Abstract
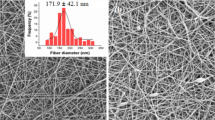
Owing to the significant importance in clinics, antibacterial activity is thought as one indispensable feature of the next generation of absorbable sutures. It is challenging but imperative to arm the existing absorbable sutures with antibacterial functions. The present study describes a “gradient deposition” technique to coat a continuous and smooth layer of chitosan on the surface of absorbable sutures. Specifically, chitosan solution is arranged to undergo gradient pH decline step by step while during each pH interval, the solution is allowed to stand for a predetermined period of time in order to control gradual chitosan deposition. Chitosan nanoparticles are found to be first generated on suture surface and finally developed into a smooth chitosan layer as the antibacterial surface. In vitro and in vivo results demonstrated that coating chitosan on sutures by our technique could relieve wound inflammation, stimulate collagen deposition, regenerate blood vessels, and assist tissue repairing, consequently leading to a significant enhancement of wound healing effect. This technique is highlighted with low cost, extreme convenience and excellent safety without organic solvents. Furthermore, the “gradient deposition” technique would not affect the fundamental properties of matrix and thus hold promises as a universal way for superficial antibacterial modification towards almost all the surgical implanted materials, including but not limited to absorbable sutures.
Similar content being viewed by others
References
Dennis, C.; Sethu, S.; Nayak, S.; Mohan, L.; Morsi, Y.; Manivasagam, G. Suture materials—current and emerging trends. J. Biomed. Mater. Res. A 2016, 104, 1544–1559.
de la Harpe, K. M.; Kondiah, P. P. D.; Marimuthu, T.; Choonara, Y. E. Advances in carbohydrate-based polymers for the design of suture materials: a review. Carbohydr. Polym. 2021, 261, 117860.
Pillai, C. K. S.; Sharma, C. P. Review paper: absorbable polymeric surgical sutures: chemistry, production, properties, biodegradability, and performance. J. Biomater. Appl. 2010, 25, 291–366.
Ashraf, I.; Butt, E.; Veitch, D.; Wernham, A. Dermatological surgery: an update on suture materials and techniques. Part 1. Clin. Exp. Dermatol. 2021, 46, 1400–1410.
Abhari, R. E.; Martins, J. A.; Morris, H. L.; Mouthuy, P. A.; Carr, A. Synthetic sutures: clinical evaluation and future developments. J. Biomater. Appl. 2017, 32, 410–421.
Taylor, J. S.; Marten, C. A.; Potts, K. A.; Cloutier, L. M.; Cain, K. E.; Fenton, S. L.; Tatum, T. N.; James, D. A.; Myers, K. N.; Hubbs, C. A.; Burzawa, J. K.; Vachhani, S.; Nick, A. M.; Meyer, L. A.; Graviss, L. S.; Ware, K. M.; Park, A. K.; Aloia, T. A.; Bodurka, D. C.; Levenback, C. F.; Schmeler, K. M. What is the real rate of surgical site infection? J. Oncol. Pract. 2016, 12, e878–e883.
Wagner, J. C.; Wetz, A.; Wiegering, A.; Lock, J. F.; Löb, S.; Germer, C. T.; Klein, I. Successful surgical closure of infected abdominal wounds following preconditioning with negative pressure wound therapy. Langenbeck. Arch. Surg. 2021, 406, 2479–2487.
Renko, M.; Paalanne, N. Tapiainen, T.; Hinkkainen, M.; Pokka, T.; Kinnula, S.; Sinikumpu, J. J.; Uhari, M.; Serlo, W. Triclosan-containing sutures versus ordinary sutures for reducing surgical site infections in children: a double-blind, randomised controlled trial. Lancet. Infect. Dis. 2017, 17, 50–57.
Tummalapalli, M.; Anjum, S.; Kumari, S.; Gupta, B. Antimicrobial surgical sutures: recent developments and strategies. Polym. Rev. 2016, 56, 607–630.
Fields, A. C.; Pradarelli, J. C.; Itani, K. M. F. Preventing surgical site infections: looking beyond the current guidelines. JAMA 2020, 323, 1087–1088.
Wu, X.; Kubilay, N. Z.; Ren, J.; Allegranzi, B.; Bischoff, P.; Zayed, B.; Pittet, D.; Li, J. Antimicrobial-coated sutures to decrease surgical site infections: a systematic review and meta-analysis. Eur. J. Clin. Microbiol. 2017, 36, 19–32.
Deng, X.; Qasim, M.; Ali, A. Engineering and polymeric composition of drug-eluting suture: a review. J. Biomed. Mater. Res. A 2021, 109, 2065–2081.
Alshomer, F.; Madhavan, A.; Pathan, O.; Song, W. Bioactive sutures: a review of advances in surgical suture functionalisation. Curr. Med. Chem. 2017, 24, 215–223.
Lee, J.; Yoo, J.; Kim, J.; Jang, Y.; Shin, K.; Ha, E.; Ryu, S.; Kim, B. G.; Wooh, S.; Char, K. Development of multimodal antibacterial surfaces using porous amine-reactive films incorporating lubricant and silver nanoparticles. ACS Appl. Mater. Interfaces 2019, 11, 6550–6560.
Wang, X.; Liu, P.; Wu, Q.; Zheng, Z.; Xie, M.; Chen, G.; Yu, J.; Wang, X.; Li, G.; Kaplan, D. Sustainable antibacterial and antiinflammatory silk suture with surface modification of combined-therapy drugs for surgical site infection. ACS Appl. Mater. Interfaces 2022, 14, 11177–11191.
Serrano, C.; García-Fernández, L.; Fernández-Blázquez, J. P.; Barbeck, M.; Ghanaati, S.; Unger, R.; Kirkpatrick, J.; Arzt, E.; Funk, L.; Turón, P.; del Campo, A. Nanostructured medical sutures with antibacterial properties. Biomaterials 2015, 52, 291–300.
Benesch, J.; Tengvall, P. Blood protein adsorption onto chitosan. Biomaterials 2002, 23, 2561–2568.
Kim, U. J.; Lee, Y. R.; Kang, T. H.; Choi, J. W.; Kimura, S.; Wada, M. Protein adsorption of dialdehyde cellulose-crosslinked chitosan with high amino group contents. Carbohydr. Polym. 2017, 163, 34–42.
Shi, X. W.; Li, X. X.; Du, Y. M. Recent progress of chitin-based materials. Acta Polymerica Sinica (in Chinese) 2011, 1–17.
Xia, G. X.; Wu, Y. M.; Bi, Y. F.; Chen, K.; Zhang, W. W.; Liu, S. Q.; Zhang, W. J.; Liu, R. H. Antimicrobial properties and application of polysaccharides and their derivatives. Chinese J. Polym. Sci. 2021, 39, 133–146.
Li, J.; Wu, Y.; Zhao, L. Antibacterial activity and mechanism of chitosan with ultra high molecular weight. Carbohydr. Polym. 2016, 148, 200–205.
Benchamas, G.; Huang, G.; Huang, S.; Huang, H. Preparation and biological activities of chitosan oligosaccharides. Trends Food. Sci. Tech. 2021, 107, 38–44.
Shariatinia, Z. Pharmaceutical applications of chitosan. Adv. Colloid Interface Sci. 2019, 263, 131–194.
Ghasemzadeh, H.; Sheikhahmadi, M.; Nasrollah, F. Full polysaccharide crosslinked-chitosan and silver nano composites, for use as an antibacterial membrane. Chinese J. Polym. Sci. 2016, 34, 949–964.
Avcu, E.; Baştan, F. E.; Abdullah, H. Z.; Rehman, M. A. U.; Avcu, Y. Y.; Boccaccini, A. R. Electrophoretic deposition of chitosan-based composite coatings for biomedical applications: a review. Prog. Mater. Sci. 2019, 103, 69–108.
Boon-in, S.; Theerasilp, M.; Crespy, D. Marrying the incompatible for better: Incorporation of hydrophobic payloads in superhydrophilic hydrogels. J. Colloid Interface Sci. 2022, 622, 75–86.
Abdelkader, A.; Fathi, H. A.; Hamad, M. A.; Elsabahy, M. Nanomedicine: a new paradigm to overcome drug incompatibilities. J. Pharm. Pharmacol. 2020, 72, 1289–1305.
Qin, B.; Fei, C.; Bridges Andrew, A.; Mashruwala Ameya, A.; Stone Howard, A.; Wingreen Ned, S.; Bassler Bonnie, L. Cell position fates and collective fountain flow in bacterial biofilms revealed by light-sheet microscopy. Science 2020, 369, 71–77.
Ciofu, O.; Moser, C.; Jensen, P. O.; Hoiby, N. Tolerance and resistance of microbial biofilms. Nat. Rev. Microbiol. 2022, DOI: https://doi.org/10.1038/s41579-022-00682-4
Hall-Stoodley, L.; Costerton, J. W.; Stoodley, P. Bacterial biofilms: from the natural environment to infectious diseases. Nat. Rev. Microbiol. 2004, 2, 95–108.
Mahesh, L.; Kumar, V. R.; Jain, A.; Shukla, S.; Aragoneses, J. M.; Martínez González, J. M.; Fernández-Domínguez, M.; Calvo-Guirado, J. L. Bacterial adherence around sutures of different material at grafted site: a microbiological analysis. Materials 2019, 12, 2848.
Katz, S.; Izhar, M.; Mirelman, D. Bacterial adherence to surgical sutures: a possible factor in suture induced infection. Ann. Surg. 1981, 194, 35–41.
Ali-Mucheru, M. N.; Seville, M. T.; Miller, V.; Sampathkumar, P.; Etzioni, D. A. Postoperative surgical site infections: understanding the discordance between surveillance systems. Ann. Surg. 2020, 271, 94–99.
Wills, B. W.; Smith, W. R.; Arguello, A. M.; McGwin, G.; Ghanem, E. S.; Ponce, B. A. Association of surgical jacket and bouffant use with surgical site infection risk. JAMA Surg. 2020, 155, 323–328.
Alverdy, J. C.; Hyman, N.; Gilbert, J. Re-examining causes of surgical site infections following elective surgery in the era of asepsis. Lancet. Infect. Dis. 2020, 20, e38–e43.
Tomihata, K.; Suzuki, M.; Oka, T.; Ikada, Y. A new resorbable monofilament suture. Polym. Degrad. Stab. 1998, 59, 13–18.
Hu, W.; Huang, Z. M. Biocompatibility of braided poly(L-lactic acid) nanofiber wires applied as tissue sutures. Polym. Int. 2010, 59, 92–99.
Baygar, T.; Sarac, N.; Ugur, A.; Karaca, I. R. Antimicrobial characteristics and biocompatibility of the surgical sutures coated with biosynthesized silver nanoparticles. Bioorg. Chem. 2019, 86, 254–258.
Korntner, S.; Lehner, C.; Gehwolf, R.; Wagner, A.; Grütz, M.; Kunkel, N.; Tempfer, H.; Traweger, A. Limiting angiogenesis to modulate scar formation. Adv. Drug Deliver. Rev. 2019, 146, 170–189.
Konieczny, P.; Naik, S. Healing without scarring. Science 2021, 372, 346–347.
Willenborg, S.; Eming Sabine, A. Cellular networks in wound healing. Science 2018, 362, 891–892.
Rodrigues, M.; Kosaric, N.; Bonham, C. A.; Gurtner, G. C. Wound healing: a cellular perspective. Physiol. Rev. 2018, 99, 665–706.
Ip, W. K. E.; Hoshi, N.; Shouval Dror, S.; Snapper, S.; Medzhitov, R. Anti-inflammatory effect of IL-10 mediated by metabolic reprogramming of macrophages. Science 2017, 356, 513–519.
Sato, Y.; Ohshima, T.; Kondo, T. Regulatory role of endogenous Interleukin-10 in cutaneous inflammatory response of murine wound healing. Biochem. Biophys. Res. Commun. 1999, 265, 194–199.
Sun, W.; Wu, Y.; Zheng, M.; Yang, Y.; Liu, Y.; Wu, C.; Zhou, Y.; Zhang, Y.; Chen, L.; Li, H. Discovery of an orally active small-molecule tumor necrosis factor-α inhibitor. J. Med. Chem. 2020, 63, 8146–8156.
Yu, Q. J.; Fen, Z. C.; Huang, L. P.; He, J. W.; Zhou, Z. L.; Liu, F. Ellagic acid (EA), a tannin was isolated from Eucalyptus citriodora leaves and its anti-inflammatory activity. Med. Chem. Res. 2021, 30, 2277–2288.
Johnson, B. Z.; Stevenson, A. W.; Prêle, C. M.; Fear, M. W.; Wood, F. M. The role of IL-6 in skin fibrosis and cutaneous wound healing. Biomedicines 2020, 8, 101–119.
Leknes, K. N.; Selvig, K. A.; Boe, O. E.; Wikesjö, U. M. E. Tissue reactions to sutures in the presence and absence of anti-infective therapy. J. Clin. Periodontol. 2005, 32, 130–138.
Masini, B. D.; Stinner, D. J.; Waterman, S. M.; Wenke, J. C. Bacterial adherence to suture materials. J. Surg. Educ. 2011, 68, 101–104.
Markel, D. C.; Bergum, C.; Wu, B.; BouAkl, T.; Ren, W. Does suture type influence bacterial retention and biofilm formation after irrigation in a mouse model?. Clin. Orthop. Relat. Res. 2019, 477, 116–126.
Acknowledgments
This work was financially supported by the National Natural Science Foundation of China (Nos. 51973164, 52131302, 22135005 and 51833007), National Key Research and Development Program of China (2019YFA0905603) and Fundamental Research Funds for the Central Universities (No. 2042021kf0037). All of the animal experiments were conducted under protocols approved by the Institutional Animal Care and Use Committee (IACUC) of the Animal Experiment Center of Wuhan University (Wuhan, P. R. China)
Author information
Authors and Affiliations
Corresponding authors
Additional information
Notes
The authors declare no competing financial interest.
Electronic Supplementary Information of
Rights and permissions
About this article
Cite this article
Chen, YG., Li, CX., Zhang, Y. et al. Antibacterial Sutures Coated with Smooth Chitosan Layer by Gradient Deposition. Chin J Polym Sci 40, 1050–1061 (2022). https://doi.org/10.1007/s10118-022-2770-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10118-022-2770-9