Abstract
Background
The results of prospective studies examining the association between dietary vitamin A intake and the risk of gastric cancer have often been conflicting. The objective of this study was to investigate this issue in a general Japanese population.
Methods
A total of 2,467 community-dwelling Japanese subjects aged 40 years or older were followed up prospectively for 14 years. Dietary vitamin A intake was estimated using a semiquantitative food frequency method.
Results
During the follow-up period, gastric cancer developed in 93 subjects. The age- and sex-adjusted incidence of gastric cancer rose progressively with increasing levels of dietary vitamin A intake: at 2.2, 3.0, 3.8, and 4.5 per 1,000 person-years for quartile groups defined by dietary vitamin A intake levels of <639, 639–837, 838–1,061, and >1,061 μg retinol equivalents (RE)/day, respectively (P for trend <0.01). The risk of gastric cancer was significantly higher in the fourth quartile than in the first one even after multivariate adjustment [hazard ratio (HR) = 1.47, 95% confidence interval (CI) = 0.70–3.09, P = 0.30 for the second quartile; HR = 1.85, 95% CI = 0.82–4.18, P = 0.14 for the third quartile; HR = 2.96, 95% CI = 1.12–7.80, P = 0.03 for the fourth quartile]. Comparable effects of vitamin A intake were observed irrespective of the location or histological type of gastric cancer. The HR for gastric cancer increased significantly only in subjects with a combination of high vitamin A intake (>1,061 μg RE/day) and Helicobacter pylori infection.
Conclusions
Our findings suggest that dietary vitamin A intake is clearly associated with the risk of gastric cancer in the general Japanese population.
Similar content being viewed by others
Introduction
Although the morbidity and mortality of gastric cancer have declined markedly worldwide over the latter half of the last century, gastric cancer is still the fourth most common malignancy and the second leading cause of cancer death [1, 2]. Because the incidence of gastric cancer varies markedly among various regions and from one generation to the next, it is thought that the risk of gastric cancer is determined largely by environmental factors, including dietary factors and infection with Helicobacter pylori [3–5]. However, the specific dietary components involved in the development of gastric cancer remain unclear.
Vitamin A is a generic term referring to both preformed vitamin A (retinol and its esters) and some carotenoids [6]. Vitamin A is needed for scotopic and color vision in the retina of the eye [7]. Vitamin A also functions as an irreversibly oxidized form of retinoic acid, which is an important hormone-like growth factor for epithelial and other cells [8]. Some epidemiological studies have indicated that the dietary intake of vitamin A has preventive effects on malignant neoplasms [9–12]. However, in two intervention trials, the supplementary intake of retinol and β-carotene, or β-carotene only, increased the incidence of lung cancer [13, 14]. Furthermore, the findings from prospective studies of the dietary intake of vitamin A in relation to gastric cancer risk have been quite inconsistent [15–20]. Some cohort studies have found a negative association between dietary intake of vitamin A and the risk of gastric cancer [15, 16], whereas others have found no apparent association [17–19] or have even found a positive association [20]. This conflicting background underscores the need for a thorough investigation of the role of vitamin A in the development of gastric cancer. In the present study, we prospectively investigated the association between dietary vitamin A intake and the incidence of gastric cancer in a general Japanese population.
Subjects, materials, and methods
Study population
The town of Hisayama, in which an epidemiological study of cardiovascular disease and malignancy has been ongoing since 1961, is located in a suburban area adjacent to Fukuoka City, a large urban center on Kyushu Island in the southern part of Japan. The population of the town is approximately 8,000 and has been stable for the past 50 years. According to the 1985 census, the age and occupational distributions of the Hisayama population are almost identical to those of the Japanese population as a whole [21]. The dietary patterns of the residents are also similar to those of the Japanese population [22].
In 1988, a total of 2,742 Hisayama residents aged 40 years or older (80.9% of the total population in that age group) underwent a comprehensive health check-up. After the exclusion of 132 subjects with a history of gastrectomy or gastric cancer, 5 subjects who died during the examination period, and 138 who did not undergo a dietary survey, a total of 2,467 subjects (1,023 men and 1,444 women) were enrolled in the study.
The study protocol was approved by the Human Ethics Review Committee of Kyushu University Graduate School of Medical Sciences, and written informed consent for medical research was obtained from the study subjects.
Follow-up survey
The precise method of follow-up used in this study has been described previously [23, 24]. In brief, the study population was followed up for 14 years, from December 1988 to November 2002, by repeated health check-ups that were conducted every year. Approximately 60% of the subjects regularly returned for the check-ups. For all those who did not undergo regular check-ups and those who had moved out of the town, health status was checked every year by mail or by telephone. In addition, a daily monitoring system was established by the study team and local physicians, as well as members of the Division of Health and Welfare of the town. To identify new occurrences of gastric cancer in the cohort, members of our study group surveyed 3 local clinics and 6 hospitals in and around the town, and monitored records of barium meal examinations, upper endoscopic examinations, and biopsy diagnoses. We also checked all reports from the annual mass screenings for gastric cancer with upper gastrointestinal series that were performed by the Division of Health and Welfare of the town. To further search for concealed cases of gastric cancer, autopsies were performed on 361 (75.4%) of the 479 subjects who died during the follow-up period.
The diagnosis of gastric cancer in all cases was confirmed by the histological examination of specimens obtained by gastrectomy, endoscopic mucosal resection, endoscopic submucosal dissection, or autopsy. The location of the tumor within the stomach was determined by the evaluation of both the clinical and histopathological records. The tumors were categorized as either intestinal-type or diffuse-type, according to the classification described by Lauren [25].
During the follow-up period, only one subject was lost to follow-up, and gastric cancer developed in 93 subjects (67 men and 26 women), including 3 concealed cancers (3.2%) first diagnosed at autopsy. Among these cases, there were 8 subjects (8.6%) who had 2 synchronous gastric cancers (double cancers), resulting in 101 cancer lesions.
Nutritional survey
The dietary survey was conducted using a semiquantitative food frequency method validated in a prior study [22, 26]. A self-administered questionnaire concerning food intake over the past year, which consisted of 70 food items, was completed by each participant prior to the initiation of the study, and was checked by experienced dietitians and nutritionists, who presented the subjects with food models of actual size in the survey. The average food intake per day was estimated based on detailed descriptions of the frequency of eating and the quantity of each food. Nutritional intake, including vitamin A intake, was calculated using the 4th revision of the Standard Tables of Food Composition in Japan [27]. The intake of nutritional elements was adjusted for energy intake, using the method of Willett and Stampfer [28], in order to assess independent contributions. In the previous validation study of this semiquantitative food frequency method with a 3-day weighed food record, the correlation coefficients of dietary factors used in this study were as follows: 0.282 for vitamin A, 0.866 for total energy, 0.524 for total fat, 0.318 for salt, 0.738 for vitamin B1, 0.579 for vitamin B2, 0.345 for vitamin C, and 0.274 for fiber [22]. Participants were divided into four groups according to the quartiles of dietary vitamin A intake [<639, 639–837, 838–1,061, and >1,061 μg retinol equivalents (RE)/day].
Risk factor measurement
Serum IgG antibodies to H. pylori were measured by means of a quantitative enzyme immunoassay, using a commercial kit (HM-CAP; Enteric Products, Westbury, NY, USA). The assay values were interpreted as positive and negative based on the manufacturer’s instructions. Diabetes was defined by medical history, glucose levels (fasting glucose level ≥7.0 mmol/l or postprandial glucose level ≥11.1 mmol/l), or a 75-g oral glucose tolerance test (1998 World Health Organization criteria), which was administered to most of the subjects aged 40–79 years, with plasma glucose measured by the glucose-oxidase method. The serum cholesterol level was determined enzymatically. Body mass index (kg/m2) was used as an indicator of obesity.
Information regarding smoking habit, alcohol intake, and regular exercise was obtained using a questionnaire administered to each subject. Smoking habit and alcohol intake were categorized as current or not. Those subjects engaging in sports more than 3 times a week, during their leisure time, were classified as belonging to the regular exercise group.
Statistical analysis
The SAS software package version 9.2 (SAS Institute, Cary, NC, USA) was used to perform all statistical analyses. The mean values of possible risk factors were adjusted for age and sex using the covariance method and were tested for trends across dietary vitamin A intake levels by multiple regression analysis. The frequencies of risk factors were adjusted for age and sex by a direct method and were tested for trends using the Cochran–Mantel–Haenszel test. The incidence of first-ever gastric cancer was estimated by the person-year method, adjusted for age and sex using the direct method, and compared by the Cox proportional hazards model. All the study subjects were regarded as a standard population for age- and sex-adjustment. Age- and sex-adjusted and multivariate-adjusted hazard ratios (HRs) and their 95% confidence intervals (CIs) were also estimated using the Cox proportional hazards model. In the multivariate analysis, the possible risk factors for gastric cancer for which we had data in our cohort; namely, age, sex, H. pylori infection, body mass index, diabetes, serum total cholesterol, smoking habit, alcohol intake, regular exercise, and dietary factors (intake of total energy, total fat, salt, vitamin B1, vitamin B2, vitamin C, and dietary fiber), were included in the model all at once. All tests were 2-sided, and a P value of <0.05 was considered to be statistically significant.
Results
Age- and sex-adjusted baseline characteristics according to quartiles of dietary vitamin A intake levels are shown in Table 1. The mean values for age, body mass index, and total cholesterol levels, as well as the frequency of regular exercise, showed a significant positive association with dietary intake of vitamin A, while the proportion of men was decreased at the higher vitamin A intake levels. Among relevant dietary factors, the mean values for total energy, total fat, salt, vitamin B1, vitamin B2, vitamin C, and dietary fiber intakes showed positive relationships with vitamin A intake levels.
Figure 1 shows the age- and sex-adjusted incidence of gastric cancer according to quartiles of dietary vitamin A intake. The incidence of gastric cancer rose significantly with increasing quartile levels of vitamin A intake (P for trend = 0.01).
Table 2 presents the adjusted HRs for the development of gastric cancer according to quartiles of dietary vitamin A intake. The age- and sex-adjusted HR was significantly higher in the fourth quartile than in the first one. This association remained significant even after adjustment for age, sex, H. pylori infection, body mass index, diabetes, serum total cholesterol, smoking habit, alcohol intake, regular exercise, and dietary factors (intake of total energy, total fat, salt, vitamin B1, vitamin B2, vitamin C, and dietary fiber) (HR 2.96, 95% CI 1.12–7.80, P = 0.03). We also estimated the age- and sex-adjusted HRs for the development of gastric cancer according to quartiles of dietary carotenoid and retinol intake. However, the risk of incident gastric cancer did not significantly change in relation to either carotenoid or retinol intake levels.
Table 3 shows the multivariate-adjusted HRs of high dietary vitamin A intake (the fourth quartile >1,061 μg RE/day) for the development of gastric cancer according to cancer location and histology. The effects of dietary vitamin A intake on the risk of gastric cancer were comparable between locations in the proximal one-third and the distal two-thirds of the stomach (P value for heterogeneity = 0.56). Likewise, there were no significant differences in the effects of dietary vitamin A intake on the risk of gastric cancer between intestinal-type and diffuse-type (P value for heterogeneity = 0.33).
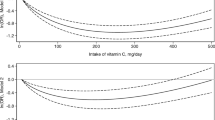
To clarify the combined effect of elevated dietary vitamin A intake and H. pylori infection on the occurrence of gastric cancer, we estimated the multivariate-adjusted HRs of gastric cancer in 4 groups—i.e., a group with high (>1,061 μg RE/day) and a group with low (≤1,061 μg RE/day) dietary vitamin A intake, each subdivided according to the presence or absence of H. pylori infection (Fig. 2). Compared with the reference group, which had neither a high dietary vitamin A intake level nor H. pylori infection, the multivariate-adjusted HRs of gastric cancer for the groups with high dietary vitamin A intake levels alone and H. pylori infection alone were not significant, but the HR for the group having both a high dietary vitamin A intake level and H. pylori infection was significantly high (HR 3.41, 95% CI 1.42–8.19, P < 0.01).The risk of future gastric cancer was also significantly higher in subjects with both an elevated dietary vitamin A intake and H. pylori infection than in those with H. pylori infection alone (HR 2.00, 95% CI 1.08–3.70, P = 0.03). There was no significant interaction between vitamin A intake and H. pylori for gastric cancer risk (P for interaction = 0.27).
Multivariate-adjusted hazard ratios and 95% confidence intervals for gastric cancer risk according to dietary vitamin A intake levels and Helicobacter pylori status at baseline. †Low dietary vitamin A intake was defined as the first, second, and third quartiles (≤1,061 μg RE/day), and high dietary vitamin A intake was defined as the fourth quartile (>1,061 μg RE/day). ‡Hazard ratios were adjusted for age, sex, body mass index, diabetes, serum total cholesterol, smoking habit, alcohol intake, regular exercise, and dietary factors (intake of total energy, total fat, salt, vitamin B1, vitamin B2, vitamin C, and dietary fiber) using the Cox proportional hazards model. *P < 0.01 versus low dietary vitamin A intake and Helicobacter pylori-negative. **P = 0.03 versus low dietary vitamin A intake and Helicobacter pylori-positive
Discussion
The present analysis demonstrated a clear positive association between dietary vitamin A intake and the incidence of gastric cancer in a general Japanese population. This association remained significant even after adjustment for age, sex, H. pylori infection, body mass index, diabetes, serum total cholesterol, smoking habit, alcohol intake, regular exercise, and dietary factors (intake of total energy, total fat, salt, vitamin B1, vitamin B2, vitamin C, and dietary fiber). The association was enhanced by H. pylori infection. Furthermore, a comparable effect of dietary vitamin A intake was observed irrespective of the location or histological type of gastric cancer.
In most but not all case–control studies, dietary vitamin A intake has been negatively associated with the risk of gastric cancer [29–31]. However, the findings of prospective studies on this issue are quite inconsistent [15–20]. A prospective cohort study in Sweden and the Alpha-Tocopherol, Beta-Carotene Cancer Prevention study documented an inverse association between dietary intake of vitamin A and gastric cancer risk [15, 16], but the Iowa Women’s Health Study, the European Prospective Investigation into Cancer and Nutrition, and a case-cohort study in Hawaiian men of Japanese ancestry showed no clear associations between dietary vitamin A intake and gastric cancer risk [17–19]. On the other hand, The Netherlands Cohort Study demonstrated a clearly positive association between dietary retinol intake and the future risk of gastric cancer [20]. In the present study, dietary vitamin A was significantly associated with incident gastric cancer, but such an association was not observed for dietary retinol or carotenoids alone. This finding suggests that combined dietary retinol and carotenoids may act as a risk factor for gastric cancer. Further epidemiological studies are needed to elucidate the influence of the dietary intake of vitamin A on the development of gastric cancer.
A weak point of previous cohort studies [15–17, 19, 20], with a single exception [18], is that H. pylori infection, which is the most powerful risk factor for gastric cancer, was not examined. In our study, the prevalence of H. pylori infection was high (more than 70%), and the association between high vitamin A intake levels and the development of gastric cancer was significant only in subjects with H. pylori infection, but not in those without it. It is not clearly understood why the findings in regard to the association between dietary intake of vitamin A and gastric cancer risk differ among studies, but one possible explanation may be that the prevalence of H. pylori infection differs among people of different ethnicities. High dietary intake of vitamin A may be a significant risk factor for the development of gastric cancer only in populations that have a high prevalence of H. pylori infection, such as the Japanese [32].
In our stratified analyses according to cancer location and histological type, the influence of dietary vitamin A intake was not different between the patients with proximal gastric cancer and those with distal gastric cancer, though there were no significant associations in each stratified category, probably due to the small number of cancer cases. The influence of dietary vitamin A intake was comparable in patients with intestinal-type and those with diffuse-type cancer. These results suggest that dietary vitamin A intake is a common risk factor for gastric cancer irrespective of the location or the histological type of cancer.
The mechanism underlying the association between dietary vitamin A intake and gastric cancer has not been completely resolved. Several experimental studies have shown that a type of vitamin A, retinoic acid, leads to the inhibition of cell growth [33, 34], which may lead to prevention of carcinogenesis. However, a recent study has reported an opposite function of retinoic acid—i.e., retinoic acid may promote neoplastic cell proliferation by activating an orphan nuclear receptor (peroxisome proliferator activated receptor β/δ) [35]. In addition, the autoxidation of retinoids generates H2O2, which plays a role in DNA damage in the presence of endogenous metals [36]. Thus, it is possible that higher dietary vitamin A intake promotes mucosal damage in the stomach. On the other hand, infection with H. pylori also induces DNA damage in gastric mucosal cells, through oxidative stress [37–39]. Thus, high dietary vitamin A intake and infection with H. pylori may have synergistic effects on malignant alterations in the gastric mucosa, though oxidative stress.
The strengths of our study include its longitudinal population-based survey, low selection bias, perfect follow-up of subjects, accuracy of diagnosis of gastric cancer, and comprehensive assessment with risk factors including H. pylori infection. These study characteristics have provided us with an opportunity to precisely examine the influence of dietary vitamin A intake on the development of gastric cancer. However, some limitations of the present study bear mention. First, in this study, the population size was relatively small, which was likely to lead to increased random errors in our results. Nonetheless, we believe that the association between dietary vitamin A intake and the incidence of gastric cancer was robust, because we perfectly followed up all participants and accurately diagnosed gastric cancer. Second, the information regarding nutrient intake, including dietary vitamin A intake, was derived from a semiquantitative food frequency questionnaire that requested information from subjects regarding their average intake over the previous year. The limitations of this method are well known, and random measurement errors are more likely to have contributed to a bias toward finding no effect. Thus, the estimates of effect that we have reported here are most likely conservative. Third, a lack of information on the intake of dietary supplements may have caused some misclassification of nutrient intake. However, dietary supplements were rarely used in 1988 in our country, and such a misclassification would tend to underestimate the effects of dietary vitamin A intake. This suggests that such a bias did not invalidate the present findings. Fourth, subjects with latent gastric cancer at baseline were not completely excluded from the present analysis. However, similar associations were observed between dietary vitamin A intake and gastric cancer even after excluding subjects who developed gastric cancer during the first 2 years of the follow-up period (data not shown). Thus, this limitation does not seem to negate our findings.
In conclusion, the present population-based prospective study demonstrated that a high dietary intake of vitamin A was associated with the future risk of gastric cancer in a general population of Japanese and was a possible cofactor increasing the risk of gastric cancer posed by H. pylori infection. Our findings suggest the possibility that reduction of dietary vitamin A intake as well as the eradication of H. pylori may confer protection against gastric cancer and could be an effective strategy for reducing the burden of gastric cancer in Japan. However, the mechanism underlying the association between dietary intake of vitamin A and the risk of gastric cancer is poorly understood. Further studies will be needed to resolve this issue.
References
Howson CP, Hiyama T, Wynder EL. The decline in gastric cancer: epidemiology of an unplanned triumph. Epidemiol Rev. 1986;8:1–27.
Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108.
Haenszel W, Kurihara M. Studies of Japanese migrants. I. Mortality from cancer and other diseases among Japanese in the United States. J Natl Cancer Inst. 1968;40:43–68.
Curado MP, Edwards B, Shin HR, Storm H. Cancer incidence in five continents. vol. 9. IARC scientific publication no.160. Lyon: International Agency for Research on Cancer, 2008.
Nomura A, Stemmermann GN, Chyou PH, Kato I, Perez–Perez GI, Blaser MJ. Helicobacter pylori infection and gastric carcinoma among Japanese Americans in Hawaii. N Engl J Med. 1991;325:1132–6.
IARC Working Group on the Evaluation of Cancer-Preventive Agents. IARC handbooks of cancer prevention. Vitamin A. vol. 3. Lyon: International Agency for Research on Cancer; 1998.
Krinsky NI, Johnson EJ. Carotenoid actions and their relation to health and disease. Mol Aspects Med. 2005;26:459–516.
Bedo G, Santisteban P, Aranda A. Retinoic acid regulates growth hormone gene expression. Nature. 1989;339:231–4.
Peto R, Doll R, Buckley JD, Sporn MB. Can dietary beta-carotene materially reduce human cancer rates? Nature. 1981;290:201–8.
Willett WC, MacMahon B. Diet and cancer—an overview. N Engl J Med. 1984;310:633–8.
Burton GW, Ingold KU. β-carotene: an unusual type of lipid antioxidant. Science. 1984;224:569–73.
Gonzalez CA. Nutrition and cancer: the current epidemiological evidence. Br J Nutr. 2006;96:S42–5.
The Alpha-Tocopherol, Beta Carotene Cancer Prevention Study Group. The effect of vitamin E and beta carotene on the incidence of lung cancer and other cancers in male smokers. N Engl J Med. 1994;15:1029–35.
Omenn GS, Goodman GE, Thornquist MD, Balmes J, Cullen MR, Glass A, et al. Effect of a combination of beta carotene and vitamin A on lung cancer and cardiovascular disease. N Engl J Med. 1996;334:1150–5.
Larsson SC, Bergkvist L, Näslund I, Rutegård J, Wolk A. Vitamin A, retinol, and carotenoids and the risk of gastric cancer: a prospective cohort study. Am J Clin Nutr. 2007;85:497–503.
Nouraie M, Pietinen P, Kamangar F, Dawsey SM, Abnet CC, Albanes D, et al. Fruits, vegetables, and antioxidants and risk of gastric cancer among male smokers. Cancer Epidemiol Biomarkers Prev. 2005;14:2087–92.
Zheng W, Sellers TA, Doyle TJ, Kushi LH, Potter JD, Folsom AR. Retinol, antioxidant vitamins, and cancers of the upper digestive tract in a prospective cohort study of postmenopausal women. Am J Epidemiol. 1995;142:955–60.
Jenab M, Riboli E, Ferrari P, Friesen M, Sabate J, Norat T, et al. Plasma and dietary carotenoid, retinol and tocopherol levels and the risk of gastric adenocarcinomas in the European prospective investigation into cancer and nutrition. Br J Cancer. 2006;95:406–15.
Chyou PH, Nomura AM, Hankin JH, Stemmermann GN. A case-cohort study of diet and stomach cancer. Cancer Res. 1990;50:7501–4.
Botterweck AA, van den Brandt PA, Goldbohm RA. Vitamins, carotenoids, dietary fiber, and the risk of gastric carcinoma: results from a prospective study after 6.3 years of follow-up. Cancer. 2000;88:737–48.
Ohmura T, Ueda K, Kiyohara Y, Kato I, Iwamoto H, Nakayama K, et al. Prevalence of type 2 (non-insulin-dependent) diabetes mellitus and impaired glucose tolerance in the Japanese general population: the Hisayama study. Diabetologia. 1993;36:1198–203.
Shirota T, Yoshizumi E. Accuracy of nutritional survey using the simple method. Jpn J Public Health. 1990;37:100–8. (in Japanese).
Yamagata H, Kiyohara Y, Aoyagi K, Kato I, Iwamoto H, Nakayama K, et al. Impact of Helicobacter pylori infection on gastric cancer incidence in a general Japanese population: the Hisayama Study. Arch Intern Med. 2000;160:1962–8.
Ikeda F, Doi Y, Yonemoto K, Ninomiya T, Kubo M, Shikata K, et al. Hyperglycemia increases risk of gastric cancer posed by Helicobacter pylori infection: a population-based cohort study. Gastroenterology. 2009;136:1234–41.
Lauren P. The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histoclinical classification. Acta Pathol Microbiol Scand. 1965;64:31–49.
Kiyohara Y, Shinohara A, Kato I, Shirota T, Kubo M, Tanizaki Y, et al. Dietary factors and development of impaired glucose tolerance and diabetes in a general Japanese population: the Hisayama Study. J Epidemiol. 2003;13:251–8.
Resources Council of Science and Technology Agency. Standard tables of food composition in Japan. 4th ed. Tokyo: Ministry of Finance Printing Bureau; 1982. (in Japanese).
Willett W, Stampfer MJ. Total energy intake: implications for epidemiologic analyses. Am J Epidemiol. 1986;124:17–27.
Ekström AM, Serafini M, Nyrén O, Hansson LE, Ye W, Wolk A. Dietary antioxidant intake and the risk of cardia cancer and noncardia cancer of the intestinal and diffuse types: a population-based case–control study in Sweden. Int J Cancer. 2000;87:133–40.
Mayne ST, Risch HA, Dubrow R, Chow WH, Gammon MD, Vaughan TL, et al. Nutrient intake and risk of subtypes of esophageal and gastric cancer. Cancer Epidemiol Biomarkers Prev. 2001;10:1055–62.
Nomura AM, Hankin JH, Kolonel LN, Wilkens LR, Goodman MT, Stemmermann GN. Case-control study of diet and other risk factors for gastric cancer in Hawaii (United States). Cancer Causes Control. 2003;14:547–58.
The EUROGAST Study Group. An international association between Helicobacter pylori infection and gastric cancer. Lancet. 1993;341:1359–62.
Altucci L, Rossin A, Raffelsberger W, Reitmair A, Chomienne C, Gronemeyer H. Retinoic acid-induced apoptosis in leukemia cells is mediated by paracrine action of tumor-selective death ligand TRAIL. Nat Med. 2001;7:680–6.
Soprano DR, Qin P, Soprano KJ. Retinoic acid receptors and cancers. Annu Rev Nutr. 2004;24:201–21.
Schug TT, Berry DC, Shaw NS, Travis SN, Noy N. Opposing effects of retinoic acid on cell growth result from alternate activation of two different nuclear receptors. Cell. 2007;129:723–33.
Murata M, Kawanishi S. Oxidative DNA damage by vitamin A and its derivative via superoxide generation. J Biol Chem. 2000;275:2003–8.
Ding SZ, O’Hara AM, Denning TL, Dirden-Kramer B, Mifflin RC, Reyes VE, et al. Helicobacter pylori and H2O2 increase AP endonuclease-1/redox factor-1 expression in human gastric epithelial cells. Gastroenterology. 2004;127:845–58.
Hahm KB, Lee KJ, Kim JH, Cho SW, Chung MH. Helicobacter pylori infection, oxidative DNA damage, gastric carcinogenesis, and reversibility by rebamipide. Dig Dis Sci. 1998;43(Suppl 9):S72–7.
Emst P. Review article: the role of inflammation in the pathogenesis of gastric cancer. Aliment Pharmacol Ther. 1999;13(Suppl 1):S13–8.
Acknowledgments
This work was supported in part by Grants-in-Aid for Scientific Research A (No.18209024) and C (No. 20591063) from the Ministry of Education, Culture, Sports, Science and Technology of Japan and a Health and Labour Sciences Research Grant of the Ministry of Health, Labour and Welfare of Japan (comprehensive research on aging and health: H20-Chouju-004). The authors thank the residents of the town of Hisayama for their participation in the survey and the staff of the Division of Health and Welfare of Hisayama for their cooperation with this study.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miyazaki, M., Doi, Y., Ikeda, F. et al. Dietary vitamin A intake and incidence of gastric cancer in a general Japanese population: the Hisayama Study. Gastric Cancer 15, 162–169 (2012). https://doi.org/10.1007/s10120-011-0092-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-011-0092-7