Abstract
The aim of this work is to investigate the long-term bleeding risk of cerebral cavernous malformation (CCM) remnants. A review of clinical, radiological, operative, and post-operative data of a cerebral cavernous malformation (CCMs) prospective database was performed. Fisher’s exact test and Mann-Whitney U-test were used to assess differences between non-hemorrhagic and hemorrhagic CCM remnants for 14 variables. Recursive partitioning analysis was performed to assess the order of variables most associated with CCM remnant bleeding. Twenty-four patients out of 126 had a CCM post-surgical remnant. Of these, 7 had at least one post-operative hemorrhagic event. The mean follow-up was 80.7 months (range 12–144). CCM post-surgical remnant bleeding presented mostly with acute headache (50%) and focal neurological deficit (25%); in the remaining cases, the hemorrhage was asymptomatic. Retreatment was performed in two patients, with surgery and radiosurgery, respectively; no treatment was performed in the majority of cases. All patients ranked as non-II, according to Zabramski classification, did not show any post-surgical bleeding. The presence of a pre-operative perilesional hemosiderin ring was highly significant in predicting post-surgical bleeding (sensitivity = 0.94, specificity = 0.88) and incorrectly predicted bleeding in only two of the 24 patients. This study provides an evaluation of clinical and radiological factors influencing the bleeding risk of a CCM post-surgical remnant in a homogeneous population. Perilesional hemosiderin ring and Zabramski Type II appear to strongly condition the bleeding risk of a CCM post-surgical remnant.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebral cavernous malformations (CCMs) are vascular lesions, histopathologically constituted by dilated vascular channels containing blood products at different stages and with a thin wall, formed by a single layer of endothelial cells and a delicate fibrous adventitia [1,2,3]. The tight junctions between the endothelial cells of these vascular caves are incomplete and dysfunctional, favoring bleeding of the lesion and the deposition of a perilesional hemosiderin ring [4, 5].
Complete surgical removal of a cerebral cavernous malformation (CCM) is mainly influenced by its size and location: lesions located in deep and/or eloquent areas might not be amenable to complete resection, leaving a lesion remnant in the surgical site [6,7,8]. CCM post-surgical remnants may be associated with various complications, including bleeding [9] and seizure [10].
Data on factors that can influence the bleeding risk of CCM remnants are limited [11, 12], and most of the studies focus on brainstem CCM remnants [13,14,15,16]. In this single-center study, based on a prospective registry of consecutive patients operated in our center, anamnestic, clinical and radiological factors were analyzed, and their possible association with the bleeding risk of CCM remnants was investigated.
Materials and methods
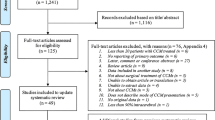
Patients who were diagnosed with a CCM post-surgical remnant on post-operative magnetic resonance imaging (MRI) were selected from a prospective database, created in 2008 at the University of Brescia.
Surgery
Surgical treatment was proposed according to the Hernesniemi grading system [17]. Radiological diagnosis was confirmed by histopathological examination. An early postoperative computer tomography (CT) scan and a 3-month MRI were performed for each patient; follow-up MRIs were usually performed every year for the first 5 years, especially if a remnant was suspected. A CCM remnant was diagnosed when a blood-containing nodule was recognized close to the surgical cavity, according to Chen B. et al. [18].
Data collection and analysis
Anamnestic, clinical, and radiological factors were retrieved from the prospectively collected database. Anamnestic and clinical data included bleeding clinical onset, patient comorbidities, pre- and post-operative drugs (i.e., antiepileptic, antiplatelet, anticoagulant, antihypertensive, hypoglycemic, cholesterol-lowering), smoke or drug addiction, CCM familiarity, and postoperative radiation therapy. Radiological data included CCM localization, pre-operative maximum diameter, presence, or absence of a perilesional pre-operative hemosiderin ring. Zabramski classification was used to rank each CCM [19]. Three-tied multi-parameter MRI-based grading system for eloquent CCM was also considered for the analysis [20].
Statistical analysis
Patients with CCM post-surgical remnant were divided into two groups based on whether or not the remnant bled. Differences between these two groups and baseline clinical variables were assessed using Fisher’s exact test, for discrete variables, and Mann-Whitney U-test, for continuous variables. A recursive partitioning analysis was used to identify the order of variables most associated with post-surgery bleeding. For the assessment of binary classification, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated. All statistical tests were two-sided. Statistical significance was defined as a p value < 0.05. The analysis was performed with R statistical software v3.4.1 (http://www.r-project.org).
Results
Out of 126 patients, who were treated at the University of Brescia from 2008 to 2018, 24 had a CCM post-surgical remnant (Table 1). The mean follow-up period was 80.7 months (range 12–144 months). Of the 24 patients, 16 did not show any bleeding, while 7 had at least one CCM post-surgical remnant bleeding. Most patients had a single bleeding episode, and only one patient presented two distinct hemorrhages. CCM post-surgical remnant bleeding was observed at a mean of 21.5 months (range 5–48 months) after surgery.
There was no sex preponderance; the mean age was 41.7 years (range 4–78). Fourteen patients presented with intracerebral hemorrhage (ICH = 56.3%), and 5 patients (21.7%) had CCM familiarity. CCM localization is reported in Table 1: deep location (58%) and dominant hemisphere locations (64%) were the most common. The mean pre-operative maximum diameter of the CCMs was 21.1 mm (range 5.6-52 mm). Ten patients were classified as type II according to Zabramski’s classification system (43.5%). In 8 patients, a perilesional hemosiderin ring was evident.
Bleeding of the CCM remnant was symptomatic in 75% of cases, occurring mostly with an acute headache (50%) and in a lower percentage of cases (25%) with the appearance of focal neurological deficit; in these cases, the bleeding was extracapsular. In the remaining cases of CCM remnant, bleeding was diagnosed during the radiological follow-up and was intracapsular (25%).
Two patients underwent treatment after the CCM remnant bleeding. A 25-year-old female patient, with a left temporal CCM remnant, presented with hemorrhage 24 months after the first treatment; she has been operated again with the resolution of bleeding and partial excision with no further bleeding (108 months of follow-up after second surgery). A 30-year-old male patient with a left cerebellar peduncle CCM remnant, who bled 12 months after surgery, underwent radiosurgical treatment, with the resolution of bleeding and ablation of part of the remnant (follow-up after radiosurgery, 136 months).
The remaining five patients with bleeding CCM remnants did not undergo any further procedure. Two reported new neurological deficits (i.e., ideomotor slowing, space-time disorientation, hemianopsia, hyposthenia), while the other three patients had no relevant clinical consequences. An example of our CCM remnant series is shown in Fig. 1.
Axial T2WI head-MRI scan. a Pre-operative head-MRI scan. CCM located between the hypothalamus, the third ventricle, and the perimesencephalic cisterns with recent bleeding causing mass effect and third ventricle displacement of 7 mm. b Post-operative head MRI scan. Post-surgical malacic area at the level of the left lenticular nucleus; in the interpeduncular cistern nodule with an axial diameter of 10 × 4 mm compatible with residual cavernoma
Furthermore, we have applied the three-tied multi-parameter MRI-based grading system for eloquent CCM [20]. Eighteen CCMs were classified as type 2, 1 CCM was classified as type 1, and 4 CCMs were classified as type 3. We were not able to prove a statistically valid correlation (p < 0.05) between the risk of bleeding and the belonging to one of three Dammann types.
Statistical analysis
Out of the 14 assessed variables, the Zabramski score and the presence of a hemosiderin ring were significantly different between the non-bleeding and bleeding groups. Patients with post-surgery bleeding were all Zabramski type II, and 88% showed the presence of a hemosiderin ring (Table 2). The two variables were highly correlated, as suggested by Fisher’s exact test (p < 0.001) and the mean square contingency coefficient (Φ = 0.77).
Other clinical and anamnestic patient factors (i.e., age, familiarity, pre- and postoperative medications, postoperative radiotherapy (RT), cardiovascular and general comorbidities, voluptuary habits and other lesion parameters, i.e., initial clinical presentation with ICH and pre-operative size) were not significantly associate to the bleeding event (Table 2).
A recursive partitioning analysis was carried out in order to identify the most significant variable in predicting post-surgery bleeding. The presence of a hemosiderin ring was selected as the most predictive variable (Fig. 2). However, 100% of the non-Zabramski type II patients did not show bleeding after surgery.
While perfect separation was not observed in any of the two variables considered with regard to post-surgery bleeding, the presence of a hemosiderin ring correctly predicted the outcome of 93.8% of patients, in contrast to Zabramski’s classification which misidentified 3 patients. The presence of a hemosiderin ring yielded a sensitivity of 0.94, a specificity of 0.88, a PPV of 0.88, and an NPV of 0.94, in contrast to Zabramski type II that showed a sensitivity of 0.81 and a specificity of 1, a PPV of 0.72, and an NPV of 1.
A model including both variables increases neither sensitivity nor specificity. No observable characteristics were identified in these two patients that could explain the missing correlation between the hemosiderin ring and bleeding.
Discussion
In this consecutive cohort of patients with CCM post-surgical remnants, the presence of hemosiderin ring and the Zabramski Type II proved the strongest predictive variables for the occurrence of post-surgical bleeding. The presence of a pre-operative perilesional hemosiderin ring is the most predictive factor of future bleeding of a CCM post-surgical remnant (Fig. 1).
The bleeding risk of CCM post-surgical remnants remains a point of open debate among the authors, with estimates reporting 40% of both cerebral and brainstem CCM remnants with at least one bleeding episode (follow-up range of 6–32 months) [9, 12].
Currently, shared guidelines on the treatment of CCM have not yet been defined, and a common opinion is still lacking, especially regarding the treatment of supratentorial CCM without cavernoma-related epilepsy [21]. In particular, in this case, the therapeutic options include open surgery and/or stereotactic radiosurgery (SRS) [21]. In the case of CCMs related to medically refractory seizures, CCM surgical resection can be a resolving therapeutic option [22]. Indeed, it has been shown that total lesionectomy results in a 70 to 90% postoperative seizure control in patients with sporadic seizures or those with seizure duration less than 1 year [23]. Conversely, there is a lower chance of seizure control after surgery in cases with longer pre-operative duration of seizures [24]. In line with these data, some authors argue for performing early surgery in patients who do not respond to single-drug therapy, even if they do not satisfy criteria for CCM medically refractory epilepsy. SRS has been proposed as an alternative treatment for symptomatic CCM in eloquent areas [25]. A meta-analysis identified 4 out of 5 studies revealing statistically significant decline in the yearly hemorrhage rate 2 years after SRS of brainstem CCM [26]. The mortality rate was 5.61%, and 11.8% developed new focal neurological deficits. An active debate as to whether the effects of SRS merely reflect the CCM natural history is ongoing.
Several factors have been previously associated with CCM bleeding risk, such as prior hemorrhage, [3, 5, 27, 28], multiplicity of CCMs [27], male gender [28], deep and subcortical location [29], and pregnancy [5]. Furthermore, the correlation between perilesional hemosiderin ring and CCM bleeding is not new in the literature [12, 30] and might be intuitive, considering that hemosiderin rings are the expression of the previous micro- and macrohemorrhages deriving from the structural instability of CCM vascular caves. However, no study describes the association between perilesional pre-operative hemosiderin ring and bleeding of CCM post-surgical remnants. A probable reason for the lack of this type of study can be found in the reduced number of CCM post-surgical remnant cases available in prospective registries. The relatively high percentage of this study might be related to the stringent definition of radiological remnant used to evaluate post-operative images [18] and to the location of the operated CCMs, which are mostly located in eloquent and deep areas.
The correlation between perilesional pre-operative hemosiderin ring and bleeding risk of CCM post-surgical remnant most likely has the same histopathological explanation (i.e., architectural instability of caves walls). The greater the instability of the CM vascular caves, the greater the perilesional hemosiderin ring, the higher the risk of bleeding.
According to the Zabramski neuroradiological grading of CCM [19], type II are lesions with typical “popcorn” appearance, with both hemorrhages and thromboses in different stages. No previous studies documented a statistically significant association between Zabramski type II pre-operative grade and higher bleeding risk of CCM post-surgical remnants. Rather, Zabramski type II lesions have been previously correlated to the clinical presentation with seizures of CCMs [29].
In this study, we underline the clinical and surgical relevance of perilesional hemosiderin ring and Zabramski type II CCMs. These variables statistically strongly condition the bleeding risk of a possible post-operative remnant, so much that the presence of these two factors should direct the surgeon toward complete removal of the lesion. However, complete surgical removal of a Zabramski type II lesion with hemosiderin ring is not an easy task, certainly from a histopathological point of view, having a high tendency to bleed, to which is added a possible localization in eloquent areas with the impossibility of complete removal in order to guarantee an adequate postoperative outcome [31]. In the context of CCM with these two pre-operative neurovascular variables, the correct path is to find the right balance between obtaining a complete removal and avoiding surgical damage to the healthy parenchyma, avoiding where practicable to leave remnants of the lesion. We believe the combination of pre-operative perilesional hemosiderin ring and Zabramski type II lesion are two possible predictors of bleeding risk of the CCM post-surgical remnant.
Limitations of the study
The main limitation of this study is represented by the small sample. We cannot exclude that the low number of patients may have hindered the identification of other risk factors for post-operative delayed bleeding in CCM remnants. The single-center analysis may also have limited the variability of the sample.
Conclusions
This study offers an analytical evaluation of clinical factors influencing the bleeding risk of a CCM post-surgical remnant in a homogeneous population of patients. The presence of a pre-operative hemosiderin ring and Zabramski type II lesion are significantly associated with the bleeding risk of the post-surgical remnant. Pre-operative perilesional hemosiderin ring has shown the greatest correlation. With the identification of these two statistically significant risk factors, we aim to give the surgeon an extra weapon in the therapeutic decision. Having to decide whether to completely remove a CCM risking neurological damage, or leave a residue knowing that there is a risk of bleeding, according to our data, the presence of hemosiderin ring and Zabramski type II are risk factors that could push toward total removal. These data will need to be confirmed by larger, multicenter series.
References
Del Curling O, Kelly DL, Elster AD, Craven TE (1991) An analysis of the natural history of cavernous angiomas. J Neurosurg 75:702–708. https://doi.org/10.3171/jns.1991.75.5.0702
McCormick WF, Hardman JM, Boulter TR (1968) Vascular malformations (“angiomas”) of the brain, with special reference to those occurring in the posterior fossa. J Neurosurg 28:241–251. https://doi.org/10.3171/jns.1968.28.3.0241
Moriarity JL, Wetzel M, Clatterbuck RE, Javedan S, Sheppard JM, Hoenig-Rigamonti K, Crone NE, Breiter SN, Lee RR, Rigamonti D (1999) The natural history of cavernous malformations: a prospective study of 68 patients. Neurosurgery 44:1166–1173. https://doi.org/10.1097/00006123-199906000-00003
Detwiler PW, Porter RW, Zabramski JM, Spetzler RF (1997) De novo formation of a central nervous system cavernous malformation: implications for predicting risk of hemorrhage. Case report and review of the literature. J Neurosurg 87:629–632. https://doi.org/10.3171/jns.1997.87.4.0629
Robinson JR, Awad IA, Little JR (1991) Natural history of the cavernous angioma. J Neurosurg 75:709–712. https://doi.org/10.3171/jns.1991.75.5.0709
Wostrack M, Shiban E, Harmening K, Obermueller T, Ringel F, Ryang Y-M, Meyer B, Stoffel M (2012) Surgical treatment of symptomatic cerebral cavernous malformations in eloquent brain regions. Acta Neurochir 154:1419–1430. https://doi.org/10.1007/s00701-012-1411-4
Bertalanffy H, Benes L, Miyazawa T, Alberti O, Siegel AM, Sure U (2002) Cerebral cavernomas in the adult. Review of the literature and analysis of 72 surgically treated patients. Neurosurg Rev 25:1–53. https://doi.org/10.1007/s101430100179
Chang EF, Gabriel RA, Potts MB, Berger MS, Lawton MT (2010) Supratentorial cavernous malformations in eloquent and deep locations: surgical approaches and outcomes. J Neurosurg 114:814–827. https://doi.org/10.3171/2010.5.JNS091159
Cenzato M, Stefini R, Ambrosi C, Giovanelli M (2008) Post-operative remnants of brainstem cavernomas: incidence, risk factors and management. Acta Neurochir 150:879–886. https://doi.org/10.1007/s00701-008-0008-4
Choudhri O, Feroze AH, Lad EM, Kim JW, Plowey ED, Karamchandani JR, Chang SD (2014) Co-occurrence of a cerebral cavernous malformation and an orbital cavernous hemangioma in a patient with seizures and visual symptoms: rare crossroads for vascular malformations. Surg Neurol Int 5:S148–S154. https://doi.org/10.4103/2152-7806.134810
Ding D, Starke RM, Crowley RW, Liu KC (2017) Surgical approaches for symptomatic cerebral cavernous malformations of the thalamus and brainstem. J Cerebrovasc Endovasc Neurosurg 19:19–35. https://doi.org/10.7461/jcen.2017.19.1.19
Mouchtouris N, Chalouhi N, Chitale A, Starke RM, Tjoumakaris SI, Rosenwasser RH, Jabbour PM (2015) Management of cerebral cavernous malformations: from diagnosis to treatment. ScientificWorldJournal 808314. 1155/2015/808314
Cenzato M, Debernardi A, Stefini R, D'Aliberti G, Piparo M, Talamonti G, Coppini M, Versari P (2012) Spinal dural arteriovenous fistulas: outcome and prognostic factors. Neurosurg Focus 32:E11. https://doi.org/10.3171/2012.2.FOCUS1218
Bozinov O, Hatano T, Sarnthein J, Burkhardt J-K, Bertalanffy H (2010) Current clinical management of brainstem cavernomas. Swiss Med Wkly 140:w13120. https://doi.org/10.4414/smw.2010.13120
Arauz A, Patiño-Rodriguez HM, Chavarria-Medina M, Becerril M, Longo GM, Nathal E (2017) Rebleeding and outcome in patients with symptomatic brain stem cavernomas. Cerebrovasc Dis 43:283–289. https://doi.org/10.1159/000463392
Gross BA, Batjer HH, Awad IA, Bendok BR, Du R (2013) Brainstem cavernous malformations: 1390 surgical cases from the literature. World Neurosurg 80(1–2):89–93
Kivelev J, Laakso A, Niemelä M, Hernesniemi J A proposed grading system of brain and spinal cavernomas. Neurosurgery 69:807–813. https://doi.org/10.1016/j.wneu.2012.04.002
Chen B, Göricke S, Wrede K, Jabbarli R, Wälchli T, Jägersberg M, Sure U, Dammann P (2017) Reliable? The value of early postoperative magnetic resonance imaging after cerebral cavernous malformation surgery. World Neurosurg 103:138–144. https://doi.org/10.1016/j.wneu.2017.03.135
Zabramski JM, Wascher TM, Spetzler RF, Johnson B, Golfinos J, Drayer BP, Brown B, Rigamonti D, Brown G (1994) The natural history of familial cavernous malformations: results of an ongoing study. J Neurosurg 80:422–432. https://doi.org/10.3171/jns.1994.80.3.0422
Dammann P, Wrede K, Jabbarli R, Müller O, Mönninghoff C, Forsting M, Sure U (2017) Of bubbles and layers: which cerebral cavernous malformations are most difficult to dissect from surrounding eloquent brain tissue? Neurosurgery 1 81(3):498–503. https://doi.org/10.1093/neuros/nyx02
Akers A, Al-Shahi Salman R, Awad IA, Dahlem K, Flemming K, Hart B, Kim H, Jusue-Torres I, Kondziolka D, Lee C, Morrison L, Rigamonti D, Rebeiz T, Tournier-Lasserve E, Waggoner D, Whitehead K (2017) Synopsis of guidelines for the clinical management of cerebral cavernous malformations: consensus recommendations based on systematic literature review by the angioma alliance scientific advisory board clinical experts panel. Neurosurgery 80(5):665–680. https://doi.org/10.1093/neuros/nyx091
Von der Brelie C, Von Lehe M, Raabe A, Niehusmann P, Urbach H, Mayer C, Elger CE, Malter MP (2014) Surgical resection can be successful in a large fraction of patients with drug-resistant epilepsy associated with multiple cerebral cavernous malformations. Neurosurgery 74(2):147–153. https://doi.org/10.1227/NEU.0000000000000210
Ferroli P, Casazza M, Marras C, Mendola C, Franzini A, Broggi G (2006) Cerebral cavernomas and seizures: a retrospective study on 163 patients who underwent pure lesionectomy. Neurol Sci 26(6):390–394. https://doi.org/10.1007/s10072-006-0521-2
Von der Brelie C, Kuczaty S, Von Lehe M (2014) Surgical management and long-term outcome of pediatric patients with different subtypes of epilepsy associated with cerebral cavernous malformations. J Neurosurg Pediatr 13(6):699–705. https://doi.org/10.3171/2014.2.PEDS13361
Gross BA, Batjer HH, Awad IA, Bendok BR, Du R (2013) Brainstem cavernous malformations: 1390 surgical cases from the literature. World Neurosurg 80(1–2):89–93. https://doi.org/10.1016/j.wneu.2012.04.002
Lu X-Y, Sun H, Xu J-G, Li Q-Y (2014) Stereotactic radiosurgery of brainstem cavernous malformations: a systematic review and meta-analysis. J Neurosurg 120(4):982–987. https://doi.org/10.3171/2013.12.JNS13990
Flemming KD, Link MJ, Christianson TJH, Brown RD (2012) Prospective hemorrhage risk of intracerebral cavernous malformations. Neurology. 78:632–636. https://doi.org/10.1212/WNL.0b013e318248de9b
Aiba T, Tanaka R, Koike T, Kameyama S, Takeda N, Komata T (1995) The natural history of intracranial cavernous malformations. J Neurosurg 83:56–59. https://doi.org/10.3171/jns.1995.83.1.0056
Agosti E, Flemming KD, Lanzino G (2019) Symptomatic cavernous malformation presenting with seizure without hemorrhage: analysis of factors influencing clinical presentation. World Neurosurg 129:e387–e392. https://doi.org/10.1016/j.wneu.2019.05.157
Al-Shahi Salman R, Berg MJ, Morrison L, Awad I (2008) Hemorrhage from cavernous malformations of the brain: definition and reporting standards. Angioma Alliance Scientific Advisory Board. Stroke 39:3222–3230. https://doi.org/10.1161/STROKEAHA.108.515544
Nikoubashman O, Di Rocco F, Davagnanam I, Zerah M, Wiesmann M (2015) Prospective hemorrhage rates of cerebral cavernous malformations in children and adolescents based on MRI appearance. Am J Neuroradiol 36:2177–2183. https://doi.org/10.3174/ajnr.A4427
Funding
Open access funding provided by Università degli Studi di Brescia within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
We received approval by the Brescian Ethical Committee with the code NET-2013-02357109.
Informed consent
Informed consent was obtained for all patients participating in this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fontanella, M.M., Agosti, E., Zanin, L. et al. Cerebral cavernous malformation remnants after surgery: a single-center series with long-term bleeding risk analysis. Neurosurg Rev 44, 2639–2645 (2021). https://doi.org/10.1007/s10143-020-01436-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-020-01436-7