Abstract
Purpose
To evaluate the role of specific distributions of free air in predicting the location of gastrointestinal (GI) tract perforation.
Materials and methods
One hundred and fifteen patients with surgically proven GI tract perforation between January 2015 and June 2019 were included in the study. The site of perforation was based on surgical findings in all cases. Two radiologists retrospectively interpreted the computed tomography (CT) images of these patients for extraluminal free air distribution. Perforation sites were demonstrated intraoperatively in all cases and were categorized as follows: stomach and duodenum, jejunum and ileum, proximal colon (cecum, ascending colon, and transverse colon), distal colon (descending colon and sigmoid colon), rectum, and appendix.
Results
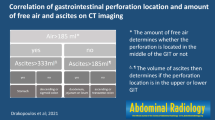
There were 79 male and 36 female patients with a mean age of 56.4 years. Periportal, perihepatic, and perigastric free air were statistically significant in predicting gastroduodenal perforation. Mesenteric free air was significant in predicting both small bowel and distal colon perforations. Pelvic free air was statistically significant in distal colon perforations. Periappendiceal free air was found to be a strong predictor of acute perforated appendicitis.
Conclusion
Specific free air distributions may help to predict the site of gastrointestinal perforation, which would change the treatment plan.






Similar content being viewed by others
Data availability
The datasets during and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Knight DJ, Girling KJ (2003) Gut flora in health and disease. Lancet 361(9371):1831. https://doi.org/10.1016/s0140-6736(03)13438-1
Ordoñez CA, Puyana JC (2006) Management of peritonitis in the critically ill patient. Surg Clin North Am 86:1323–1349. https://doi.org/10.1016/j.suc.2006.09.006
Langell JT, Mulvihill SJ (2008) Gastrointestinal perforation and the acute abdomen. Med Clin North Am 92:599–625. https://doi.org/10.1016/j.mcna.2007.12.004 (viii-ix)
Siu WT, Chau CH, Law BK, Tang CN, Ha PY, Li MK (2004) Routine use of laparoscopic repair for perforated peptic ulcer. Br J Surg 91:481–484. https://doi.org/10.1002/bjs.4452
Hainaux B, Agneessens E, Bertinotti R, De Maertelaer V, Rubesova E, Capelluto E, Moschopoulos C (2006) Accuracy of MDCT in predicting site of gastrointestinal tract perforation. Am J Roentgenol 187:1179–1183. https://doi.org/10.2214/AJR.05.1179
Francavilla ML, Pollock AN (2017) Perforated duodenal ulcer. Pediatr Emerg Care 33:219–220. https://doi.org/10.1097/PEC.0000000000001060
Yeung KW, Chang MS, Hsiao CP, Huang JF (2004) CT evaluation of gastrointestinal tract perforation. Clin Imaging 28:329–333. https://doi.org/10.1016/S0899-7071(03)00204-3
Miki T, Ogata S, Uto M, Nakazono T, Urata M, Ishibe R, Shinyama S, Nakajo M (2004) Multidetector-row CT findings of colonic perforation: direct visualisation of ruptured colonic wall. Abdom Imaging 29:658–662. https://doi.org/10.1007/s00261-003-0159-y
Ghekiere O, Lesnik A, Hoa D, Laffargue G, Uriot C, Taourel P (2007) Value of computed tomography in the diagnosis of the cause of nontraumatic gastrointestinal tract perforation. J Comput Assist Tomogr 31:169–176. https://doi.org/10.1097/01.rct.0000237809.11123.8e
Maniatis V, Chryssikopoulos H, Roussakis A, Kalamara C, Kavadias S, Papadopoulos A, Andreou J, Stringaris K (2000) Perforation of the alimentary tract: evaluation with computed tomography. Abdom Imaging 25:373–379. https://doi.org/10.1007/s002610000022
Furukawa A, Sakoda M, Yamasaki M, Kono N, Tanaka T, Nitta N, Kanasaki S, Imoto K, Takahashi M, Murata K, Sakamoto T, Tani T (2005) Gastrointestinal tract perforation: CT diagnosis of presence, site, and cause. Abdom Imaging 30:524–534. https://doi.org/10.1007/s00261-004-0289-x
Imuta M, Awai K, Nakayama Y, Murata Y, Asao C, Matsukawa T, Yamashita Y (2007) Multidetector CT findings suggesting a perforation site in the gastrointestinal tract: analysis in surgically confirmed 155 patients. Radiat Med 25:113–118. https://doi.org/10.1007/s11604-006-0112-4
Brofman N, Atri M, Hanson JM, Grinblat L, Chughtai T, Brenneman F (2006) Evaluation of bowel and mesenteric blunt trauma with multidetector CT. Radiographics 26:1119–1131. https://doi.org/10.1148/rg.264055144
Toprak H, Yilmaz TF, Yurtsever I, Sharifov R, Gültekin MA, Yiğman S, Yildiz Ş (2019) Multidetector CT findings in gastrointestinal tract perforation that can help prediction of perforation site accurately. Clin Radiol 74:736.e1-736.e7. https://doi.org/10.1016/j.crad.2019.06.005
Earls JP, Dachman AH, Colon E, Garrett MG, Molloy M (1993) Prevalence and duration of postoperative pneumoperitoneum: sensitivity of CT vs left lateral decubitus radiography. AJR Am J Roentgenol 161:781–785. https://doi.org/10.2214/ajr.161.4.8372757
Songne B, Jean F, Foulatier O, Khalil H, Scotté M (2004) Traitement non opératoire des perforations d’ulcère gastroduodénal. Résultats d’une étude prospective [Non operative treatment for perforated peptic ulcer: results of a prospective study]. Ann Chir 129:578–82. https://doi.org/10.1016/j.anchir.2004.06.012 (French)
van Dijk ST, Rottier SJ, van Geloven AAW, Boermeester MA (2017) Conservative treatment of acute colonic diverticulitis. Curr Infect Dis Rep 23(19):44. https://doi.org/10.1007/s11908-017-0600-y
Cao F, Li J, Li A, Fang Y, Wang YJ, Li F (2014) Nonoperative management for perforated peptic ulcer: who can benefit? Asian J Surg 37:148–153. https://doi.org/10.1016/j.asjsur.2013.10.002
Grassi R, Romano S, Pinto A, Romano L (2004) Gastro-duodenal perforations: conventional plain film, US and CT findings in 166 consecutive patients. Eur J Radiol 50:30–36. https://doi.org/10.1016/j.ejrad.2003.11.012
Kim HC, Yang DM, Kim SW, Park SJ (2014) Gastrointestinal tract perforation: evaluation of MDCT according to perforation site and elapsed time. Eur Radiol 24:1386–1393. https://doi.org/10.1007/s00330-014-3115-z
Choi AL, Jang KM, Kim MJ, Koh SH, Lee Y, Min K, Choi D (2011) What determines the periportal free air, and ligamentum teres and falciform ligament signs on CT: can these specific air distributions be valuable predictors of gastroduodenal perforation? Eur J Radiol 77:319–324. https://doi.org/10.1016/j.ejrad.2009.07.033
Cho HS, Yoon SE, Park SH, Kim H, Lee YH, Yoon KH (2009) Distinction between upper and lower gastrointestinal perforation: usefulness of the periportal free air sign on computed tomography. Eur J Radiol 69:108–113. https://doi.org/10.1016/j.ejrad.2007.08.024
Stoker J, van Randen A, Laméris W, Boermeester MA (2009) Imaging patients with acute abdominal pain. Radiology 253:31–46. https://doi.org/10.1148/radiol.2531090302
Kim HC, Shin HC, Park SJ, Park SI, Kim HH, Bae WK, Kim IY, Jeong DS (2004) Traumatic bowel perforation: analysis of CT findings according to the perforation site and the elapsed time since accident. Clin Imaging 28:334–339. https://doi.org/10.1016/S0899-7071(03)00244-4
Ishtiaq R, Niaz K, Masood D, Ishtiaq D, Yasin S, Chaudhry UH, Ashraf A (2017) Not a common rectosigmoid perforation. Cureus 13(9):e1465. https://doi.org/10.7759/cureus.1465
Oguro S, Funabiki T, Hosoda K, Inoue Y, Yamane T, Sato M, Kitano M, Jinzaki M (2010) 64-Slice multidetector computed tomography evaluation of gastrointestinal tract perforation site: detectability of direct findings in upper and lower GI tract. Eur Radiol 20:1396–1403. https://doi.org/10.1007/s00330-009-1670-5
Author information
Authors and Affiliations
Contributions
HC, MAK and CA evaluated the CT scans regarding intraabdominal free air distribution. HC, MAK, and MS analyzed the data. HC prepared the original draft. CA and IBA helped in writing and editing. MS supervised the research.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our institutional review board approved this retrospective study. Due to its retrospective nature, informed consent was waived.
Consent for publication
Available upon request.
Competing interests
The authors declare that they have no conflict of interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Celik, H., Kamar, M.A., Altay, C. et al. Accuracy of specific free air distributions in predicting the localization of gastrointestinal perforations. Emerg Radiol 29, 99–105 (2022). https://doi.org/10.1007/s10140-021-01990-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-021-01990-7