chemotherapy, conclusion, and type of biomarkers. Subsequently, the hazard ratios (HR) and 95% confidence intervals (CI) of blood-based biomarkers associated with each of the outcomes were retrieved. The HRs were extracted from the multivariate analyses and all discrepancies regarding data extraction were resolved by consensus with the additional investigator.
Quality assessment
The Newcastle–Ottawa Scale (NOS) was used to assess the quality of the included studies in accordance with the Cochrane Handbook for systematic reviews of interventions for included non-randomized studies [12, 13]. The scale rates following three factors: Selection (1–4 points), Comparability (1–2 points) and Exposure (1–3 points), with total scores ranging from 0 (lowest) to 9 (highest). The main confounders were identified as the important prognostic factors of CSS. The presence of confounders was determined by consensus and review of the literature. Studies with scores of more than 6 were identified as “high-quality” choices.
Statistical analyses
Forest plots were used to assess the multivariate HRs and summarize them to describe the relationships between blood-based biomarkers and CSS. Studies were not considered in the meta-analysis if they used Kaplan–Meier log-rank, univariate Cox proportional hazard regression, or general logistic regression analyses. In studies with only HRs and P-values, we calculated the corresponding 95% CIs [14, 15]. Heterogeneity among the outcomes of included studies in this meta-analysis was evaluated by using Cochrane’s Q test and the I2 statistic. Significant heterogeneity was indicated by a P < 0.05 in Cochrane’s Q tests and a ratio > 50% in I2 statistics. We used fixed-effects models for the calculation of pooled HRs for non-heterogeneous results [16,17,18]. Publication bias was assessed using funnel plots. All statistical analyses were performed using Stata/MP 14.2 (Stata Corp., College Station, TX); statistical significance level was set at P < 0.05.
Results
Study selection and characteristics
Our initial search identified 4861 records, and after removing of duplicates, 4192 remained (Fig. 1). A total of 4112 articles were excluded after screening the titles and abstracts, and a full-text review was performed for 80 articles. After applying the selection criteria, we identified 36 articles with 23,632 patients for the systematic review, of which, 32 articles with 22,224 patients were used for the meta-analysis [10, 19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53]. The extracted data from the 36 studies are outlined in Tables 1 and 2. All included studies had a retrospective design and were published between 2002 and 2019, with 13 studies being from Europe, 5 from North America, 15 from Asia and 3 from international collaboration. The median age and follow-up ranged from 60.7 to 72 years, and 14 to 132 months, respectively; 19,185 of the studied patients were male and 4447 were female. The studies had a median NOS score of 7 (6–7)0.2329.
Meta-analysis
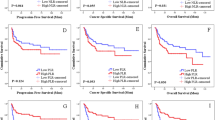
Association of NLR with CSS in UCB
Twelve studies including 11, 158 patients provided data on the association of NLR with CSS in UCB. The forest plot (Fig. 2a) revealed that NLR was significantly associated with CSS in UCB (pooled HR: 1.20, 95% CI 1.11–1.29; z = 4.83). The Cochrane’s Q test (Chi2 = 56.41; P = 0.000) and I2 test (I2 = 80.5%) revealed significant heterogeneity. The funnel plot identified four studies over the pseudo-95% CI (Fig. 3a).
Forest plot (association of hematologic biomarkers with cancer-specific survival). a neutrophil − lymphocyte ratio; b hemoglobin; c platelet; d albumin; e lymphocyte-to-monocyte ratio; f de ritis ratio; g albumin-globulin ratio; h c-reactive protein; i platelet-lymphocyte ratio; j white blood cell; k leukocyte
Funnel plot (association of hematologic biomarkers with cancer-specific survival). a neutrophil − lymphocyte ratio; b hemoglobin; c platelet; d albumin; e lymphocyte-to-monocyte ratio; f de ritis ratio; g albumin-globulin ratio; h c-reactive protein; i platelet-lymphocyte ratio; j white blood cell; k leukocyte
Association of Hb with CSS in UCB
Fourteen studies including 7661 patients provided data on the association of Hb with CSS in UCB. The forest plot (Fig. 2b) revealed that Hb was significantly associated with CSS in UCB (pooled HR, 0.87; 95% CI, 0.82–0.94; z = 3.71). The Cochrane’s Q test (Chi2 = 79.01; P = 0.000) and I2 test (I2 = 83.5%) revealed significant heterogeneity. The funnel plot identified six studies over the pseudo-95% CI (Fig. 3b).
Association of platelet count with CSS in UCB
Six studies including 3, 283 patients provided data on the association of platelet count (Plt) with CSS in UCB. The forest plot (Fig. 2c) revealed that Plt was not significantly associated with CSS in UCB (pooled HR: 1.01, 95% CI 0.98–1.03; z = 0.55). The Cochrane’s Q test (Chi2 = 26.31; P = 0.000) and I2 test (I2 = 81.0%) revealed significant heterogeneity. The funnel plot identified three studies over the pseudo-95% CI (Fig. 3c).
Association of albumin with CSS in UCB
Six studies including 2, 237 patients provided data on the association of albumin (Alb) with CSS in UCB. The forest plot (Fig. 2d) revealed that Alb was not significantly associated with CSS in UCB (pooled HR: 0.93, 95% CI 0.85–1.02; z = 1.45). The Cochrane’s Q test (Chi2 = 5.80; P = 0.327) and I2 test (I2 = 13.7%) revealed no significant heterogeneity. The funnel plot did not identify any studies over the pseudo-95% CI (Fig. 3d).
Association of LMR with CSS in UCB
Three studies including 4644 patients provided data on the association of LMR with CSS in UCB. The forest plot (Fig. 2e) revealed that LMR was not significantly associated with CSS in UCB (pooled HR, 1.12; 95% CI 0.71–1.78; z = 0.50). The Cochrane’s Q test (Chi2 = 31.73; P = 0.000) and I2 test (I2 = 93.7%) revealed significant heterogeneity. The funnel plot identified two studies over the pseudo-95% CI (Fig. 3e).
Association of De Ritis ratio with CSS in UCB
Three studies including 1042 patients provided data on the association of De Ritis ratio with CSS in UCB. The forest plot (Fig. 2f) revealed that De Ritis ratio was significantly associated with CSS in UCB (pooled HR, 2.18; 95% CI, 1.37 − 3.48; z = 3.30). The Cochrane’s Q test (Chi2 = 5.35; P = 0.069) and I2 test (I2 = 62.6%) revealed significant heterogeneity. The funnel plot identified one study over the pseudo-95% CI (Fig. 3f).
Association of Albumin-globulin ratio with CSS in UCB
Two studies including 485 patients provided data on the association of albumin-globulin ratio (AGR) with CSS in UCB. The forest plot (Fig. 2g) revealed that AGR was significantly associated with CSS in UCB (pooled HR: 0.26, 95% CI 0.14–0.48; z = 4.27). The Cochrane’s Q test (Chi2 = 0.04; P = 0.837) and I2 test (I2 = 0.0%) revealed no significant heterogeneity. The funnel plot did not identify any studies over the pseudo-95% CI (Fig. 3g).
Association of CRP with CSS in UCB
Two studies including 913 patients provided data on the association of CRP with CSS in UCB. The forest plot (Fig. 2h) revealed that CRP was significantly associated with CSS in UCB (pooled HR: 1.44, 95% CI 1.26–1.66; z = 5.15). The Cochrane’s Q test (Chi2 = 0.05; P = 0.816) and I2 test (I2 = 0.0%) revealed no significant heterogeneity. The funnel plot did not identify any studies over the pseudo-95% CI (Fig. 3h).
Association of Platelet-lymphocyte ratio with CSS in UCB
Two studies including 261 patients provided data on the association of platelet-lymphocyte ratio (PLR) with CSS in UCB. The forest plot (Fig. 2I) revealed that PLR was not significantly associated with CSS in UCB (pooled HR: 1.00, 95% CI 1.00–1.00; z = 0.10). The Cochrane’s Q test (Chi2 = 0.22; P = 0.635) and I2 test (I2 = 0.0%) revealed no significant heterogeneity. The funnel plot did not identify any studies over the pseudo-95% CI (Fig.3I).
Association of White blood cell with CSS in UBC
Two studies including 668 patients provided data on the association of white blood cell (WBC) with CSS in UCB. The forest plot (Fig. 2j) revealed that WBC was significantly associated with CSS in UCB (pooled HR: 1.05, 95% CI 1.02–1.07; z = 3.95). The Cochrane’s Q test (Chi2 = 1.41; P = 0.235) and I2 test (I2 = 29.0%) revealed significant heterogeneity. The funnel plot did not identify any studies over the pseudo-95% CI (Fig. 3j).
Association of leukocyte with CSS in UCB
Two studies including 1, 192 patients provided data on the association of leukocyte with CSS in UCB. The forest plot (Fig. 2k) revealed that leukocyte was not significantly associated with CSS in UCB (pooled HR: 1.24, 95% CI 0.51 − 3.04; z = 0.02). The Cochrane’s Q test (Chi2 = 3.02; P = 0.097) and I2 test (I2 = 63.6%) revealed significant heterogeneity. The funnel plot did not identify any studies over the pseudo-95% CI (Fig. 3k).
Other factors associated with CSS (in one paper only)
Estimate glomerular filtration rate (eGFR), and lymphocyte were significantly associated with CSS in one study each. Lactate dehydrogenase (LDH), and neutrocyte were found not to be significantly associated with CSS in one study each.
Discussion
This systematic review and meta-analysis were conducted to investigate the prognostic value of preoperative hematologic biomarkers in UCB, based on their association with CSS. Study results indicate that high preoperative NLR, CRP, WBC, and De Ritis ratio, as well as low AGR, and Hb are significantly associated with worse CSS.
First, De Ritis ratio was found to be associated with CSS in UCB, potentially as a marker of cellular metabolism and cancer cell turnover. It is generally assumed that alanine aminotransferase (ALT) is more liver-specific, whereas aspartate aminotransferase (AST) is widely expressed in different tissue types [54]. Therefore, pathological conditions associated with tumor proliferation, tumor cell turnover, and tissue damage, are thought to be more likely to increase AST than ALT, thus making the AST/ALT ratio an attractive potential biomarker [55]. However, the exact mechanism underlying the correlation between elevated AST/ALT and poor prognosis in UCB patients remains to be elucidated. Most cancer cells rely on anaerobic glycolysis to generate the energy required for survival, growth and metastasis even in the presence of oxygen via a process referred to as the “Warburg effect” [56]. Furthermore, increased glycolysis has been shown to be linked to several alterations in mitochondrial activity involving NADH-related enzymes and glucose transporters, and high LDH and cytosolic NADH/NAD + have been shown to be essential for the maintenance of this enhanced glycolysis [57, 58]. AST is known to form part of the malate-aspartate shuttle pathway facilitating NADH/NAD + conversion [59]. Therefore, AST/ALT may be related to tumor metabolism in many glucose-utilizing malignancies, such as UC [60,61,62].
Second, AGR was found to be associated with CSS in UCB. Of the 2 major human serum proteins evaluated in AGR, albumin and globulin, albumin is generally used to assess nutritional status and severity of disease. Low albumin has been shown to reflect malnutrition, which is common among patients with cancer, leading to disruption of a number of human defense mechanisms, such as anatomic barriers, cellular and humoral immunity, and phagocyte function [63, 64]. Moreover, albumin is now considered a marker of inflammatory response in addition to a nutritional marker [65, 66]. Globulin (derived from total protein minus the albumin fraction) consists of various pro-inflammatory proteins, including CRP, complement components, and immunoglobulins, and is, therefore, a central component of immunity and inflammation. Chronic inflammation markers play an important role in the proliferation, progression, development, and metastasis of tumor cells. Thus, AGR, as a combination of 2 separate predictors of adverse outcome, may have greater predictive value, given that nutritional status and systemic inflammatory response are both implicated in the outcome of patients with UCB undergoing RC.
Third, as an index of hypoxia, Hb was found to be associated with CSS in UCB. Hypoxia, which is commonly seen in advanced tumors, represents an imbalance between oxygen supply and consumption and thus may contribute to the resistance of tumor cells to therapy, whose impact may also be further enhanced by anemia [67, 68]. Tumor hypoxia has been shown to induce expression of hypoxia-inducible factor 1α (HIF1α), which is known to be integral to adaptively responding to hypoxia by targeting many genes involved in facilitating tumor survival, proliferation, invasion, and metastasis [69,70,71]. Furthermore, research suggests that hypoxia may promote tumor progression by inducing genetic changes and clonal selection in tumor cells [72].
Finally, in addition to AGR, several markers of the systemic inflammatory response, such as CRP, WBC, and NLR were shown to be significantly associated with CSS in UCB. These markers are known to be stimulated by cancer-related inflammatory factors, such as interleukin-6 thus sensitively reflecting cancer-related inflammation [7, 73, 74]. Cancer and inflammation are linked through both extrinsic and intrinsic pathways, with the former being activated by infection or chronic inflammation, and the latter being driven by genetic changes, such as oncogene activation or tumor suppressor gene deactivation. Both pathways activate key transcription factors, primarily nuclear factor -kB, signal transducer and activator of transcription 3, and HIF1α in tumor cells, which in turn lead to inflammatory mediators and cyclooxygenase-2 being produced, resulting in cancer-related inflammation and further promotion of tumor progression [7]. Therefore, the elevation of these systemic inflammatory response biomarkers impacts cancer growth and development [75]. Moreover, not only above mentioned systemic inflammatory markers, anemia is also brought about by inflammation such as IL-6 [76]. Hypoxia due to anemia will lead to increased HIF1α, which then activate Glucose transporter 1 and Phosphofructokinase-2 involved in glycolysis, leading to an increase of De Ritis ratio [69, 77,78,79]. Thus, the hematological biomarkers we identified are all related to inflammation.
Although this meta-analysis revealed a strong association between several biomarkers and UCB mortality, it has some limitations that need to be taken into account. First, reporting bias could have led to non-publication of negative results. All the studies included were retrospective in design, thus increasing the risk of selection bias. Second, unknown pre-treatment factors (e.g., nutritional deficiencies, comorbidities, medications, and lifestyle factors) may have affected the hematologic biomarkers, thus producing systematic bias. Third, there were no established cut-off values for hematologic biomarkers among the studies evaluated, with the cut-off value being chosen by most investigators based on statistical methods (e.g., based on the highest sensitivity and specificity), the lower or higher limit of normal, or with pre-defined biomarker cut-off values from the literature. Fourth, the preoperative chemotherapeutic protocols were heterogeneous between the studies included, which did not allow each individual protocol to be assessed for its impact on the prognostic factors evaluated. In particular, it was a major limitation of the study that the hematologic biomarkers were not readily evaluable for their prognostic value in patients receiving and those not receiving NAC. Fifth, this systematic review and meta-analysis included no patients receiving immunotherapy. In this era of immunotherapy and other newly available targeted therapies, it remains unclear how the results of this meta-analysis may direct impact on patient management. Sixth, while it is crucial to examine hematologic biomarkers for their combined prognostic significance in UCB, this has not been adequately addressed in this systematic review and meta-analysis. It is a further limitation of the study that it was confined to the analysis of preoperative biomarkers, to the exclusion of relevant perioperative biomarkers. Seventh, despite its relevance, intravesical therapy prior to RC was not readily evaluable for its prognostic significance in UCB due to the paucity of data available from the literature. Finally, heterogeneity was detected in the CSS analysis, thus limiting the value of these results. Although the random effect model was used to address heterogeneity among the studies evaluated, the conclusions should be interpreted with caution. Therefore, well-designed prospective studies with long-term follow-up are required to validate the prognostic value of biomarkers in this setting, and to determine whether they could improve the current tools for risk stratification of patients with UCB.
Conclusions
This meta-analysis revealed that several preoperative hematologic biomarkers were associated with an increased risk of cancer-specific mortality in patients with UCB. Therefore, it might be useful to incorporate such hematologic biomarkers into prognostic tools to help with appropriate risk stratification of patients with UCB. In addition, low AGR had the highest HR, suggesting indirectly potentially stronger prognostic value than any other biomarkers.
References
Antoni S, Ferlay J, Soerjomataram I et al (2017) Bladder cancer incidence and mortality: a global overview and recent trends. Eur Urol 71(1):96–108. https://doi.org/10.1016/j.eururo.2016.06.010
Babjuk M, Burger M, Comperat EM et al (2019) European Association of Urology Guidelines on Non-muscle-invasive Bladder Cancer (TaT1 and Carcinoma In Situ)—2019 Update. Eur Urol 76(5):639–657. https://doi.org/10.1016/j.eururo.2019.08.016
Alfred Witjes J, Lebret T, Comperat EM et al (2017) Updated 2016 EAU guidelines on muscle-invasive and metastatic bladder cancer. Eur Urol 71(3):462–475. https://doi.org/10.1016/j.eururo.2016.06.020
Abdollah F, Gandaglia G, Thuret R et al (2013) Incidence, survival and mortality rates of stage-specific bladder cancer in United States: a trend analysis. Cancer Epidemiol 37(3):219–225. https://doi.org/10.1016/j.canep.2013.02.002
Zargar H, Espiritu PN, Fairey AS et al (2015) Multicenter assessment of neoadjuvant chemotherapy for muscle-invasive bladder cancer. Eur Urol 67(2):241–249. https://doi.org/10.1016/j.eururo.2014.09.007
Kluth LA, Black PC, Bochner BH et al (2015) Prognostic and prediction tools in bladder cancer: a comprehensive review of the literature. Eur Urol 68(2):238–253. https://doi.org/10.1016/j.eururo.2015.01.032
Putluri N, Shojaie A, Vasu VT et al (2011) Metabolomic profiling reveals potential markers and bioprocesses altered in bladder cancer progression. Can Res 71(24):7376–7386. https://doi.org/10.1158/0008-5472.can-11-1154
Karakiewicz PI, Shariat SF, Palapattu GS et al (2006) Nomogram for predicting disease recurrence after radical cystectomy for transitional cell carcinoma of the bladder. J Urol 176(4 Pt 1):1354–1361. https://doi.org/10.1016/j.juro.2006.06.025(discussion 1361-1352)
Shariat SF, Palapattu GS, Karakiewicz PI et al (2007) Discrepancy between clinical and pathologic stage: impact on prognosis after radical cystectomy. Eur Urol 51(1):137–149. https://doi.org/10.1016/j.eururo.2006.05.021(discussion 149-151)
Lucca I, Jichlinski P, Shariat SF et al (2016) The neutrophil-to-lymphocyte ratio as a prognostic factor for patients with urothelial carcinoma of the bladder following radical cystectomy: validation and meta-analysis. Eur Urol Focus 2(1):79–85. https://doi.org/10.1016/j.euf.2015.03.001
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100. https://doi.org/10.1371/journal.pmed.1000100
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605. https://doi.org/10.1007/s10654-010-9491-z
Deeks JJ, Dinnes J, D'Amico R et al (2003) Evaluating non-randomised intervention studies. Health Technol Assess (Winchester, England) 7(27):1–173. https://doi.org/10.3310/hta7270(iii-x)
Altman DG, Bland JM (2011) How to obtain the confidence interval from a P value. BMJ (Clin Res Ed) 343:d2090. https://doi.org/10.1136/bmj.d2090
Altman DG, Bland JM (2011) How to obtain the P value from a confidence interval. BMJ (Clin Res Ed) 343:d2304. https://doi.org/10.1136/bmj.d2304
DerSimonian R, Kacker R (2007) Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials 28(2):105–114. https://doi.org/10.1016/j.cct.2006.04.004
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188. https://doi.org/10.1016/0197-2456(86)90046-2
Higgins JP, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analyses. BMJ (Clin Res Ed) 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Buisan O, Orsola A, Areal J et al (2017) Low pretreatment neutrophil-to-lymphocyte ratio predicts for good outcomes in patients receiving neoadjuvant chemotherapy before radical cystectomy for muscle invasive bladder cancer. Clin Genitour Cancer 15(1):145–151.e142. https://doi.org/10.1016/j.clgc.2016.05.004
Calvete J, Larrinaga G, Errarte P et al (2019) The coexpression of fibroblast activation protein (FAP) and basal-type markers (CK 5/6 and CD44) predicts prognosis in high-grade invasive urothelial carcinoma of the bladder. Hum Pathol 91:61–68. https://doi.org/10.1016/j.humpath.2019.07.002
Chipollini JJ, Tang DH, Patel SY et al (2017) Perioperative transfusion of leukocyte-depleted blood products in contemporary radical cystectomy cohort does not adversely impact short-term survival. Urology 103:142–148. https://doi.org/10.1016/j.urology.2016.12.015
D'Andrea D, Moschini M, Gust KM et al (2017) Lymphocyte-to-monocyte ratio and neutrophil-to-lymphocyte ratio as biomarkers for predicting lymph node metastasis and survival in patients treated with radical cystectomy. J Surg Oncol 115(4):455–461. https://doi.org/10.1002/jso.24521
Ergani B, Türk H, Ün S et al (2015) Prognostic effect of preoperative anemia in patients who have undergone radical cystectomy for bladder cancer. Cancer Treat Commun 4:196–199. https://doi.org/10.1016/j.ctrc.2015.11.005
Gershman B, Moreira DM, Tollefson MK et al (2016) The association of ABO blood type with disease recurrence and mortality among patients with urothelial carcinoma of the bladder undergoing radical cystectomy. Urol Oncol 34(1):4.e1–9. https://doi.org/10.1016/j.urolonc.2015.07.023
Gierth M, Mayr R, Aziz A et al (2015) Preoperative anemia is associated with adverse outcome in patients with urothelial carcinoma of the bladder following radical cystectomy. J Cancer Res Clin Oncol 141(10):1819–1826. https://doi.org/10.1007/s00432-015-1957-7
Gondo T, Nakashima J, Ohno Y et al (2012) Prognostic value of neutrophil-to-lymphocyte ratio and establishment of novel preoperative risk stratification model in bladder cancer patients treated with radical cystectomy. Urology 79(5):1085–1091. https://doi.org/10.1016/j.urology.2011.11.070
Gorgel SN, Kose O, Koc EM et al (2017) The prognostic significance of preoperatively assessed AST/ALT (De Ritis) ratio on survival in patients underwent radical cystectomy. Int Urol Nephrol 49(9):1577–1583. https://doi.org/10.1007/s11255-017-1648-1
Grimm T, Buchner A, Schneevoigt B et al (2016) Impact of preoperative hemoglobin and CRP levels on cancer-specific survival in patients undergoing radical cystectomy for transitional cell carcinoma of the bladder: results of a single-center study. World J Urol 34(5):703–708. https://doi.org/10.1007/s00345-015-1680-7
Ha YS, Kim SW, Chun SY et al (2019) Association between De Ritis ratio (aspartate aminotransferase/alanine aminotransferase) and oncological outcomes in bladder cancer patients after radical cystectomy. BMC urology 19(1):10. https://doi.org/10.1186/s12894-019-0439-7
Hermanns T, Bhindi B, Wei Y et al (2014) Pre-treatment neutrophil-to-lymphocyte ratio as predictor of adverse outcomes in patients undergoing radical cystectomy for urothelial carcinoma of the bladder. Br J Cancer 111(3):444–451. https://doi.org/10.1038/bjc.2014.305
Jo JK, Jeong SJ, Hong SK, Byun SS, Lee SE, Oh JJ (2016) The impact of preoperative anemia on oncologic outcome in patients undergoing radical cystectomy for urothelial carcinoma of the bladder. Int Urol Nephrol 48(4):489–494. https://doi.org/10.1007/s11255-016-1219-x
Jokisch JF, Grimm T, Buchner A et al (2019) Preoperative thrombocytosis in patients undergoing radical cystectomy for urothelial cancer of the bladder: an independent prognostic parameter for an impaired oncological outcome. Urol Int. https://doi.org/10.1159/000500729
Kang M, Balpukov UJ, Jeong CW et al (2017) Can the preoperative neutrophil-to-lymphocyte ratio significantly predict the conditional survival probability in muscle-invasive bladder cancer patients undergoing radical cystectomy? Clin Genitour Cancer 15(3):e411–e420. https://doi.org/10.1016/j.clgc.2016.10.015
Kluth LA, Xylinas E, Rieken M et al (2015) Prognostic model for predicting survival in patients with disease recurrence following radical cystectomy. Eur Urol Focus 1(1):75–81. https://doi.org/10.1016/j.euf.2014.10.003
Ku JH, Kang M, Kim HS et al (2015) The prognostic value of pretreatment of systemic inflammatory responses in patients with urothelial carcinoma undergoing radical cystectomy. Br J Cancer 112(3):461–467. https://doi.org/10.1038/bjc.2014.631
Kwon T, Jeong IG, You D et al (2014) Obesity and prognosis in muscle-invasive bladder cancer: the continuing controversy. Int J Urol 21(11):1106–1112. https://doi.org/10.1111/iju.12530
Lambert JW, Ingham M, Gibbs BB et al (2013) Using preoperative albumin levels as a surrogate marker for outcomes after radical cystectomy for bladder cancer. Urology 81(3):587–592. https://doi.org/10.1016/j.urology.2012.10.055
Liu J, Dai Y, Zhou F et al (2016) The prognostic role of preoperative serum albumin/globulin ratio in patients with bladder urothelial carcinoma undergoing radical cystectomy. Urol Oncol 34(11):484.e481–484.e488. https://doi.org/10.1016/j.urolonc.2016.05.024
Liu Z, Huang H, Li S et al (2017) The prognostic value of preoperative serum albumin-globulin ratio for high-grade bladder urothelial carcinoma treated with radical cystectomy: A propensity score-matched analysis. J Cancer Res Ther 13(5):837–843. https://doi.org/10.4103/jcrt.JCRT_237_17
Matsumoto A, Nakagawa T, Kanatani A et al (2018) Preoperative chronic kidney disease is predictive of oncological outcome of radical cystectomy for bladder cancer. World J Urol 36(2):249–256. https://doi.org/10.1007/s00345-017-2141-2
Miyake M, Morizawa Y, Hori S et al (2017) Integrative assessment of pretreatment inflammation-, nutrition-, and muscle-based prognostic markers in patients with muscle-invasive bladder cancer undergoing radical cystectomy. Oncology 93(4):259–269. https://doi.org/10.1159/000477405
Moschini M, Suardi N, Pellucchi F et al (2014) Impact of preoperative thrombocytosis on pathological outcomes and survival in patients treated with radical cystectomy for bladder carcinoma. Anticancer Res 34(6):3225–3230
Ozcan C, Telli O, Ozturk E et al (2015) The prognostic significance of preoperative leukocytosis and neutrophil-to-lymphocyte ratio in patients who underwent radical cystectomy for bladder cancer. Canad Urological Assoc Journal de l'Association des urologues du Canada 9(11–12):E789–794. https://doi.org/10.5489/cuaj.3061
Rajwa P, Zyczkowski M, Paradysz A et al (2018) Evaluation of the prognostic value of LMR, PLR, NLR, and dNLR in urothelial bladder cancer patients treated with radical cystectomy. Eur Rev Med Pharmacol Sci 22(10):3027–3037. https://doi.org/10.26355/eurrev_201805_15060
Schubert T, Todenhofer T, Mischinger J et al (2016) The prognostic role of pre-cystectomy hemoglobin levels in patients with invasive bladder cancer. World J Urol 34(6):829–834. https://doi.org/10.1007/s00345-015-1693-2
Sejima T, Morizane S, Yao A et al (2014) Prognostic impact of preoperative hematological disorders and a risk stratification model in bladder cancer patients treated with radical cystectomy. Int J Urol 21(1):52–57. https://doi.org/10.1111/iju.12161
Tan YG, Eu E, Lau KamOn W et al (2017) Pretreatment neutrophil-to-lymphocyte ratio predicts worse survival outcomes and advanced tumor staging in patients undergoing radical cystectomy for bladder cancer. Asian J Urol 4(4):239–246. https://doi.org/10.1016/j.ajur.2017.01.004
Todenhofer T, Renninger M, Schwentner C et al (2012) A new prognostic model for cancer-specific survival after radical cystectomy including pretreatment thrombocytosis and standard pathological risk factors. BJU Internat 110(11 Pt B):E533–E540. https://doi.org/10.1111/j.1464-410X.2012.11231.x
Un S, Turk H, Dindar AS et al (2018) Does preoperative neutrophil/lymphocyte rate have an effect on survival of the bladder cancer patients who received radical cystectomy? J Cancer Res Ther 14(2):432–436. https://doi.org/10.4103/0973-1482.183555
Viers BR, Boorjian SA, Frank I et al (2014) Pretreatment neutrophil-to-lymphocyte ratio is associated with advanced pathologic tumor stage and increased cancer-specific mortality among patients with urothelial carcinoma of the bladder undergoing radical cystectomy. Eur Urol 66(6):1157–1164. https://doi.org/10.1016/j.eururo.2014.02.042
Yang MH, Yen CC, Chen PM et al (2002) Prognostic-factors-based risk-stratification model for invasive urothelial carcinoma of the urinary bladder in Taiwan. Urology 59(2):232–238. https://doi.org/10.1016/s0090-4295(0101590-4(discussion 238-239)
Yoshida T, Kinoshita H, Yoshida K et al (2016) Prognostic impact of perioperative lymphocyte-monocyte ratio in patients with bladder cancer undergoing radical cystectomy. Tumour Biolo 37(8):10067–10074. https://doi.org/10.1007/s13277-016-4874-8
Yuk HD, Jeong CW, Kwak C et al (2019) De Ritis Ratio (Aspartate Transaminase/Alanine Transaminase) as a Significant Prognostic Factor in Patients Undergoing Radical Cystectomy with Bladder Urothelial Carcinoma: a Propensity Score-Matched Study. Dis Markers 2019:6702964. https://doi.org/10.1155/2019/6702964
Botros M, Sikaris KA (2013) The de ritis ratio: the test of time. Clin Biochem Rev 34(3):117–130
Conde VR, Oliveira PF, Nunes AR et al (2015) The progression from a lower to a higher invasive stage of bladder cancer is associated with severe alterations in glucose and pyruvate metabolism. Exp Cell Res 335(1):91–98. https://doi.org/10.1016/j.yexcr.2015.04.007
Warburg O (1956) On the origin of cancer cells. Science (New York, NY) 123(3191):309–314. https://doi.org/10.1126/science.123.3191.309
Dorward A, Sweet S, Moorehead R et al (1997) Mitochondrial contributions to cancer cell physiology: redox balance, cell cycle, and drug resistance. J Bioenerg Biomembr 29(4):385–392. https://doi.org/10.1023/a:1022454932269
Fantin VR, St-Pierre J, Leder P (2006) Attenuation of LDH-A expression uncovers a link between glycolysis, mitochondrial physiology, and tumor maintenance. Cancer Cell 9(6):425–434. https://doi.org/10.1016/j.ccr.2006.04.023
Greenhouse WV, Lehninger AL (1976) Occurrence of the malate-aspartate shuttle in various tumor types. Can Res 36(4):1392–1396
Tai YS, Chen CH, Huang CY et al (2015) Diabetes mellitus with poor glycemic control increases bladder cancer recurrence risk in patients with upper urinary tract urothelial carcinoma. Diabetes/Metab Res Rev 31(3):307–314. https://doi.org/10.1002/dmrr.2614
Whyard T, Waltzer WC, Waltzer D et al (2016) Metabolic alterations in bladder cancer: applications for cancer imaging. Exp Cell Res 341(1):77–83. https://doi.org/10.1016/j.yexcr.2016.01.005
Kitajima K, Yamamoto S, Fukushima K et al (2016) FDG-PET/CT as a post-treatment restaging tool in urothelial carcinoma: Comparison with contrast-enhanced CT. Eur J Radiol 85(3):593–598. https://doi.org/10.1016/j.ejrad.2015.12.017
Dewys WD, Begg C, Lavin PT et al (1980) Prognostic effect of weight loss prior to chemotherapy in cancer patients Eastern Cooperative Oncology Group. Am J Med 69(4):491–497. https://doi.org/10.1016/s0149-2918(05)80001-3
Chandra RK (1999) Nutrition and immunology: from the clinic to cellular biology and back again. Proc Nutr Soc 58(3):681–683. https://doi.org/10.1017/s0029665199000890
Barbosa-Silva MC (2008) Subjective and objective nutritional assessment methods: what do they really assess? Curr Opin Clin Nutr Metab Care 11(3):248–254. https://doi.org/10.1097/MCO.0b013e3282fba5d7
McMillan DC, Watson WS, O'Gorman P et al (2001) Albumin concentrations are primarily determined by the body cell mass and the systemic inflammatory response in cancer patients with weight loss. Nutr Cancer 39(2):210–213. https://doi.org/10.1207/S15327914nc392_8
Vaupel P, Thews O, Hoeckel M (2001) Treatment resistance of solid tumors: role of hypoxia and anemia. Med Oncol (Northwood, London, England) 18(4):243–259. https://doi.org/10.1385/mo:18:4:243
Vaupel P (2004) The role of hypoxia-induced factors in tumor progression. Oncologist 9(Suppl 5):10–17. https://doi.org/10.1634/theoncologist.9-90005-10
Dachs GU, Tozer GM (2000) Hypoxia modulated gene expression: angiogenesis, metastasis and therapeutic exploitation. Eur J Cancer (Oxford, England: 1990) 36(13 Spec No):1649–1660. https://doi.org/10.1016/s0959-8049(00)00159-3
Semenza GL (2000) Hypoxia, clonal selection, and the role of HIF-1 in tumor progression. Crit Rev Biochem Mol Biol 35(2):71–103. https://doi.org/10.1080/10409230091169186
Wu S, Jiang F, Wu H et al (2018) Prognostic significance of hypoxia inducible factor-1alpha expression in patients with clear cell renal cell carcinoma. Mol Med Rep 17(3):4846–4852. https://doi.org/10.3892/mmr.2018.8409
Coquelle A, Toledo F, Stern S et al (1998) A new role for hypoxia in tumor progression: induction of fragile site triggering genomic rearrangements and formation of complex DMs and HSRs. Mol Cell 2(2):259–265. https://doi.org/10.1016/s1097-2765(00)80137-9
Andrews B, Shariat SF, Kim JH et al (2002) Preoperative plasma levels of interleukin-6 and its soluble receptor predict disease recurrence and survival of patients with bladder cancer. J Urol 167(3):1475–1481
Shariat SF, Semjonow A, Lilja H et al (2011) Tumor markers in prostate cancer I: blood-based markers. Acta Oncol (Stockholm, Sweden) 50(Suppl 1):61–75. https://doi.org/10.3109/0284186x.2010.542174
Lucca I, Hofbauer SL, Leitner CV et al (2016) Development of a preoperative nomogram incorporating biomarkers of systemic inflammatory response to predict nonorgan-confined urothelial carcinoma of the bladder at radical cystectomy. Urology 95:132–138. https://doi.org/10.1016/j.urology.2016.06.007
Raj DS (2009) Role of interleukin-6 in the anemia of chronic disease. Semin Arthritis Rheum 38(5):382–388. https://doi.org/10.1016/j.semarthrit.2008.01.006
Bartrons R, Caro J (2007) Hypoxia, glucose metabolism and the Warburg's effect. J Bioenerg Biomembr 39(3):223–229. https://doi.org/10.1007/s10863-007-9080-3
Ancey PB, Contat C, Meylan E (2018) Glucose transporters in cancer—from tumor cells to the tumor microenvironment. FEBS J 285(16):2926–2943. https://doi.org/10.1111/febs.14577
Chesney J (2006) 6-phosphofructo-2-kinase/fructose-2, 6-bisphosphatase and tumor cell glycolysis. Curr Opin Clin Nutr Metab Care 9(5):535–539. https://doi.org/10.1097/01.mco.0000241661.15514.fb
Acknowledgements
Open access funding provided by Medical University of Vienna.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Project development: KM, SE, PIK, SFS. Data collection: KM, NM, HM, FQ, Data analysis: KM, RSM, IL, SK. Manuscript writing/editing: KM, NM, HM, FQ, RSM, IL, SK, SE, PIK, SFS.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Mori, K., Miura, N., Mostafaei, H. et al. Prognostic value of preoperative hematologic biomarkers in urothelial carcinoma of the bladder treated with radical cystectomy: a systematic review and meta-analysis. Int J Clin Oncol 25, 1459–1474 (2020). https://doi.org/10.1007/s10147-020-01690-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-020-01690-1