Abstract
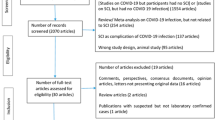
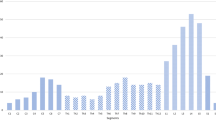
The neurological manifestations of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, including spontaneous spinal hemorrhage (SSH), are diverse. SSH is a detrimental neurosurgical event requiring immediate medical attention. We aimed to investigate the association between SARS-CoV-2 and SSH and delineate a rational clinical approach. The authors searched PubMed, Scopus, Web of Science, and Google Scholar for studies published up to January 25, 2023, on SSH and SARS-CoV-2 infection. For each dataset, the authors performed pooled estimates examining three outcomes of interest: (1) early post-intervention neurological status, (2) mortality, and (3) post-intervention neurological rehabilitation outcomes. After reviewing 1341 results, seven datasets were identified for the final analysis. Fifty-seven percent of patients were females. Twenty-eight percent of the patients experienced severe systemic infection. The mean interval between the SARS-CoV-2 infection and neurological presentation was 18 days. Pain and sensorimotor deficits were the most common (57%). Spinal epidural hematoma (EDH) was the most common presentation (71.4%). Three patients were treated conservatively, while 4 received neurosurgical intervention. Pain and sensorimotor deficits had the best treatment response (100%), while the sphincter had the worst response (0%). Long-term follow-up showed that 71% of patients had good recovery. SARS-CoV-2-associated SSH is a rare complication of infection, with an often insidious presentation that requires high clinical suspicion. Patients with SARS-CoV-2 infection and new neurological symptoms or disproportionate neck or back pain require a neuroaxis evaluation. Neurosurgical intervention and conservative management are both viable options to treat SSH following COVID-19. Still, a homogenous approach to the treatment paradigm of SSH cannot be obtained, but lesions with space-occupying effects are suitable for neurosurgical evacuation-decompression while more indolent lesions could be treated conservatively. These options should be tailored individually until larger studies provide a consensus.

Similar content being viewed by others
References
Gupta A, Madhavan MV, Sehgal K, Nair N, Mahajan S, Sehrawat TS et al (2020) Extrapulmonary manifestations of COVID-19. Nat Med 26(7):1017–1032. https://doi.org/10.1038/s41591-020-0968-3
Abobaker A, Raba AA, Alzwi A (2020) Extrapulmonary and atypical clinical presentations of COVID-19. J Med Virol 92(11):2458–2464. https://doi.org/10.1002/jmv.26157
Deeb A, Kumar PC, Sakrani N, Trehan RK, Papinenei VR (2021) Neurological presentations of COVID-19: characteristic features in a case series of hospitalized patients from Abu Dhabi UAE. Biomed Res Int 2021:5822259. https://doi.org/10.1155/2021/5822259
Figueroa J, DeVine JG (2017) Spontaneous spinal epidural hematoma: literature review. J Spine Surg 3(1):58–63. https://doi.org/10.21037/jss.2017.02.04
Raasck K, Habis AA, Aoude A, Simões L, Barros F, Reindl R et al (2017) Spontaneous spinal epidural hematoma management: a case series and literature review. Spinal Cord Ser Cases 3:16043. https://doi.org/10.1038/scsandc.2016.43
Zübeyde Ö, Adem K, Samet D (2022) A case of spontaneous thoracolumbar epidural hematoma in Covid-19 pneumonia. Int J Surg Case Rep 90:106719. https://doi.org/10.1016/j.ijscr.2021.106719
Lim SW, Wong E (2020) Spontaneous epidural hematoma of the cervical spine in an elderly woman with recent COVID-19 infection: a case report. Am J Case Rep 21:e926784. https://doi.org/10.12659/ajcr.926784
Sabouri M, Rezvani M, Aminmansour B, Sourani A, Baradaran MS (2022) Spontaneous intramedullary hematoma in a patient with COVID-19 infection: a case report. Clin Case Rep 10(2):e05387. https://doi.org/10.1002/ccr3.5387
Romagna A, Potthast F, Steinborn MM, Burdach S, Lehmberg J (2022) Surgical treatment of a spontaneous spinal epidural hematoma under antithrombotic treatment of a multisystem inflammatory syndrome in children associated with SARS-COV-2. Childs Nerv Syst 38(6):1213–1216. https://doi.org/10.1007/s00381-021-05375-6
Scalia G, Umana GE, Marrone S, Graziano F, Giuffrida A, Ponzo G et al (2021) Spontaneous anterior cervicothoracic spinal epidural hematoma extending to clivus in SARS-CoV-2 infection. Surg Neurol Int 12:181. https://doi.org/10.25259/sni_40_2021
Dlaka D, Vavro H, Romić D, Almahariq F, Chudy D, Lukšić I et al (2022) Spontaneous spinal subdural hematoma in COVID-19 patient: Croatian national COVID hospital experience. Surg Neurol Int 13:394. https://doi.org/10.25259/sni_87_2022
Chu EC, Trager RJ, Lai CR, Shum JS (2022) Spontaneous cervical epidural hematoma following COVID-19 illness presenting to a chiropractor: a case report. Cureus 14(12):e32199. https://doi.org/10.7759/cureus.32199
Garg RK, Paliwal VK, Gupta A (2021) Spinal cord involvement in COVID-19: a review. J Spinal Cord Med:1–15. https://doi.org/10.1080/10790268.2021.1888022
Mondal R, Deb S, Shome G, Ganguly U, Lahiri D, Benito-León J (2021) COVID-19 and emerging spinal cord complications: a systematic review. Mult Scler Relat Disord 51:102917. https://doi.org/10.1016/j.msard.2021.102917
Jafari Khaljiri H, Jamalkhah M, Amini Harandi A, Pakdaman H, Moradi M, Mowla A (2021) Comprehensive review on neuro-COVID-19 pathophysiology and clinical consequences. Neurotox Res 39(5):1613–1629. https://doi.org/10.1007/s12640-021-00389-z
Margos NP, Meintanopoulos AS, Filioglou D, Ellul J (2021) Intracerebral hemorrhage in COVID-19: a narrative review. J Clin Neurosci 89:271–278. https://doi.org/10.1016/j.jocn.2021.05.019
Fraiman P, Freire M, Moreira-Neto M, Godeiro-Junior C (2020) Hemorrhagic stroke and COVID-19 infection: coincidence or causality? eNeurologicalSci 21:100274. https://doi.org/10.1016/j.ensci.2020.100274
Chian Chiang Nicholas C, John M, Jerome I, Yuen S (2020) Acute transverse myelitis in COVID-19 infection. BMJ Case Rep 13(8):e236720. https://doi.org/10.1136/bcr-2020-236720
Gulati N, Kapila S, Bhalla Sehgal L, Sehgal V, Lnu P (2022) Myelitis following COVID-19 illness. Cureus 14(8):e28134. https://doi.org/10.7759/cureus.28134
Beyrouti R, Best JG, Chandratheva A, Perry RJ, Werring DJ (2021) Characteristics of intracerebral haemorrhage associated with COVID-19: a systematic review and pooled analysis of individual patient and aggregate data. J Neurol 268(9):3105–3115. https://doi.org/10.1007/s00415-021-10425-9
Leasure AC, Khan YM, Iyer R, Elkind MSV, Sansing LH, Falcone GJ et al (2021) Intracerebral hemorrhage in patients with COVID-19: an analysis from the COVID-19 Cardiovascular Disease Registry. Stroke 52(7):e321–e3e3. https://doi.org/10.1161/strokeaha.121.034215
Kaushik RM, Kumar R, Kaushik M, Saini M, Kaushik R (2022) Spontaneous spinal intradural hemorrhage in dengue fever: a case report. J Med Case Rep 16(1):213. https://doi.org/10.1186/s13256-022-03451-2
Patel H, Boaz JC, Phillips JP, Garg BP (1998) Spontaneous spinal epidural hematoma in children. Pediatr Neurol 19(4):302–307. https://doi.org/10.1016/s0887-8994(98)00059-9
Leep Hunderfund AN, Wijdicks EF (2009) Intramedullary spinal cord hemorrhage (hematomyelia). Rev Neurol Dis 6(2):E54–E61
Peng D, Yan M, Liu T, Yang K, Ma Y, Hu X et al (2022) Prognostic factors and treatments efficacy in spontaneous spinal epidural hematoma: a multicenter retrospective study. Neurology 99(8):e843–ee50. https://doi.org/10.1212/wnl.0000000000200844
Bakker NA, Veeger NJ, Vergeer RA, Groen RJ (2015) Prognosis after spinal cord and cauda compression in spontaneous spinal epidural hematomas. Neurology 84(18):1894–1903. https://doi.org/10.1212/wnl.0000000000001545
Sheng OC, Wu R-C, Chang IH (2021) Spontaneous spinal epidural hematoma: a case report. Int J Emerg Med 14(1):60. https://doi.org/10.1186/s12245-021-00379-0
Sourani A, Rezvani M, Foroughi M, Baradaran MS (2022) Spontaneous intramedullary hematoma following COVID-19 vaccination: a case report. Clin Case Rep 10(12):e6743. https://doi.org/10.1002/ccr3.6743
Maghrabi Y, Baeesa SS (2021) Acute hemorrhagic myelitis in an adolescent with COVID-19: a case report and review of literature. Cureus 13(12):e20553. https://doi.org/10.7759/cureus.20553
Schulte EC, Hauer L, Kunz AB, Sellner J (2021) Systematic review of cases of acute myelitis in individuals with COVID-19. Eur J Neurol 28(10):3230–3244. https://doi.org/10.1111/ene.14952
Acknowledgements
The authors would like to thank the departments of Neurosurgery and Physical Medicine and Rehabilitation of Isfahan University of Medical Sciences, Isfahan, Iran. In addition, this work could not be completed without receiving valuable comments from the Department of Radiology, University of California, San Diego Health, San Diego, California, USA.
Author information
Authors and Affiliations
Contributions
Arman S contributed to the conception of the work, data search, data extraction, manuscript preparation, manuscript revision, final approval of the manuscript and agreed to be accountable for all aspects of the work.
NV contributed to manuscript preparation, data verification, English language processing, final approval of the manuscript and agreed to be accountable for all aspects of the work.
CS contributed to manuscript preparation, scientific review, English language processing, final approval of the manuscript and agreed to be accountable for all aspects of the work.
OH contributed to manuscript preparation, scientific review, English language processing, final approval of the manuscript and agreed to be accountable for all aspects of the work.
MR contributed to data gathering, scientific review, final approval of the manuscript and agreed to be accountable for all aspects of the work.
MF contributed to manuscript preparation, final approval of the manuscript and agreed to be accountable for all aspects of the work.
RM contributed to manuscript revision and English language editing, final approval of the manuscript and agreed to be accountable for all aspects of the work.
Armin. S contributed to data verification, article review, final approval of the manuscript and agreed to be accountable for all aspects of the work.
SBM contributed to the conception of the work, data search, data extraction, manuscript preparation, manuscript revision, final approval of the manuscript and agreed to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1. Search strings
Search string for PubMed
((“Spinal Hematoma”[Title/Abstract] OR “Subdural Hematoma*”[Title/Abstract] OR “Subdural Hemorrhage*”[Title/Abstract] OR SDH[Title/Abstract] OR “Subarachnoid Hemorrhage*”[Title/Abstract] OR SAH[Title/Abstract] OR “Epidural Hemorrhage*”[Title/Abstract] OR “Extradural Hematoma*”[Title/Abstract] OR EDH[Title/Abstract] OR Hematomyelia[Title/Abstract] OR “Spinal Cord Hemorrhage*”[Title/Abstract]) OR (“Hematoma, Subdural”[Mesh] OR “Subarachnoid Hemorrhage” [Mesh] OR “Hematoma, Epidural, Spinal” [Mesh] OR “Spinal Cord Vascular Diseases” [Mesh])) AND ((COVID-19[Title/Abstract] OR SARS-CoV-2[Title/Abstract] OR 2019-nCoV[Title/Abstract] OR “Coronavirus Disease 19”[Title/Abstract] OR “2019 Novel Coronavirus”[Title/Abstract]) OR (COVID-19 [Mesh] OR SARS-CoV-2 [Mesh]))
167 Records [with these filters: Full text, Humans, English]
Search string for Web of Science
“Spinal Hematoma” OR “Subdural Hematoma*” OR “Subdural Hemorrhage*” OR SDH OR “Subarachnoid Hemorrhage*” OR SAH OR “Epidural Hemorrhage*” OR “Extradural Hematoma*” OR EDH OR Hematomyelia OR “Spinal Cord Hemorrhage*” (All Fields) and COVID-19 OR SARS-CoV-2 OR 2019-nCoV OR “Coronavirus Disease 19” OR “2019 Novel Coronavirus” (All Fields)
316 Records [with these filters: Article, English]
Search string for Scopus
( TITLE-ABS-KEY ( “Spinal Hematoma” OR “Subdural Hematoma*” OR “Subdural Hemorrhage*” OR sdh OR “Subarachnoid Hemorrhage*” OR sah OR “Epidural Hemorrhage*” OR “Extradural Hematoma*” OR edh OR hematomyelia OR “Spinal Cord Hemorrhage*” ) AND TITLE-ABS-KEY ( covid-19 OR sars-cov-2 OR 2019-ncov OR “Coronavirus Disease 19” OR “2019 Novel Coronavirus” ) ) AND ( LIMIT-TO ( DOCTYPE , “ar” ) ) AND ( LIMIT-TO ( LANGUAGE , “English” ) ) AND ( LIMIT-TO ( SRCTYPE , “j” ) )
389 Records [with these filters: Journal, Article, English]
Search string for Embase
(‘spinal hematoma’/exp OR ‘spinal hematoma’ OR ‘subdural hematoma*’ OR ‘subdural hemorrhage*’ OR ‘sdh’/exp OR sdh OR ‘subarachnoid hemorrhage*’ OR sah OR ‘epidural hemorrhage*’ OR ‘extradural hematoma*’ OR ‘edh’/exp OR edh OR ‘hematomyelia’/exp OR hematomyelia OR ‘spinal cord hemorrhage*’) AND (‘covid 19’/exp OR ‘covid 19’ OR ‘sars cov 2’/exp OR ‘sars cov 2’ OR ‘2019 ncov’/exp OR ‘2019 ncov’ OR ‘coronavirus disease 19’/exp OR ‘coronavirus disease 19’ OR ‘2019 novel coronavirus’/exp OR ‘2019 novel coronavirus’)
469 Records [with this filter: Article]
Appendix 2
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sourani, A., Vahdat, N., Son, C. et al. SARS-CoV-2 infection and spontaneous spinal hemorrhage: a systematic review. Neurosurg Rev 46, 300 (2023). https://doi.org/10.1007/s10143-023-02211-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-023-02211-0