Abstract
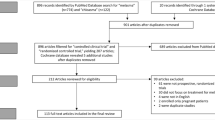
Although patients with refractory melasma have been treated using various methods, there is still no precise definition or summary of the therapies. To define refractory melasma and conduct a review of the treatments, we searched for relevant publications in PubMed, Web of Science, and the Cochrane Library, and a total of 35 references were obtained. Refractory melasma can be roughly defined as an ineffective treatment for melasma, including topical bleaching agents, chemical peels, laser therapy, microdermabrasion for more than six months, or chemical peels treated more than six times. Meanwhile, physicians should be careful when treating patients with darker skin and dermal or mixed types of melasma since these individuals do not respond well to treatment. Lasers combined with other methods, especially different types of lasers or topical agents, are considered more effective than monotherapy. Oral tranexamic acid (TXA) is a prospective cure for refractory melasma. Other methods include a combination of chemical peels, microneedling, or injections with additional therapies. In conclusion, we were able to provide a rough definition of refractory melasma and list the available therapies. According to the literature, the most prevalent treatment is laser combination therapy. However, laser treatment should be considered only after topical agents and chemical peeling have failed. Considering its side effects, efficacy, and safety, oral TXA may be a better option, but more research is needed to make a firm conclusion. Moreover, maintenance therapy is required after treatment.
Similar content being viewed by others
References
Neagu N, Conforti C, Agozzino M, Marangi GF, Morariu SH, Pellacani G et al (2022) Melasma treatment: a systematic review. J Dermatolog Treat 33:1816–1837. https://doi.org/10.1080/09546634.2021.1914313
Wang CC, Hui CY, Sue YM, Wong WR, Hong HS (2004) Intense pulsed light for the treatment of refractory melasma in Asian persons. Dermatol Surg 30:1196–1200. https://doi.org/10.1111/j.1524-4725.2004.30371.x
Sarkar R, Bansal A, Ailawadi P (2020) Future therapies in melasma: what lies ahead? Indian J Dermatol Venereol Leprol 86:8–17. https://doi.org/10.4103/ijdvl.IJDVL_633_18
Angsuwarangsee S, Polnikorn N (2003) Combined ultrapulse CO2 laser and Q-switched alexandrite laser compared with Q-switched alexandrite laser alone for refractory melasma: split-face design. Dermatol Surg 29:59–64. https://doi.org/10.1046/j.1524-4725.2003.29009.x
Arellano I, Cestari T, Ocampo-Candiani J, Azulay-Abulafia L, Bezerra Trindade Neto P, Hexsel D et al (2012) Preventing melasma recurrence: prescribing a maintenance regimen with an effective triple combination cream based on long-standing clinical severity. J Eur Acad Dermatol Venereol 26:611–618. https://doi.org/10.1111/j.1468-3083.2011.04135.x
Taylor CR, Anderson RR (1994) Ineffective treatment of refractory melasma and postinflammatory hyperpigmentation by Q-switched ruby laser. J Dermatol Surg Oncol 20:592–597. https://doi.org/10.1111/j.1524-4725.1994.tb00152.x
Manaloto RM, Alster T (1999) Erbium:YAG laser resurfacing for refractory melasma. Dermatol Surg 25:121–123. https://doi.org/10.1046/j.1524-4725.1999.08103.x
Goldberg DJ, Berlin AL, Phelps R (2008) Histologic and ultrastructural analysis of melasma after fractional resurfacing. Lasers Surg Med 40:134–138. https://doi.org/10.1002/lsm.20591
Polnikorn N (2008) Treatment of refractory dermal melasma with the MedLite C6 Q-switched nd:YAG laser: two case reports. J Cosmet Laser Ther 10:167–173. https://doi.org/10.1080/14764170802179687
Attwa E, Khater M, Assaf M, Haleem MA (2015) Melasma treatment using an erbium:YAG laser: a clinical, immunohistochemical, and ultrastructural study. Int J Dermatol 54:235–244. https://doi.org/10.1111/ijd.12477
Park BJ, Jung YJ, Ro YS, Chang SE, Kim JE (2022) Therapeutic effects of New Pulsed-Type Microneedling Radiofrequency for Refractory Facial Pigmentary disorders. Dermatol Surg 48:327–333. https://doi.org/10.1097/dss.0000000000003367
Garg S, Vashisht KR, Makadia S (2019) A prospective randomized comparative study on 60 Indian patients of melasma, comparing pixel Q-switched NdYAG (1064 nm), super skin rejuvenation (540 nm) and ablative pixel erbium YAG (2940 nm) lasers, with a review of the literature. J Cosmet Laser Ther 21:297–307. https://doi.org/10.1080/14764172.2019.1605447
Polnikorn N, Tanghetti EA (2019) Treatment of refractory melasma in asians with flat and diffractive lens picosecond alexandrite laser. Lasers Surg Med 51:S49–S50. https://doi.org/10.1002/lsm.23059
Wattanakrai P, Mornchan R, Eimpunth S (2010) Low-fluence Q-Switched neodymium-doped Yttrium Aluminum Garnet (1,064 nm) laser for the Treatment of Facial Melasma in asians. Dermatol Surg 36:76–87. https://doi.org/10.1111/j.1524-4725.2009.01383.x
Figueiredo Souza L, Trancoso Souza S (2012) Single-session intense pulsed light combined with stable fixed-dose triple combination topical therapy for the treatment of refractory melasma. Dermatol Ther 25:477–480. https://doi.org/10.1111/j.1529-8019.2012.01530.x
Wanitphakdeedecha R, Sy-Alvarado F, Patthamalai P, Techapichetvanich T, Eimpunth S, Manuskiatti W (2020) The efficacy in treatment of facial melasma with thulium 1927-nm fractional laser-assisted topical tranexamic acid delivery: a split-face, double-blind, randomized controlled pilot study. Lasers Med Sci 35:2015–2021. https://doi.org/10.1007/s10103-020-03045-8
Mokhtari F, Bahrami B, Faghihi G, Asilian A, Iraji F (2022) Fractional erbium:YAG laser (2940 nm) plus topical hydroquinone compared to intradermal tranexamic acid plus topical hydroquinone for the treatment of refractory melasma: a randomized controlled trial. J Dermatolog Treat 33:2475–2481. https://doi.org/10.1080/09546634.2021.1968996
Beyzaee AM, Goldust M, Rokni GR, Patil A, Mostaghiman R, Golpour M (2023) Comparative effectiveness and safety of topical methimazole 5% monotherapy versus combination of Q-Switched nd: YAG Laser and topical methimazole 5% in patients with refractory melasma. J Cosmet Dermatol. https://doi.org/10.1111/jocd.15641
Cunha PR, Pinto CA, Mattos CB, Cabrini DP, Tolosa JL (2015) New insight in the treatment of refractory melasma: laser Q-switched nd: YAG non-ablative fractionated followed by intense pulsed light. Dermatol Ther 28:296–299. https://doi.org/10.1111/dth.12250
Tian WCBA (2016) Novel technique to treat melasma in Chinese: the combination of 2940-nm fractional Er:YAG and 1064-nm Q-switched nd:YAG laser. J Cosmet Laser Therapy 18:72–74. https://doi.org/10.3109/14764172.2015.1063662
Hai L, Phuong B, Ha L, Lam V, Van B, Al-Niaimi F (2021) Dual Toning Method with the combination of Picosecond and Microsecond Nd:YAG in Refractory Melasma unresponsive to Picosecond alone. J Cutan Aesthet Surg 14:101–106. https://doi.org/10.4103/jcas.Jcas_30_20
Polnikorn N (2010) Treatment of refractory melasma with the MedLite C6 Q-switched nd:YAG laser and alpha arbutin: a prospective study. J Cosmet Laser Ther 12:126–131. https://doi.org/10.3109/14764172.2010.487910
Kauvar ANB (2012) Successful treatment of melasma using a combination of microdermabrasion and Q-switched nd:YAG lasers. Lasers Surg Med 44:117–124. https://doi.org/10.1002/lsm.21156
Cameli N, Abril E, Mariano M, Berardesca E (2014) Combined use of monopolar radiofrequency and transdermal drug delivery in the treatment of melasma. Dermatol Surg 40:748–755. https://doi.org/10.1111/dsu.0000000000000029
Shaikh ZI, Mashood AA (2014) Treatment of refractory melasma with combination of topical 5% magnesium ascorbyl phosphate and fluorescent pulsed light in Asian patients. Int J Dermatol 53:93–99. https://doi.org/10.1111/ijd.12195
Zamanian A, Behrangi E, Hossein Ghafarpour G, Mehran G, Espahbodi R, Hoseinzade Fakhim T et al (2015) Effect of hydroquinone plus neodymium-doped yttrium aluminium garnet laser with and without CO2 fractional laser on resistant dermal melasma. J Skin Stem Cell 2. https://doi.org/10.17795/jssc30290
Kim C, Gao JC, Moy J, Lee HS (2022) Fractional CO2 laser and adjunctive therapies in skin of color melasma patients. JAAD Int 8:118–123. https://doi.org/10.1016/j.jdin.2022.02.010
Kang WH, Chun SC, Lee S (1998) Intermittent therapy for melasma in Asian patients with combined topical agents (retinoic acid, hydroquinone and hydrocortisone): clinical and histological studies. J Dermatol 25:587–596. https://doi.org/10.1111/j.1346-8138.1998.tb02463.x
Hantash BM, Jimenez F (2009) A split-face, double-blind, randomized and placebo-controlled pilot evaluation of a novel oligopeptide for the treatment of recalcitrant melasma. J Drugs Dermatol 8:732–735
McKesey J, Tovar-Garza A, Pandya AG (2020) Melasma Treatment: an evidence-based review. Am J Clin Dermatol 21:173–225. https://doi.org/10.1007/s40257-019-00488-w
Tan AWM, Sen P, Chua SH, Goh BK (2017) Oral tranexamic acid lightens refractory melasma. Australas J Dermatol 58:e105–e8. https://doi.org/10.1111/ajd.12474
Nagaraju D, Bhattacharjee R, Vinay K, Saikia UN, Parsad D, Kumaran MS (2018) Efficacy of oral tranexemic acid in refractory melasma: a clinico-immuno-histopathological study. Dermatol Ther 31:e12704. https://doi.org/10.1111/dth.12704
Erbil H, Sezer E, Taştan B, Arca E, Kurumlu Z (2007) Efficacy and safety of serial glycolic acid peels and a topical regimen in the treatment of recalcitrant melasma. J Dermatol 34:25–30. https://doi.org/10.1111/j.1346-8138.2007.00211.x
Mashiko T, Oka A, Osawa E, Koshima I (2017) A deceptively simple solution for refractory melasma: glycolic acid peels and hydroquinone at Home. Plast Reconstr Surg Glob Open 5:e1335. https://doi.org/10.1097/gox.0000000000001335
Piquero-Casals J, Granger C, Piquero-Casals V, Garre A, Mir-Bonafé JF (2020) A treatment combination of peels, oral antioxidants, and topical therapy for refractory melasma: a report of 4 cases. Clin Cosmet Investig Dermatol 13:209–213. https://doi.org/10.2147/ccid.S242180
Wu SZ, Muddasani S, Alam M (2020) A systematic review of the efficacy and safety of Microneedling in the Treatment of Melasma. Dermatol Surg 46:1636–1641. https://doi.org/10.1097/dss.0000000000002763
Lima Ede A (2015) Microneedling in facial recalcitrant melasma: report of a series of 22 cases. Bras Dermatol 90:919–921. https://doi.org/10.1590/abd1806-4841.20154748
Ustuner P, Balevi A, Ozdemir M (2017) A split-face, investigator-blinded comparative study on the efficacy and safety of Q-switched nd:YAG laser plus microneedling with vitamin C versus Q-switched nd:YAG laser for the treatment of recalcitrant melasma. J Cosmet Laser Ther 19:383–390. https://doi.org/10.1080/14764172.2017.1342036
Ramírez-Oliveros JF, de Abreu L, Tamler C, Vilhena P, de Barros MH (2020) Microneedling with drug delivery (hydroquinone 4% serum) as an adjuvant therapy for recalcitrant Melasma. Skinmed 18:38–40
Shamsi Meymandi S, Mozayyeni A, Shamsi Meymandi M, Aflatoonian M (2020) Efficacy of microneedling plus topical 4% tranexamic acid solution vs 4% hydroquinone in the treatment of melasma: a single-blind randomized clinical trial. J Cosmet Dermatol 19:2906–2911. https://doi.org/10.1111/jocd.13392
Khalili M, Amiri R, Iranmanesh B, Zartab H, Aflatoonian M (2022) Safety and efficacy of mesotherapy in the treatment of melasma: a review article. J Cosmet Dermatol 21:118–129. https://doi.org/10.1111/jocd.14644
Garg S, Khillan K, Bharija SC (2019) Platelet-Rich plasma therapy in the treatment of recalcitrant Melasma. Dermatol Surg 45:482–484. https://doi.org/10.1097/dss.0000000000001559
Gupta AK, Gover MD, Nouri K, Taylor S (2006) The treatment of melasma: a review of clinical trials. J Am Acad Dermatol 55:1048–1065. https://doi.org/10.1016/j.jaad.2006.02.009
Rodrigues M, Pandya AG (2015) Melasma: clinical diagnosis and management options. Australas J Dermatol 56:151–163. https://doi.org/10.1111/ajd.12290
Passeron T, Genedy R, Salah L, Fusade T, Kositratna G, Laubach HJ et al (2019) Laser treatment of hyperpigmented lesions: position statement of the European Society of Laser in Dermatology. J Eur Acad Dermatol Venereol 33:987–1005. https://doi.org/10.1111/jdv.15497
Shankar K, Godse K, Aurangabadkar S, Lahiri K, Mysore V, Ganjoo A et al (2014) Evidence-based treatment for melasma: expert opinion and a review. Dermatol Ther (Heidelb) 4:165–186. https://doi.org/10.1007/s13555-014-0064-z
Ogbechie-Godec OA, Elbuluk N (2017) Melasma: an Up-to-date Comprehensive Review. Dermatol Ther (Heidelb) 7:305–318. https://doi.org/10.1007/s13555-017-0194-1
Sarkar R, Handog EB, Das A, Bansal A, Macarayo MJ, Keshavmurthy V et al (2023) Topical and systemic therapies in Melasma: a systematic review. Indian Dermatol Online J 14:769–781. https://doi.org/10.4103/idoj.idoj_490_22
Sarkar R, Katoch S (2024) Chemical peels in treatment of Melasma. Dermatol Clin 42:21–32. https://doi.org/10.1016/j.det.2023.06.003
Rivas S, Pandya AG (2013) Treatment of melasma with topical agents, peels and lasers: an evidence-based review. Am J Clin Dermatol 14:359–376. https://doi.org/10.1007/s40257-013-0038-4
Funding
This work was supported by the Hangzhou biomedical and health industry development support project (2021WJCY159), and Hangzhou medical key discipline construction project (No [37]21 − 3).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yao, H., Shen, S., Gao, X. et al. Definition of refractory melasma and its treatment: a review. Lasers Med Sci 39, 118 (2024). https://doi.org/10.1007/s10103-024-04066-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-024-04066-3