Abstract
Background
The purpose of the study was to conduct a comprehensive genomic characterization of gene alterations, microsatellite instability (MSI), and tumor mutational burden (TMB) in submucosal-penetrating (Pen) early gastric cancers (EGCs) with varying prognoses.
Methods
Samples from EGC patients undergoing surgery and with 10-year follow-up data available were collected. Tissue genomic alterations were characterized using Trusight Oncology panel (TSO500). Pathway instability (PI) scores for a selection of 218 GC-related pathways were calculated both for the present case series and EGCs from the TCGA cohort.
Results
Higher age and tumor location in the upper-middle tract are significantly associated with an increased hazard of relapse or death from any cause (p = 0.006 and p = 0.032). Even if not reaching a statistical significance, Pen A tumors more frequently present higher TMB values, higher frequency of MSI-subtypes and an overall increase in PI scores, along with an enrichment in immune pathways. ARID1A gene was observed to be significantly more frequently mutated in Pen A tumors (p = 0.006), as well as in patients with high TMB (p = 0.027). Tumors harboring LRP1B alterations seem to have a higher hazard of relapse or death from any cause (p = 0.089), being mutated mainly in relapsed patients (p = 0.093).
Conclusions
We found that the most aggressive subtype Pen A is characterized by a higher frequency of ARID1A mutations and a higher genetic instability, while LRP1B alterations seem to be related to a lower disease-free survival. Further investigations are needed to provide a rationale for the use of these markers to stratify prognosis in EGC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer (GC) incidence has decreased in Western countries, but this neoplasm is still the fifth solid cancer for frequency and the fourth leading cause of cancer-related death worldwide [1]. Early gastric cancer (EGC), classically defined by the Japanese Cancer Association as a carcinoma limited to the mucosa and/or submucosa regardless of the lymph node status [2], is generally associated with a favorable outcome, with 10-year survival of around 90% [3, 4]. In Europe, the incidence of EGC is much lower than in Asian countries and it represents 10–15% of all GC [5,6,7].
Despite the generally good prognosis, a subgroup of EGC seems to be associated with poor prognosis. In particular, a multicenter GIRCG (Italian Gastric Cancer Research Group) study has demonstrated that the Kodama’s classification could identify a subgroup of EGC patients who have a significantly poorer prognosis according to the type of submucosal invasion [3, 8]. Submucosa-penetrating tumor (Pen) A type, reported to represent around 20% of all EGCs, was, in fact, significantly associated with lower 10-year survival (78.2%) when compared with other submucosal non-Pen A (91.5%) and mucosal (94.2%) EGC. It was also found that Pen A type differed from other EGCs for various clinico-pathological features. As such, the proportion of patients with > 60 years, with tumor size > 2 cm and pN+ status was found to be higher in Pen A types [3]. According to these features and giving its high lymphatic spread, Pen A type EGCs should always be approached with radical gastrectomy plus D2 lymphadenectomy to guarantee the most appropriate oncologic treatment. However, to date, it is difficult to detect a Pen A type before surgical or endoscopic treatment as the type of submucosal involvement could be defined only after resection by the pathologist.
Recent studies tried to characterize EGC at the molecular level, analyzing their expression profiles or genetic alterations, but considering mainly intramucosal tumors, together with premalignant lesions to dissect mechanisms underlying GC cancerogenesis [9,10,11]. Some other studies aimed to find biomarkers of aggressiveness, either focusing on the EGC tumoral component and on the tumor microenvironment [12,13,14,15], but to date the relative contributions of them in the prognostic stratification of EGCs patients warrant further investigation.
Within the same aim, to our knowledge, a wide genomic characterization of gene alterations, microsatellite instability (MSI) status and tumor mutational burden (TMB) of submucosal-penetrating EGCs at different prognosis is still missing and this was the main purpose of our study.
Methods
Study design
This was an observational study conducted at the Istituto Romagnolo per lo Studio dei Tumori “Dino Amadori” on cases with a histological diagnosis of penetrating EGC and surgically treated from 1990 to 2014 by three centers: Morgagni-Pierantoni Hospital of Forlì, University of Verona and University of Siena (Italy). All patients underwent surgery with D2 lymph node dissection. The analyses were performed on patients with adequate tumoral tissue samples and clinico-pathological and follow-up data. Tumors were classified according to Kodama classification [8] in submucosal-penetrating Pen A, referring to EGCs massively invading the submucosa with a nodular pattern and measuring less than 4 cm, and submucosal-penetrating Pen B, which includes EGCs invading the submucosa with a sawtooth pattern and measuring less than 4 cm. The study was conducted in accordance with the Declaration of Helsinki and all participants provided written informed consent.
DNA extraction
The genomic DNA (gDNA) extraction was performed using QIAamp DNA FFPE Tissue Kit (Qiagen, Hilden, Germany) starting from macrodissected formalin-fixed paraffin-embedded (FFPE) slices containing at least 50% of tumoral cells. Manufacturer recommendations were followed for quantitative and qualitative evaluation of DNA quality. The gDNA was quantified with Qubit® dsDNA BR Assay on Qubit 3.0 fluorometer (Invitrogen, Carlsbad, CA) and diluted for the subsequent molecular analyses.
Next-generation sequencing (NGS) analysis
All gDNA samples were characterized for a wide variety of genetic alterations, including single nucleotide variants (SNVs) of 523 genes and copy number variants (CNVs) of 49 gene, as well as MSI and TMB, using Trusight Oncology 500 DNA kit (Illumina) (Supplementary Table 1). Forty ng of gDNA was fragmented using the ME220 ultrasonicator (Covaris). The libraries were prepared and enriched for the 523 genes targeted by the panel following the manufacturer’s instructions. In each run, eight final libraries were pooled and loaded on NextSeq™ 550 sequencer (Illumina). Data were analyzed using the Illumina TSO500 Local app software version 2.0.1.4 (filters: median insert size ≥ 75; percentage of target bases with coverage greater than 100X ≥ 75%). Variants were annotated using ANNOVAR (version 2020-06-08) [16] (filters: i) read depth ≥ 100X; ii) variant allele frequency ≥ 5%; iii) exclusion of non exonic, non splicing and synonymous variants) and Varsome tool (version 11.7.2) [17] to classify them according to ACMG/AMP guidelines [18].
The selected cutoff values were ≥ 10 mut/Mb to define high TMB and > 20% of unstable microsatellites sites to define MSI [19, 20]. The minimum number of usable microsatellite sites to define MSI status was 40. The OncoPrint and Fig. 5a were built with ComplexHeatmap R package [21].
Pathway instability analysis
SNV and CNV data were used to calculate pathway instability (PI) scores for a selection of 218 GC-related pathways in order to estimate their mutagenic disruptions [22] (Supplementary material). The GC-related pathways were selected based on the Reactome pathways enrichment analysis using the list of altered genes across EGC patients [23], using the Reactome Pathway analysis tool [24]. Alterations classified as benign were excluded.
The resultant high-dimensional matrix of PI scores was reduced to two dimensions, using the t-distributed stochastic embedding (t-SNE) dimensionality reduction algorithm [25]. This representation of the PI scores was clustered using the density-based spatial clustering (DBSCAN) method [26]. Both algorithms were applied via the scikit-learn 1.1.3 package [27]. The implementation of the pathway instability analysis can be found at https://doi.org/10.5281/zenodo.10816958.
Statistical analysis
Participant characteristics were summarized by means of descriptive statistics such as mean ± standard deviation (SD) or median, first (IQ) and third (IIIQ) quartile, as well as minimum and maximum values for continuous variables, and frequencies and percentages for categorical ones. Student’s t test or the Mann–Whitney U test and the Chi-square or the Fisher’s exact test, as appropriate, were used to compare baseline characteristics between the Pen A and Pen B groups. The Cox proportional hazard (PH) model was used to investigate the association between baseline covariates and disease-free survival (DFS). The proportional hazards assumption was tested using Schoenfeld residuals. Results were reported as hazard ratios (HRs) and 95% confidence intervals (CIs). DFS was defined as the time since surgery to disease recurrence and death from any cause, whichever occurred first.
For identifying the defining pathways of obtained clusters, the Wilcoxon rank-sum test was used. P values were corrected for multiple testing using the Benjamini/Hochberg procedure, using a cutoff of 0.05 for establishing significance. To test whether unsupervised clustering captures important clinical features, Fisher’s exact test was used to compare the distribution of clinical parameters between the clusters. Lastly, the distribution of PI scores was directly compared across various clinical groupings (TMB class, MSI class, Kodama class and relapse status) using the Wilcoxon rank-sum test.
The analyses were carried out using STATA 15.1 (college station, Texas, USA), R version 4.1.0 statistical software (http://cran.r-project.org/) and Python version 3.8.16 (Python Software Foundation, https://www.python.org/).
Results
Clinico-pathological characteristics and prognosis of EGC patients
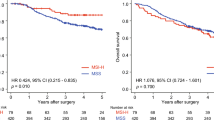
A total of 27 patients were considered in the analyses. Most were females, with a mean age at EGC diagnosis of 67 \(\pm\) 11.7 years. Tumors were mainly classified as intestinal type and did not involve lymph nodes. Among patients, 14 were diagnosed with Pen B (52%) and 13 (48%) with Pen A tumors, according to the Kodama’s classification; 9 (33%) and 7 (26%) patients had a recurrence or death as first event, whereas 11 (67%) patients were disease free/alive within 10 years of follow-up. No statistically significant differences were observed between Pen B and Pen A tumors (Table 1). At univariate analyses using Cox PH model, higher age and tumor location in the upper-middle tract were associated with an increased hazard of relapse or death from any cause (p = 0.006 and p = 0.032, respectively), as shown in the forest plot (Fig. 1). Moreover, patients with higher tumor grade seem to have about a double risk of relapsing or dying, even if the small case series does not permit statistical significance.
Forest plot. Univariate Cox regression analysis for disease-free survival. The following reference categories were used: “female” for gender; “Pen B” for Kodama classification; “antrum” for tumor location; “intestinal” for Lauren classification; “G1+G2” for grade; “N0” for lymph node status; “Absent” for lymphovascular invasion. Age, Tumor size, and lymph node ratio are reported as continuous variables. HR hazard ratio, CI confidence interval, p p-value
Molecular profiling of EGCs
NGS analysis revealed a total of 904 variants. Among them, 200 variants (22.1%) were predicted as pathogenic/likely pathogenic, 372 (41.2%) as variants of uncertain significance (VUS), and 332 (36.7%) as benign/likely benign. Regarding the effect on the protein, 103 variants (11.4%) were frameshift deletions/insertions, 17 (1.9%) in-frame deletions/insertions, 27 (3.0%) nonsense mutations, 721 (79.8%) missense mutations, and 36 (4%) splice site mutations (Fig. 2a). Regarding mutation type, 73.4% were transitions and 26.6% were transversions (Fig. 2b). No significant differences between Pen A and Pen B tumors as well as relapsed and non-relapsed status were observed.
Mutational characterization of EGCs based on DNA sequencing. a For each patient (x-axis, ordered by TMB) relative frequency of variant types is shown for mutations in exonic regions of genes. b Relative frequency of SNV types. c MSI and TMB status of EGC patients. Patients are grouped by Kodama classification and relapse status in all subfigures
TMB and MSI were significantly associated with 100% of MSI high (> 20%) patients showing also a high TMB (≥ 10), Fisher’s exact p = 0.002. Although no statistically significant difference was observed, Pen A presented higher median TMB values compared to Pen B (8 [IQ-IIIQ 4.8 – 25.3] vs 5.2 [IQ-IIIQ 2.4 – 11.1] (p = 0.120)), as well as a higher number of MSI subtype tumor, defined according to the selected cut off (p = 0.165) (Fig. 2c and Supplementary Table S2).
Genomic analysis revealed that the most frequently mutated genes were TP53, protein tyrosine phosphatase receptor type T (PTPRT), E3 ubiquitin ligase ring finger protein 43 (RNF43), F-box and WD repeat domain-containing7 (FBXW7), AT-rich interaction domain 1A (ARID1A) and spectrin alpha, erythrocytic 1 (SPTA1), as shown in Fig. 3. Twenty-two percent of patients presented erb-b2 receptor tyrosine kinase 2 (ERBB2) gene alterations, 5/27 (18%) being ERBB2 amplified. Similarly, cyclin E1 (CCN1E) was amplified in 15% of tumors. Of interest, mutations in ARID1A were found only in Pen A tumors (p = 0.006), 4/6 of them being frameshift substitutions classified as “likely pathogenic”, the remaining 2 classified as variants of uncertain significance (Table 2 and Fig. 4). A significant association between ARID1A alterations and high TMB (p = 0.027) and microsatellite instability (p = 0.056) has been observed. No other statistically significant molecular differences between Pen A and Pen B were observed.
In patients with a high tumor mutational burden, other significantly mutated genes were APC (p = 0.029), and ARID2 (p = 0.029). A significant association was also observed between MSI and ANKRD11 (p = 0.013) and RNF43 mutations (p < 0.0001).
The broad molecular characterization of the EGC series did not reveal any other significant associations with clinico-pathological characteristics, except for TP53 mutations which were more frequently found in intestinal-type EGC and in males (p = 0.041 and p = 0.054) and for the association between the low-density lipoprotein receptor-related protein 1b (LRP1B) mutations and higher age (p = 0.020). Despite not reaching statistical significance, tumors harboring LRP1B alterations seem to have a higher hazard of relapse or death from any cause (HR = 2.73 95% CI: 0.857–8.703 p = 0.089), being mutated mainly in relapsed patients (p = 0.093).
Pathway analysis of EGC
The enrichment analysis revealed no statistically significant associations after correction for multiple testing between a pathway’s PI score and Kodama classification at the detailed level with 218 GC-related pathways. The results of the statistical comparison of individual pathway PI scores across different subgroups of patients (TMB and MSI class, Kodama classification, relapse status) are presented in Supplementary Table S3 (available in our Zenodo repository). Visual representation of the PI score distribution for all 218 pathways is presented in Fig. 5a. Individual pathways can be grouped according to their corresponding Top Level Pathway in the Reactome database hierarchy, representing overarching biological processes critical for the functioning of organisms. Such grouping allows the identification of general patterns in how increased pathway instability potentially disrupts these biological functions for different subgroups of patients. Upon grouping the pathways according to their Top Level Pathways, it becomes apparent that higher PI score in pathways belonging to “Disease” (p < 0.001), “Immune System” (p < 0.001) and “Signal Transduction” (p < 0.001) are associated with Pen A classification (Fig. 5b). Association between overall increased PI score and Pen A classification remained significant when considering all pathways together.
Pathway instability analysis. a Heatmap representation of the 218 GC pathways identified with the Reactome enrichment analysis. Pathways are sorted in columns and grouped according to their corresponding Top Level pathways, with hierarchical clustering applied within the groupings. TMB and MSI class, as well as relapse status and Kodama classification are annotated on the left side for all patients. b, c PI score distribution across b Kodama classification subtypes and c relapse status, shown for pathways grouped according to selected top level pathways. Each data point indicates a PI score value for an individual GC-related pathway, for each patient separately. Violin plots with horizontal black lines marking the median values convey the overall distribution of PI scores between different patient groupings. Note that since no information on Kodama classification was available for EGC-TCGA patients, these patients are excluded from comparisons between Pen A and Pen B groups. d, e Two-dimensional t-SNE representation of PI scores obtained from 218 pathways of interest, for the combined case series of EGC and TCGA EGC. Clustering overlaid with patients’ d Kodama classification and e TMB classification
To explore in more depth the molecular landscape of early gastric cancer using a bigger case series, the publicly available dataset of Stomach Adenocarcinomas (STAD) from TCGA––PanCancer Atlas was retrieved using the cBioPortal (https://www.cbioportal.org/) [28] and was added to the analysis. To match EGC, only stage I gastric cancer patients with survival data available were included (n = 54). The clinico-pathological characteristics of the two cohorts were largely comparable. Notably, the EGC cohort of the present study had a higher percentage of female patients, tumors predominantly located in the lower tract and a greater proportion of pN+ tumors, compared to the TCGA cohort (Supplementary Table S4). Moreover, for the patients belonging to the TCGA cohort, the Kodama classification of the tumor was not available.
PI scores were calculated for the GC-related pathways for a combined cohort of EGC and EGC–TCGA patients (n = 81), but no statistically significant association between a pathway’s PI score and the relapse status was observed for any single pathway after correction for multiple testing. However, top level pathways revealed that relapsed patients had significantly higher PI scores in pathways belonging to “DNA Repair” (p < 0.001) and “Cellular responses to stimuli” (p < 0.001), whereas they had significantly lowered PI scores for “Immune System” (p = 0.03) and “Signal Transduction” (p = 0.024) (Fig. 5c). Interestingly, whereas disruptions to the “Immune System” and “Signal Transduction” Top Level pathways are significantly enriched in Pen A patients, the exact opposite is true for relapsed patients. However, it is important to note that relapse status was known for all EGC-TCGA patients, whereas Kodama classification was not available, which is why EGC-TCGA patients are absent from comparisons involving Pen status. Furthermore, as we do not observe the expected association between Kodama classification and relapse status, this should not come off as a surprise.
Moreover, the analysis of the combined cohort permits the identification of four main clusters of patients (Fig. 5d, e). Clusters 1–3 are characterized by a majority of TMB low patients, whereas the smallest Cluster 4 is made up of exclusively TMB low patients (p = 0.16). Clusters 3 and 4 contain only three patients each with available information on Kodama status, and both feature the same split (2 Pen B vs 1 Pen A). Cluster 1 is characterized by a slight majority (6/11) of Pen B patients, whereas the reverse is true for Cluster 2 with 6/10 patients being Pen A (p = 0.44). There were no statistically significant differences among the clusters in the distribution of the main clinico-pathological parameters or disease-free survival (p = 0.607) (Supplementary Figure S1).
A closer look showed that the clusters were characterized by specific signatures of disrupted pathways. For example, Cluster 4 is differentiated by disruptions in the pathways belonging mainly to signal transduction by tyrosine kinases. Clusters 2 and 3 share some significantly disrupted pathways such as those involved in transcription, intracellular signaling, metabolism of proteins, DNA repair and programmed cell death. The remaining Cluster 1 had no specific significantly disrupted pathways (Supplementary Table S5- available at https://doi.org/10.5281/zenodo.10816958).
Looking at which genes were most frequently mutated for each cluster provides further credence that PI score-based clustering stratifies patients into groups with distinct molecular characteristics. All patients belonging to Cluster 1 have mutations in TP53 (100%). After TP53, most often mutated genes are SPTA1 (22.8%), LRP1B (18.2%) and ARID1A (18.2%), roughly following the overall trend of mutated genes for the cohort. The most frequently mutated gene in Cluster 2 is ARID1A (44.44%), which is the 2nd most commonly mutated gene across all clusters with an overall mutation frequency of about 30%. Significant associations for patients with mutated ARID1A and TMB and MSI status were observed in the combined case series, but no significant association has been found with the relapse status (p = 0.7721). Interestingly, no patients from Cluster 2 have mutated TP53. As for Cluster 1, Cluster 3 is TP53 mutated in all 18 patients (100%), followed by LRP1B (33.33%) and EPHA5 (33.33%). ARID1A (22.22%) and SPTA1 (11.11%), otherwise among the most commonly mutated genes, are notably less mutated in Cluster 3. Lastly, Cluster 4 features a unique mutation signature with the most commonly mutated gene being RHOA (100%), followed by TP53 (20%) and RNF43 (20%) (Supplementary Table S6).
Discussion
In the minimally invasive surgery era, EGC may be more easily treated with D1+ lymphadenectomy or with more conservative endoscopic-assisted hybrid procedures. However, a variable outcome has been observed for patients with submucosa-penetrating EGC. In particular, patients with Pen A type early gastric cancer, which has been shown to be at high risk for lymph node metastases (LNM), should undergo D2 lymphadenectomy to achieve radicality.
Current methods for a pretreatment evaluation of LNM in EGC are insufficient due to suboptimal accuracy [29, 30], which may result in high rate of overtreatment and unnecessary gastrectomies.
Thus, the assessment of prognostic markers should be mandatory in the decision making, to better stratify EGCs and to give the patient the most adequate treatment.
In the present case series of EGC with a 10-year follow-up, neither LNM nor penetrating-subtype A were significantly associated with DFS, whereas patients with higher age and a tumor localization in the upper-middle part of the stomach present a higher risk of relapse or death from any cause. In the last 10 years, several models, based on clinico-radiological parameters, have been proposed as an attempt to predict the curability of the endoscopic treatment [31,32,33]. However, they did not consider in their analysis genomic or molecular data which could have helped in improving the prognostic accuracy of the model.
Several efforts have been made focusing on the biological characteristics which can impact the higher aggressiveness of some EGCs. Chen and collaborators showed the association between the collagen signature in the tumor microenvironment is an independent risk factor for LNM in EGC [12]. Moreover, it has been recently shown that LNM in EGC are related to a specific 3-markers DNA methylation signature, which can have a diagnostic potential to identify more aggressive EGC patients, thus reducing unnecessary gastrectomy in EGC [13].
Recent results revealed that a deep molecular characterization is useful in determining and predicting the malignant potential of EGC. Datta et al. examined the EGCs associated with the worst prognosis, comparing them with those with the best survival, with the aim of revealing a distinct genomic profile in those groups. The authors found that TP53MUT/LOH was associated with those EGC with poor prognosis, in line with what we observed in our previous study, i.e., a prevalence of TP53MUT/LOH type in the most aggressive EGC subtype, Pen A [14].
In the present study, we performed a wide NGS profiling to characterize the molecular landscape of submucosa-penetrating EGC to find if a specific genomic signature is related to a different prognosis.
Consistent with previous studies [34, 35], in our cohort of patients, TP53 was the most frequently altered gene (52%), followed by other tumor suppressor mutated genes, such as FBW7, RNF43 and ARID1A, already identified as biomarkers for early GC carcinogenesis, determinants for the progression of intestinal metaplasia to gastric cancer and worst prognosis [36,37,38]. The approach we adopted in the present study permitted us to evaluate the TP53 entire coding region, but not its LOH. No significant association was observed between TP53 mutations and relapse or Pen subtype.
In line with the enrichment of chromosomal unstable subtypes in TP53 mutated tumors [39], we also observed frequent ERBB2 and CCN1E focal amplifications in this case series, albeit without any association with prognosis.
Among the remaining genes, mutations we found in LRP1B seem especially of interest. LRP1B is a novel candidate tumor suppressor gene, capable of inhibiting tumor cell invasion and metastasis. Its reduced expression and alterations were more commonly found in tumors with a high lymph node ratio [36]. Moreover, LRP1B mutations have been found to be associated with an older age and a low survival rate [40]. This is roughly in line with our observation that LRP1B alterations tend to exhibit higher hazard of relapse or death from any cause even though the statistical tests did not reach significance level (p = 0.089). Being one of the most commonly mutated genes in our dataset overall, LRP1B is mutated at a high rate in three out of four clusters identified in the t-SNE embedding (Supplementary Table S6). Therefore, a potentially increased risk of relapse or death due to LRP1B would likely not be discernible in direct comparison of the clusters. Cluster 4, which does not contain any patients with mutated LRP1B, does at first seemingly display higher DFS in the first 50 months of follow-up compared to other clusters (Supplementary Figure S1). However, this cluster consists of only five patients and consequently has very few events, and the difference is not statistically significant when considering the complete duration of the follow-up.
Another interesting marker we identified in the present study is ARID1A, which is a member of the SW/SNF family and a key component of the adenosine triphosphate-dependent chromatin-remodeling complex. Loss of ARID1A expression is one of most frequent abnormalities associated with histological heterogeneity in GC, with mutation prevalence ranging from 8 to 31% [41], specifically 22% in our case series. Inactivating mutations in the gene, as well as complete or partial loss of ARID1A expression, seem to be an important factor promoting lymph node metastasis after invasion and are associated with poor patient prognosis [42]. Some authors indicate ARID1A’s role as a prognostic biomarker for the identification of high-risk GC patients, especially in early-stage undifferentiated cases [43]. Others found that somatic genomic alterations of ARID1A and other genes, combined with TMB, were associated with the development of metachronous cancers after curative endoscopic submucosal dissection and successful HP eradication in EGC [44]. It has been demonstrated that ARID1A alterations compromise the mismatch repair system; thus ARID1A defects are associated with MSI and high TMB, which can ultimately affect disease-free survival and overall survival of patients with advanced gastric cancer [45]. Interestingly, in our case series of EGC, we observed that ARID1A is mutated only in the most aggressive subtype Pen A. Furthermore, even the statistical significance was not reached, Pen A tumors more frequently present higher TMB values, higher frequency of MSI-subtypes and an overall increase in PI scores. Even if the results of pathways analysis should be interpreted with caution, the grouping of individual pathways according to their Top Level pathway seemingly identifies, among the others, a significant difference in the potential disruption to “Immune System” pathways in Pen A patients compared to Pen B patients. This is in line with the hypothesis that the loss of ARID1A leads to immune resistance, potentially because of the AKT signaling pathway activation, which could be finally related to the observed poor prognosis of ARID1A-negative patients [46]. The link between the loss of ARID1A and MSI and TMB, together with PD-L1 expression, TILs and systemic inflammatory markers [46,47,48] increases its clinical and prognostic relevance as a marker for screening and therapeutic response to targeted therapy and immune checkpoint inhibitors in gastric cancer.
To the best of our knowledge, our study is the largest to investigate the genomic alteration profile, including TMB and MSI status, in EGC patients with a relatively long follow-up. We are aware that the sample size of our cohort was limited, which is why we included publicly available data to parts of our analysis. However, large cohort studies are warranted to confirm our findings and elucidate the mechanisms by which these mutations impact the prognosis of EGC, particularly submucosa-penetrating tumors, with the ultimate goal of finding specific markers, easily determinable also in small diagnostic biopsy samples, which permit to offer the patient the best treatment option.
Conclusions
In summary, the present study revealed the genomic characteristics of a small cohort of Italian EGC patients and suggested that ARID1A might warrant further investigations to provide a rationale for its use as a prognostic marker in EGC patients.
Data availability
Scripts used for the pathways instability analysis and Supplementary Tables 3 and 5 have been deposited in the following public depository https://doi.org/10.5281/zenodo.10816958.
References
Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209–49.
Japanese Gastric Cancer A. Japanese Classification of Gastric Carcinoma - 2nd English Edition. Gastric Cancer 1998;1(1):10–24.
Morgagni P, Solaini L, Saragoni L, et al. An aggressive early gastric cancer: Kodama’s pena type. Eur J Surg Oncol. 2018;44:1186–90.
Suzuki H, Oda I, Abe S, et al. High rate of 5-year survival among patients with early gastric cancer undergoing curative endoscopic submucosal dissection. Gastric Cancer. 2016;19:198–205.
Bollschweiler E, Berlth F, Baltin C, Mönig S, Hölscher AH. Treatment of early gastric cancer in the Western World. World J Gastroenterol. 2014;20:5672–8.
Saragoni L, Morgagni P, Gardini A, et al. Early gastric cancer: diagnosis, staging, and clinical impact. evaluation of 530 patients. new elements for an updated definition and classification. Gastric Cancer. 2013;16(4):549–54.
Satoshi K, Ioannis R, Mats L, Magnus N. Current trends in gastric cancer treatment in Europe. J Cancer Metastasis Treat. 2018;4:35.
Kodama Y, Inokuchi K, Soejima K, Matsusaka T, Okamura T. Growth patterns and prognosis in early gastric carcinoma Superficially spreading and penetrating growth types. Cancer. 1983;51(2):320–6.
Rokutan H, Abe H, Nakamura H, et al. Initial and crucial genetic events in intestinal-type gastric intramucosal neoplasia. J Pathol. 2019;247:494–504.
Zhang P, Yang M, Zhang Y, et al. Dissecting the single-cell transcriptome network underlying gastric premalignant lesions and early gastric cancer. Cell Rep. 2019;27:1934-47.e5.
Zhang Y, Wu X, Zhang C, et al. Dissecting expression profiles of gastric precancerous lesions and early gastric cancer to explore crucial molecules in intestinal-type gastric cancer tumorigenesis. J Pathol. 2020;251:135–46.
Chen D, Chen G, Jiang W, et al. Association of the collagen signature in the tumor microenvironment with lymph node metastasis in early gastric cancer. JAMA Surg. 2019;154: e185249.
Chen S, Yu Y, Li T, et al. A novel DNA methylation signature associated with lymph node metastasis status in early gastric cancer. Clin Epigenet. 2022;14:18.
Datta J, Da Silva EM, Kandoth C, et al. Poor survival after resection of early gastric cancer: extremes of survivorship analysis reveal distinct genomic profile. Br J Surg. 2020;107:14–9.
Molinari C, Tedaldi G, Rebuzzi F, et al. Early gastric cancer: identification of molecular markers able to distinguish submucosa-penetrating lesions with different prognosis. Br J Surg. 2021;24:392–401.
Wang K, Li M, Hakonarson H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 2010;38: e164.
Kopanos C, Tsiolkas V, Kouris A, et al. VarSome: the human genomic variant search engine. Bioinformatics. 2019;35:1978–80.
Richards S, Aziz N, Bale S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of medical genetics and genomics and the Association for molecular pathology. Genet Med. 2015;17:405–24.
Jung J, Heo YJ, Park S. High tumor mutational burden predicts favorable response to anti-PD-(L)1 therapy in patients with solid tumor: a real-world pan-tumor analysis. J Immunother Cancer. 2023;11: e006454.
Wei B, Kang J, Kibukawa M, et al. Evaluation of the trusight oncology 500 assay for routine clinical testing of tumor mutational burden and clinical utility for predicting response to pembrolizumab. J Mol Diagn. 2022;24:600–8.
Gu Z, Eils R, Schlesner M. Complex heatmaps reveal patterns and correlations in multidimensional genomic data. Bioinformatics. 2016;32:2847–9.
Zolotovskaia MA, Sorokin MI, Roumiantsev SA, Borisov NM, Buzdin AA. Pathway instability is an effective new mutation-based type of cancer biomarkers. Front Oncol. 2018;8:658.
Gillespie M, Jassal B, Stephan R, et al. The reactome pathway knowledgebase 2022. Nucleic Acids Res. 2022;50:D687–92.
Fabregat A, Sidiropoulos K, Viteri G, et al. Reactome pathway analysis: a high-performance in-memory approach. BMC Bioinformatics. 2017;18:142.
van der Maaten L, Hinton G. Visualizing data using t-SNE. J Mach Learn Res. 2008;9:2579–605.
Ester M., Kriegel H.P., Sander J., Xu X. A Density-Based Algorithm for Discovering Clusters in Large Spatial Databases with Noise. KDD-96 Proceedings. 1996:226–31.
Pedregosa F, Varoquaux G, Gramfort A, et al. Scikit-learn: machine learning in python. J Mach Learn Res. 2011;12:2825–30.
Cerami E, Gao J, Dogrusoz U, et al. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2:401–4.
Lee SL, Lee HH, Ku YM, Jeon HM. Usefulness of two-dimensional values measured using preoperative multidetector computed tomography in predicting lymph node metastasis of gastric cancer. Ann Surg Oncol. 2015;22(Suppl 3):S786–93.
You JM, Kim TU, Kim S, et al. Preoperative N stage evaluation in advanced gastric cancer patients using multidetector CT: can the sum of the diameters of metastatic LNs be used for N stage evaluation? Clin Radiol. 2019;74:782–9.
Embaye KS, Zhang C, Ghebrehiwet MA, et al. Clinico-pathologic determinants of non-e-curative outcome following en-bloc endoscopic submucosal dissection in patients with early gastric neoplasia. BMC Cancer. 2021;21:92.
Lin JX, Wang ZK, Wang W, et al. Risk factors of lymph node metastasis or lymphovascular invasion for early gastric cancer: a practical and effective predictive model based on international multicenter data. BMC Cancer. 2019;19:1048.
Sekiguchi M, Oda I, Taniguchi H, et al. Risk stratification and predictive risk-scoring model for lymph node metastasis in early gastric cancer. J Gastroenterol. 2016;51:961–70.
Cancer Genome Atlas Research Network. Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202–9.
Cristescu R, Lee J, Nebozhyn M, et al. Molecular analysis of gastric cancer identifies subtypes associated with distinct clinical outcomes. Nat Med. 2015;21:449–56.
Holm B, Barsuhn S, Behrens HM, Krüger S, Röcken C. The tumor biological significance of RNF43 and LRP1B in gastric cancer is complex and context-dependent. Sci Rep. 2023;13:3191.
Huang KK, Ma H, Chong RHH, et al. Spatiotemporal genomic profiling of intestinal metaplasia reveals clonal dynamics of gastric cancer progression. Cancer Cell. 2023;41:2019-37.e8.
Huang KK, Ramnarayanan K, Zhu F, et al. Genomic and epigenomic profiling of high-risk intestinal metaplasia reveals molecular determinants of progression to gastric cancer. Cancers (Basel). 2018;33:137-50.e5.
Sahgal P, Huffman BM, Patil DT, et al. Early TP53 alterations shape gastric and esophageal cancer development. Cancers (Basel). 2021;13:5915.
Wang H, Ding Y, Chen Y, et al. A novel genomic classification system of gastric cancer via integrating multidimensional genomic characteristics. Gastric Cancer. 2021;24:1227–41.
Xu S, Tang C. The role of ARID1A in tumors: tumor initiation or tumor suppression? Gastric Cancer. 2021;11: 745187.
Kim SM, Min BH, Ahn JH, et al. Nomogram to predict lymph node metastasis in patients with early gastric cancer: a useful clinical tool to reduce gastrectomy after endoscopic resection. BMC Cancer. 2020;52:435–43.
Ashizawa M, Saito M, Min AKT, et al. Prognostic role of ARID1A negative expression in gastric cancer. Sci Rep. 2019;9:6769.
Sakuta K, Sasaki Y, Abe Y, et al. Somatic alterations and mutational burden are potential predictive factors for metachronous development of early gastric cancer. Sci Rep. 2020;10:22071.
Zhang N, Li P, Wu X, Xia S, Zhao X, Chen L. Analysis of threshold changes of tumor mutation burden of gastric cancer and its relationship with patients’ prognosis. J Oncol. 2021;2021:1–5.
Zhang Z, Li Q, Sun S, et al. Prognostic and immune infiltration significance of ARID1A in TCGA molecular subtypes of gastric adenocarcinoma. Cancer Med. 2023;12:16716–33.
Lu S, Duan R, Cong L, Song Y. The effects of ARID1A mutation in gastric cancer and its significance for treatment. J Cancer Res Clin Oncol. 2023;23:296.
Wang X, Che K, Shi T, et al. Loss of ARID1A expression is associated with systemic inflammation markers and has important prognostic significance in gastric cancer. J Cancer Res Clin Oncol. 2022;148:1583–95.
Acknowledgements
DP and ER acknowledge support by the Sächsische Staatsministerium für Wissenschaft, Kultur und Tourismus (SMWK) under the frame of ERA PerMed (GRAMMY, 2019-275). JE acknowledges the financial support by the Federal Ministry of Education and Research of Germany and by SMWK in the Programme Center of Excellence for AI-research, Center for Scalable Data Analytics and Artificial Intelligence Dresden/Leipzig“, project identification number: ScaDS.AI.
Funding
Open access funding provided by Alma Mater Studiorum - Università di Bologna within the CRUI-CARE Agreement. The study was partially supported by the Gruppo Italiano Ricerca Cancro Gastrico (GIRCG) and by the Italian Ministry of Health within the ERAPerMed Project GRAMMY (ERP-2019–23671108; GRAMMY, 2019–275).
Author information
Authors and Affiliations
Contributions
CM, LSo, PM, GM, PU, and LSa conceived the idea and designed the study; CM, GT, FR, and MC were responsible for data acquisition and interpretation; EP performed the statistical analysis; DA, DP, JE, and ER performed the bioinformatic analysis and interpretation; PM, MB, AT, DM, MRA, GE, LSo, and LSa collected samples and interpreted the clinical patient data; AT, MRA, and LSa performed the histo-pathological examination of the tissue specimens; CM, FR, and PU were major contributors in writing the manuscript; PM, GM, DP, JE, ER, and LSa critically revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The protocol was reviewed and approved by the Local Ethics Committee C.E.ROM. (protocol number: IRSTB044).
Informed consent
Written informed consent (or substitutive declaration for the deceased subjects) was obtained for all patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Molinari, C., Solaini, L., Rebuzzi, F. et al. Genomic events stratifying prognosis of early gastric cancer. Gastric Cancer (2024). https://doi.org/10.1007/s10120-024-01536-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10120-024-01536-z