Abstract
Ultrasonography, a radiation-free and cost-effective modality, stands out as a promising tool for evaluating nasal bone fractures. Despite limited literature on its pediatric application, there is an increasing recognition of its potential to enhance diagnostic precision. To evaluate the diagnostic efficacy of ultrasound in detecting pediatric nasal bone fractures. Employing established guidelines, a systematic review and meta-analysis were conducted through a comprehensive literature search in PubMed, Scopus, Web of Science, and Embase databases until December 5, 2023. Inclusion criteria encompassed studies reporting diagnostic accuracy measures of ultrasound in pediatric patients with nasal bone fractures. Data extraction and analysis were undertaken for the selected studies. Involving four studies with 277 patients, ultrasound demonstrated a pooled sensitivity of 66.1% (95% CI: 35.1-87.5%) and specificity of 86.8% (95% CI: 80.1-91.4%) in diagnosing pediatric nasal fractures. The area under the receiver operating characteristic curve (AUC) was 0.88 (95% CI: 0.72–0.93). After excluding an outlier study, sensitivity and specificity increased to 78.0% (95% CI: 65.6-86.9%) and 87.8 (95% CI: 78.1-93.6%), respectively, with an AUC of 0.79 (95% CI: 0.75–0.94). Pooled positive and negative likelihood ratios were 5.11 (95% CI: 2.12–9.15) and 0.40 (95% CI: 0.14–0.77) before exclusion and 6.75 (95% CI: 3.47–12.30) and 0.26 (95% CI: 0.15–0.40) after exclusion of an outlier study, respectively. This study highlighted ultrasonography’s utility in diagnosing pediatric nasal bone fractures with high accuracy and specificity. However, caution is advised in relying solely on ultrasound due to suboptimal overall diagnostic performance, evident in likelihood ratios.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pediatric nasal bone fractures are highly prevalent, constituting 40–50% of facial fractures in children [1,2,3]. The untreated consequences of these fractures can lead to both cosmetic and functional impairments, underscoring the critical need for accurate and timely diagnosis [4, 5].
While physical examination is widely acknowledged as the gold standard for diagnosing nasal fractures [1, 6], challenges arise when significant post-traumatic swelling occurs, hindering the prompt identification of deformities [7], especially in younger age patients who have higher amount of cartilage in nasal structures [4], [5]. Furthermore, the subjective nature of physical examination necessitates the exploration of supplementary objective imaging techniques, particularly for comprehensive documentation, often for legal purposes. This requirement is accentuated in pediatric cases, where the inherent challenges of patient non-compliance further complicate the efficacy of physical examinations [4,5,6]. Traditional imaging methods, including X-rays and computed tomography (CT) scans, present limitations in sensitivity, specificity, and concerns about radiation exposure [8, 9]. In this context, ultrasonography emerges as a promising method for evaluating pediatric nasal bone fractures. This imaging modality can detect skeletal deformation along three axes without radiation exposure. Its cost-effectiveness, especially in resource-limited settings, and the improved quality of results due to the absence of an air gap between the transducer and bones make it a valuable diagnostic tool. Furthermore, owing to the portability of ultrasound devices, their utility extends beyond hospital environments, proving invaluable in situations involving multiple trauma patients. This advantage enables swift assessment and diagnosis without the constraints associated with bulkier imaging modalities [1, 10, 11].
Prior research has investigated the effectiveness of ultrasound in the diagnosis of nasal bone fractures, yielding promising outcomes [11,12,13]. However, the literature on its application in detecting nasal bone fractures in the pediatric population is limited. The present systematic review and meta-analysis aim to evaluate the diagnostic utility of ultrasound for nasal bone fractures, examining its sensitivity, specificity, and other diagnostic accuracy measures in the pediatric population.
Methods
This systematic review adheres to the guidelines established in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [14]. The literature search, initiated on December 5, 2023, spanned four major databases: PubMed, Scopus, Web of Science, and Embase. Distinct search terms tailored for each database included (“nasal” OR “midfacial”) AND (“fracture*”) AND (“sonograph*” OR “ultrasonograph*” OR “ultrasound” OR “POCUS”) AND (“pediatric*” OR “paediatric*” OR “child*” OR “neonat*” OR “infant*” OR “toddler*” OR “preschool” OR “pre-school” OR “juvenile” OR “young adult*”). Additionally, a meticulous manual examination of references within the selected studies ensured comprehensive coverage. The review process involved a thorough evaluation of each article’s title, abstract, and/or full text, conducted independently by two co-authors. Uncertainties or ambiguities were addressed through consultation with a senior co-author. Deduplication, screening, and data extraction were facilitated by the AutoLit platform, developed by Nested Knowledge in St. Paul, Minnesota, USA.
All studies relevant to the diagnostic accuracy of ultrasound in pediatric patients (under 21 years old) were considered for inclusion if they presented at least one of the following diagnostic measures: sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), likelihood ratio (LR), diagnostic odds ratio (DOR), and area under the receiver operating characteristic curve (AUC). No restrictions were imposed on publication date, country of origin, patient characteristics, reference standard type, or study design. Non-English literature, case reports, case series with fewer than five eligible patients, conference abstracts, editorial comments, and review articles were excluded from the study.
Details extracted from each qualifying paper included the first author’s name, publication year, study design, sample size, participant and fracture characteristics, reference standard modality, ultrasound operator, type of ultrasound device, type of ultrasound probe, image acquisition methods, ultrasound features indicating nasal bone fractures, and diagnostic accuracy measures of ultrasound.
The quality assessment utilized the Diagnostic Accuracy Studies-2 (QUADAS-2) tool to evaluate included studies’ quality [15]. Independent assessments for potential bias and concerns regarding applicability were conducted for the four primary domains of the QUADAS-2 tool: patient selection, index test, reference standard, and flow and timing. Specific criteria outlined in the tool, such as the representativeness of the study population, blinding of test results, and completeness of outcome data, informed evaluations for each domain. Ratings of “low,” “high,” or “unclear” were assigned to determine the overall rigor and reliability of the evidence synthesis.
Statistical analysis
The analysis employed a random effects diagnostic test accuracy (DTA) model, specifically utilizing the bivariate model proposed by Reitsma et al. [16]. Summary Receiver Operating Characteristic (SROC) curves were generated based on the bivariate meta-analysis data, with study-specific estimates weighted in the random effects univariate DOR model. The AUC and its confidence interval (CI) for each subgroup were determined through 2000 sample bootstrapping, utilizing the bivariate model [17].
Heterogeneity assessment relied on the I2 metric, following the method outlined by Holling et al. [18], where an I2 CI exceeding 50% signified significant heterogeneity. Sensitivity analyses using the DOR univariate meta-analysis were conducted to identify potential outliers in the presence of significant heterogeneity. If outliers were identified, a re-analysis was performed to validate the results. The clinical relevance of the findings was explored using Fagan plots and likelihood ratio scattergrams, where positive likelihood ratios above 10 indicated confirmation suitability, and negative ratios below 0.1 suggested suitability for exclusion. Fagan nomograms were constructed for assumed pre-test prevalences of 25%, 50%, and 75%, based on the bivariate Reitsma model, as detailed by Zwinderman et al. [19].
All analyses were executed in R (version 4.3.2, R Foundation for Statistical Computing, Vienna, Austria), utilizing packages such as “mada,” “dmetatools” [20], “Metafor” [21], and “meta” [22].
Results
Screening and selection of articles
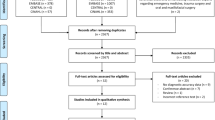
The initial phase involved a systematic literature search using a predefined strategy, resulting in the identification of 173 articles. After the removal of duplicates, 79 papers underwent screening based on title and abstract. Subsequently, 68 articles were excluded during this initial screening phase. The full text of the remaining 11 papers underwent review. Following a thorough examination, 7 articles were excluded due to insufficient numerical data, preventing the calculation of required values for conducting diagnostic test accuracy meta-analysis. Eventually, 4 articles that met the inclusion criteria were identified and included in the study. The screening process and eligibility criteria were in accordance with PRISMA guidelines, and a visual representation is provided in Fig. 1.
Study and patient characteristics
The meta-analysis incorporated four studies that evaluated the efficacy of ultrasound in diagnosing pediatric nasal bone fractures. Together, these studies investigated 277 pediatric patients, employing various ultrasound devices. The inclusion criteria across studies typically involved participants aged ≤ 18 with isolated nasal trauma, excluding cases with multiple traumas. The reference tests in all included studies relied on physical examination; however, the testing protocols varied between examinations conducted by emergency physicians [8] and those carried out by otolaryngologists [1, 6] and plastic surgeons [9]. Additional information regarding the studies, characteristics of the patients, and details of the ultrasound examinations can be found in Table 1.
Quality assessment
The quality assessment of the included studies is detailed in Table 2. These studies primarily exhibited bias related to the reference standard test, which stemmed from the use of physical examination, an inherently subjective method reliant on the examiner’s expertise. Furthermore, two studies [6, 8] in the review did not clearly specify sonographic criteria for diagnosing nasal fractures. Additionally, one study [9] exclusively employed CT scans as a reference test for patients with suspected nasal fractures in ultrasound results, rather than uniformly applying it to all patients. In summary, the review suggests a moderate overall quality of the included studies.
Meta-analysis
The meta-analysis results from four studies assessing the accuracy of ultrasonography for pediatric nasal bone fractures revealed pooled sensitivity and specificity values of 66.1% (95% CI: 35.1-87.5%) and 86.8% (95% CI: 80.1-91.4%), as illustrated in Fig. 2. The AUC for the SROC curve was 0.88 (95% CI: 0.72–0.93), as depicted in Fig. 3.
Figure 4 presents a scattergram of positive and negative likelihood ratios, indicating a test performance ranging from low to moderate. This performance level is suboptimal for both exclusion and confirmation purposes. The pooled positive and negative likelihood ratios were 5.11 (95% CI: 2.12–9.15) and 0.40 (95% CI: 0.14–0.77), respectively.
Likelihood ratio scattergram of included studies indicating low to moderate test performance suboptimal for both exclusion and confirmation purposes. LLQ. Left lower quadrant. LRN. Likelihood ratio, negative. LRP. Likelihood ratio, positive. LUQ. Left upper quadrant. RLQ. Right lower quadrant. RUQ. Right upper quadrant
In the Fagan plot study, considering pre-test probabilities of 25%, 50%, and 75% for pediatric nasal bone fractures, the positive post-test probabilities are 63%, 84%, and 94%, while the negative post-test probabilities are 12%, 29%, and 55%, respectively (Fig. 5).
The meta-analysis revealed substantial heterogeneity, as illustrated in Fig. 2. To pinpoint potential outliers and explore the origin of this heterogeneity, an influential analysis was undertaken. This analysis identified the study by Dogan et al. [8] as a significant outlier (Supplementary Fig. 1).
Meta-analysis following the exclusion of an outlier study
The meta-analysis of the three remaining studies revealed pooled sensitivity and specificity values of 78.0% (95% CI: 65.6-86.9%) and 87.8 (95% CI: 78.1-93.6%), with a moderate level of heterogeneity, as depicted in Supplementary Fig. 2. The AUC for the SROC curve was 0.79 (95% CI: 0.75–0.94), as shown in Supplementary Fig. 3.
Supplementary Fig. 4 presents a scattergram of positive and negative likelihood ratios after excluding one outlier study, indicating a test performance ranging from low to moderate, which is suboptimal for both exclusion and confirmation purposes. The pooled positive and negative likelihood ratios were 6.75 (95% CI: 3.47–12.30) and 0.26 (95% CI: 0.15–0.40), respectively.
In the Fagan plot study, considering pre-test probabilities of 25%, 50%, and 75% for pediatric nasal bone fractures, the positive post-test probabilities are 69%, 87%, and 95%, while the negative post-test probabilities are 8%, 20%, and 44%, respectively (Supplementary Fig. 5).
Discussion
In this systematic review and meta-analysis, ultrasonography exhibited a significant level of diagnostic accuracy in identifying nasal bone fractures in children. Importantly, even with the inclusion of more homogeneous studies, this finding remained consistent, as evidenced by a minimal difference of approximately 0.10 in the AUC. The analysis revealed that the pooled specificity of ultrasonography was significantly higher than its pooled sensitivity, both across the four included studies and even after excluding one outlier study. However, the test overall performance, as indicated by likelihood ratios, was observed to be low to moderate for both exclusion and confirmation purposes.
A meta-analysis involving 1480 patients, with no age restrictions, revealed that ultrasonography achieved a pooled sensitivity of 87.2% and specificity of 87.4% in diagnosing nasal bone fractures. The study suggests that ultrasonography surpasses plain radiography in sensitivity, specificity, PPV, and NPV. Moreover, CT scans showed only marginally higher performance indices compared to ultrasonography, except for specificity. This implies that, overall, the diagnostic accuracy for nasal bone fractures appears comparable between these studied imaging techniques [12]. In a separate meta-analysis centered on facial bone fractures, utilizing CT scans as the reference standard and with no age restrictions, ultrasonography exhibited remarkable sensitivity and specificity rates of 99% and 94%, respectively, in diagnosing nasal bone fractures. These results emphasize the strong diagnostic capabilities of ultrasonography for nasal bone fractures compared to CT scans [13].
Our findings indicated a lower pooled sensitivity compared to the two meta-analyses mentioned earlier. It is important to acknowledge that ultrasonography encounters inherent limitations in assessing bones during childhood. Nasal bones in younger children are less prominent and not fully ossified. The ongoing process of ossification results in anatomical variations during different stages of childhood, potentially contributing to the increased difficulty of utilizing ultrasonography for fracture detection [23]. Additionally, a study involving 423 patients with nasal bone fractures revealed significant differences in the most prevalent fracture types between children under 12 years old and adults. In this study, Yabe et al. observed that the most common type of nasal bone fracture in children was unilateral bone displacement without posterior shift, whereas bilateral displacement was more prevalent in older patients [24]. Moreover, the diagnosis of nasal bone fractures in children presents greater challenges due to factors such as smaller body size and reduced cooperativeness compared to adults [25].
In the current study, the pooled positive and negative likelihood ratios suggest that ultrasound’s overall diagnostic performance is approximately moderate but falls short of an ideal level. These findings emphasize the importance of exercising caution when solely relying on ultrasound for definitive diagnostic decisions in pediatric nasal bone fractures. There is potential value in supplementing ultrasound with other imaging modalities or diagnostic approaches. This also emphasizes the need for additional research and refinement to improve diagnostic accuracy and reliability of ultrasound in this context.
In our analysis, the study conducted by Dogan et al. emerged as an outlier, leading to an 11.8% reduction in the pooled sensitivity in our findings. Their study reported a sensitivity of 22.5% and a specificity of 83.1%. They attributed the low sensitivity to the younger age and higher number of their patients. Additionally, the determination of the presence of a fracture relied on a physical examination by an emergency physician specialist, while the sonography was performed by a radiologist. The clarity of whether the radiologists were aware of the diagnosis during the sonography was not provided [8]. Furthermore, their study exclusively included patients with isolated nasal fractures who did not meet the criteria for a CT scan. It is worth mentioning that in two other included studies, the diagnosis was established through the physical examination by an otolaryngologist [1, 6]. Tamada et al., on the other hand, considered serial physical examinations by emergency physicians or general pediatric registrars as the ground truth. Additionally, they followed patients with a negative physical examination for nasal fracture a few days after the initial visit. If symptoms persisted, a second ultrasonography was conducted, confirming a nasal fracture in four more patients and raising the sensitivity to 91.7% [9]. However, we included only the initial results to align with the approach taken in other included studies.
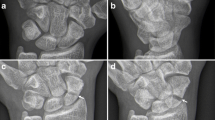
It is also important to emphasize that enhancing the diagnostic performance of ultrasonography can be achieved by incorporating physical signs of a nasal bone fracture. This is demonstrated in the study by Hong et al., where the absence of edema and hypoechoic hematoma is identified as distinguishing features that can differentiate an old fracture line from acute trauma [26].
While the current meta-analysis provided compelling findings regarding the diagnostic efficacy of ultrasound in detecting nasal bone fractures in children, certain limitations should be acknowledged. Although the reference test across all included studies was physical examination, factors such as the operator’s expertise, patient age groups, types of fractures, criteria used for definition of fractures, transducer resolution, adherence to standardized imaging protocols, real-time visualization, interpretation of results during imaging, and the time elapsed from injury to imaging may influence the diagnostic validity of ultrasonography in detecting fractures [27]. These factors serve as potential sources of heterogeneity in the study. However, the limited number of studies on this topic constrained our ability to conduct meta-regression or subgroup analysis to assess the impact of these factors on diagnostic performance. It also remains unclear whether the results of the physical examination and medical history were blinded to the sonography operator in all the studies included in our analysis. Moreover, observer bias is a limitation attributed to the superficial nature of the nasal bone. Ultrasound operators might be influenced by visible deformities when interpreting images, potentially resulting in an overestimation of ultrasound accuracy.
Conducting additional well-designed studies with larger sample sizes and rigorous methodologies is essential. These studies should include blinding sonography operators to physical examination and medical history results, while also comparing various standardized diagnostic protocols and imaging modalities. These investigations should aim to explore the potential impact of the various factors mentioned above on the diagnostic performance of ultrasound in children with nasal bone fractures.
Conclusion
This study highlighted the utility of ultrasonography as a diagnostic tool for pediatric nasal bone fractures, particularly due to its high accuracy and specificity. Following the exclusion of an outlier study, the analysis also revealed a notable level of sensitivity for this modality in this context. However, the suboptimal overall diagnostic performance of ultrasound, as indicated by likelihood ratios, underscores the importance of exercising caution in relying solely on ultrasound and highlights the necessity for additional diagnostic methods and further refinement in clinical practice. Researchers are encouraged to conduct additional large-scale studies to improve the generalizability of findings. Specifically, they should investigate the impact of potential factors on the diagnostic performance of ultrasound in this area, contributing more robust evidence to the field.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Noy R, Gvozdev N, Ilivitzki A, Nasrallah N, Gordin A (2023) Ultrasound for management of pediatric nasal fractures. Rhinology 61:568–573
Navaratnam R, Davis T (2019) The role of ultrasound in the diagnosis of pediatric nasal fractures. J Craniofac Surg 30:2099–2101
Tolley PD, Massenburg BB, Manning S, Lu GN, Bly RA (2023) Pediatric nasal and septal fractures. Oral Maxillofac Surg Clin North Am 35:577–584
Yu H, Jeon M, Kim Y, Choi Y (2019) Epidemiology of violence in pediatric and adolescent nasal fracture compared with adult nasal fracture: an 8-year study. Arch Craniofac Surg 20:228–232
Landeen KC, Kimura K, Stephan SJ (2022) Nasal fractures. Facial Plast Surg Clin North Am 30:23–30
Gökçen E, Savrun A, Kuşdoğan M et al (2021) Ability of bedside ultrasonography to detect pediatric nasal bone fractures. Laryngoscope 131:1398–1403
Kim L, Huddle MG, Smith RM, Byrne P (2020) 1.10-Nasal fractures. Dorafshar AH, Rodriguez ED, Manson PN, Facial Trauma Surgery. London: Elsevier 122–128
Dogan S, Kalafat UM, Yüksel B, Karaboğa T, Basturk M, Ocak T (2017) Use of radiography and ultrasonography for nasal fracture identification in children under 18 years of age presenting to the ED. Am J Emerg Med 35:465–468
Tamada I, Mori T, Inoue N (2017) An algorithmic approach using ultrasonography in the diagnosis of pediatric nasal bone fracture. J Craniofac Surg 28:84–87
Ardeshirpour F, Ladner KM, Shores CG, Shockley WW (2013) A preliminary study of the use of ultrasound in defining nasal fractures: criteria for a confident diagnosis. Ear Nose Throat J 92:508–512
Caglar B, Serin S, Akay S (2017) The accuracy of bedside USG in the diagnosis of nasal fractures. Am J Emerg Med 35:1653–1656
Hwang K, Jung JS, Kim H (2018) Diagnostic performance of plain film, ultrasonography, and computed tomography in nasal bone fractures: a systematic review. Plast Surg (Oakv) 26:286–292
Gadicherla S, Pentapati KC, Rustaqi N, Singh A, Smriti K (2021) Diagnostic accuracy of ultrasonography for the assessment of maxillofacial fractures: a meta-analysis. J Int Soc Prev Community Dent 11:503–509
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Whiting PF, Rutjes AW, Westwood ME et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536
Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH (2005) Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol 58:982–990
Noma H, Matsushima Y, Ishii R (2021) Confidence interval for the AUC of SROC curve and some related methods using bootstrap for meta-analysis of diagnostic accuracy studies. Commun Stat Case Stud Data Anal Appl 7:344–358
Holling H, Böhning W, Masoudi E, Böhning D, Sangnawakij P (2020) Evaluation of a new version of I2 with emphasis on diagnostic problems. Commun Stat Case Stud Data Anal Appl 49:942–972
Zwinderman AH, Bossuyt PM (2008) We should not pool diagnostic likelihood ratios in systematic reviews. Stat Med 27:687–697
Noma H (2023) MVPBT: R package for publication bias tests in meta-analysis of diagnostic accuracy studies. arXiv Available via: https://arxiv.org/abs/2209.07270. Accessed: October 20, 2023
Viechtbauer W (2010) Conducting meta-analyses in R with the metafor package. J Stat Softw 36:1–48
Balduzzi S, Rücker G, Schwarzer G (2019) How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health 22:153–160
Poboży T, Konarski W, Piotrowska-Lis K, Domańska J, Poboży K, Kielar M (2022) Basic differences and most common findings in ultrasound examinations of musculoskeletal system in children: a narrative literature review. Healthc (Basel) 10:2010
Yabe T, Tsuda T, Hirose S, Ozawa T (2012) Comparison of pediatric and adult nasal fractures. J Craniofac Surg 23:1364–1366
Kopacheva-Barsova G, Arsova S (2016) The impact of the nasal trauma in childhood on the development of the nose in future. Open Access Maced J Med Sci 4:413–419
Hong HS, Cha JG, Paik SH (2007) High-resolution sonography for nasal fracture in children. AJR Am J Roentgenol 188:W86–92
Adeyemo WL, Akadiri OA (2011) A systematic review of the diagnostic role of ultrasonography in maxillofacial fractures. Int J Oral Maxillofac Surg 40:655–661
Acknowledgements
Recognizing the utilization of ChatGPT, an OpenAI-developed language model based on the GPT-3.5 framework, enhanced the precision of language in the manuscript editing process. This collaborative endeavor led to enhanced readability and elevated linguistic quality. Nonetheless, the authors meticulously reviewed and edited the content as necessary, taking full responsibility for the substance of the publication.
Funding
No funding was received from public, commercial, or not-for-profit sectors for this research. The authors have no relevant financial or non-financial interests to disclose.
Open access funding provided by SCELC, Statewide California Electronic Library Consortium
Author information
Authors and Affiliations
Contributions
The project’s conception was shaped by the collaborative efforts of all authors. Ali Gholamrezanezhad and Pauravi S. Vasavada provided valuable scientific insights during the revision phase. Amir Hassankhani, Melika Amoukhteh, Delaram J. Ghadimi, and Nikoo Saeedi played pivotal roles in conducting database searches, extracting data, drafting, and critically revising the manuscript to include essential intellectual content. Mobina Fathi, Shirin Yaghoobpoor, and Paniz Adli made significant contributions to drafting the manuscript. Payam Jannatdoust and Parya Valizadeh made significant contributions to data analysis and interpretation. The final manuscript underwent a thorough review by all authors and received unanimous approval.
Corresponding author
Ethics declarations
Leadership role
Ali Gholamrezanezhad serves as the Director of Clinical Research at the Department of Radiology in the Keck School of Medicine of USC. Pauravi S. Vasavada holds the position of Director of Medical Student Education at Case Western Reserve University School of Medicine. Furthermore, she serves as the Co-director of the Women in Radiology Interest Group at the same institution
Competing interests
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hassankhani, A., Amoukhteh, M., Jannatdoust, P. et al. Diagnostic utility of ultrasound in pediatric nasal bone fractures: a systematic review and meta-analysis. Emerg Radiol 31, 417–428 (2024). https://doi.org/10.1007/s10140-024-02225-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-024-02225-1