Abstract
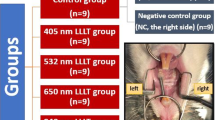
Discomfort and dull pain are known side effects of orthodontic treatment. Pain is expected to be reduced by near-infrared (NIR) lasers; however, the mechanism underlying effects of short-pulse NIR lasers in the oral and maxillofacial area remains unclear. This study aimed to examine the effects of high-frequency NIR diode laser irradiation on pain during experimental tooth movement (ETM) on 120 J. NIR laser with 910 nm wavelength, 45 W maximum output power, 300 mW average output power, and 200 ns pulse width (Lumix 2; (Lumix 2; Fisioline, Verduno CN, Italy) was used for the experiment. A nickel–titanium-closed coil was used to apply a 50-gf force between the maxillary left-side first molar and incisor in 7-week-old Sprague–Dawley rats (280–300 g) to induce ETM. We measured facial-grooming frequency and vacuous chewing movement (VCM) period between laser-irradiation and ETM groups. We performed immunofluorescent histochemistry analysis to quantify levels of Iba-1, astrocytes, and c-fos protein-like immunoreactivity (Fos-IR) in the trigeminal spinal nucleus caudalis (Vc). Compared with the ETM group, the laser irradiation group had significantly decreased facial-grooming frequency (P = 0.0036), VCM period (P = 0.043), Fos-IR (P = 0.0028), Iba-1 levels (P = 0.0069), and glial fibrillary acidic protein (GFAP) levels (P = 0.0071). High-frequency NIR diode laser irradiation appears to have significant analgesic effects on ETM-induced pain, which involve inhibiting neuronal activity, microglia, and astrocytes, and it inhibits c-fos, Iba-1, and GFAP expression, reducing ETM-induced pain in rats. High-frequency NIR diode laser application could be applied to reduce pain during orthodontic tooth movement.







Similar content being viewed by others
Availability of data and material
Not applicable.
Code availability
Not applicable.
References
Graber L, Vanarsdall R, Vig K, Huang G (2011) Orthodontics: current principles and techniques, 5th edn. Elsevier, Mosby
Flieger R, Matys J, Dominiak M (2018) The best time for orthodontic treatment for Polish children based on skeletal age analysis in accordance to refund policy of the Polish National Health Fund (NFZ). Adv Clin Exp Med 27:1377–1382. https://doi.org/10.17219/acem/69976
Krukemeyer AM, Arruda AO, Inglehart MR (2009) Pain and orthodontic treatment. Angle Orthod 79:1175–1181. https://doi.org/10.2319/121308-632R.1
Sergl HG, Klages U, Zentner A (2000) Functional and social discomfort during orthodontic treatment–effects on compliance and prediction of patients’ adaptation by personality variables. Eur J Orthod 22:307–315. https://doi.org/10.1093/ejo/22.3.307
Oliver RG, Knapman YM (1985) Attitudes to orthodontic treatment. Br J Orthod 12:179–188. https://doi.org/10.1179/bjo.12.4.179
Bos A, Hoogstraten J, Prahl-Andersen B (2005) Towards a comprehensive model for the study of compliance in orthodontics. Eur J Orthod 27:296–301. https://doi.org/10.1093/ejo/cji003
Blechman AM (1998) Pain-free and mobility-free orthodontics? Am J Orthod Dentofacial Orthop 113:379–383. https://doi.org/10.1016/S0889-5406(98)80007-3
Krishnan V (2007) Orthodontic pain: from causes to management–a review. Eur J Orthod 29:170–179. https://doi.org/10.1093/ejo/cjl081
Polat O, Karaman AI (2005) Pain control during fixed orthodontic appliance therapy. Angle Orthod 75:214–219. https://doi.org/10.1043/0003-3219(2005)075%3c0210:PCDFOA%3e2.0.CO;2
Steen Law SL, Southard KA, Law AS, Logan HL, Jakobsen JR (2000) An evaluation of preoperative ibuprofen for treatment of pain associated with orthodontic separator placement. Am J Orthod Dentofacial Orthop 118:629–635. https://doi.org/10.1067/mod.2000.110638
Bird SE, Williams K, Kula K (2007) Preoperative acetaminophen vs ibuprofen for control of pain after orthodontic separator placement. Am J Orthod Dentofacial Orthop 132:504–510. https://doi.org/10.1016/j.ajodo.2006.11.019
Matys J, Jaszczak E, Flieger R, Kostrzewska-Kaminiarz K, Grzech-Leśniak K, Dominiak M (2020) Effect of ozone and diode laser (635 nm) in reducing orthodontic pain in the maxillary arch—a randomized clinical controlled trial. Lasers Med Sci 35:487–496. https://doi.org/10.1007/s10103-019-02896-0
Kilmer PD (2010) Review article: review article. Journalism 11:369–373. https://doi.org/10.1177/1461444810365020
Chae HS, Park HJ, Hwang HR, Kwon A, Lim WH, Yi WJ, Han DH, Kim YH, Baek JH (2011) The effect of antioxidants on the production of pro-inflammatory cytokines and orthodontic tooth movement. Mol Cells 32:189–196. https://doi.org/10.1007/s10059-011-0071-1
Itoh K, Chiang CY, Li Z, Lee JC, Dostrovsky JO, Sessle BJ (2011) Central sensitization of nociceptive neurons in rat medullary dorsal horn involves purinergic P2X7 receptors. Neuroscience 192:721–731. https://doi.org/10.1016/j.neuroscience.2011.06.083
Kobayashi M, Horinuki E (2017) Neural mechanisms of nociception during orthodontic treatment. J Oral Sci 59:167–171. https://doi.org/10.2334/josnusd.16-0847
Loane DJ, Byrnes KR (2010) Role of microglia in neurotrauma. Neurotherapeutics 7:366–377. https://doi.org/10.1016/j.nurt.2010.07.002
Svensson M, Eriksson NP, Aldskogius H (1993) Evidence for activation of astrocytes via reactive microglial cells following hypoglossal nerve transection. J Neurosci Res 35:373–381. https://doi.org/10.1002/jnr.490350404
Yamamoto Y, Terayama R, Kishimoto N, Maruhama K, Mizutani M, Iida S, Sugimoto T (2015) Activated microglia contribute to convergent nociceptive inputs to spinal dorsal horn neurons and the development of neuropathic pain. Neurochem Res 40:1000–1012. https://doi.org/10.1007/s11064-015-1555-8
Bernhardt MK, Southard KA, Batterson KD, Logan HL, Baker KA, Jakobsen JR (2001) The effect of preemptive and/or postoperative ibuprofen therapy for orthodontic pain. Am J Orthod Dentofacial Orthop 120:20–27. https://doi.org/10.1067/mod.2001.115616
Polat O, Karaman AI, Durmus E (2005) Effects of preoperative ibuprofen and naproxen sodium on orthodontic pain. Angle Orthod 75:791–796. https://doi.org/10.1043/0003-3219(2005)75[791:EOPIAN]2.0.CO;2
Tortamano A, Lenzi DC, Haddad AC, Bottino MC, Dominguez GC, Vigorito JW (2009) Low-level laser therapy for pain caused by placement of the first orthodontic archwire: a randomized clinical trial. Am J Orthod Dentofacial Orthop 136:662–667. https://doi.org/10.1016/j.ajodo.2008.06.028
Youssef M, Ashkar S, Hamade E, Gutknecht N, Lampert F, Mir M (2008) The effect of low-level laser therapy during orthodontic movement: a preliminary study. Lasers Med Sci 23:27–33. https://doi.org/10.1007/s10103-007-0449-7
Lou Z, Zhang C, Gong T, Xue C, Scholp A, Jiang JJ (2019) Wound-healing effects of 635-nm low-level laser therapy on primary human vocal fold epithelial cells: an in vitro study. Lasers Med Sci 34:547–554. https://doi.org/10.1007/s10103-018-2628-0
Suzuki R, Takakuda K (2016) Wound healing efficacy of a 660-nm diode laser in a rat incisional wound model. Lasers Med Sci 31:1683–1689. https://doi.org/10.1007/s10103-016-2038-0
de Souza Merli LA, de Medeiros VP, Toma L, Reginato RD, Katchburian E, Nader HB, Faloppa F (2012) The low level laser therapy effect on the remodeling of bone extracellular matrix. Photochem Photobiol 88:1293–1301. https://doi.org/10.1111/j.1751-1097.2012.01172.x
Wu JY, Wang YH, Wang GJ, Ho ML, Wang CZ, Yeh ML, Chen CH (2012) Low-power GaAlAs laser irradiation promotes the proliferation and osteogenic differentiation of stem cells via IGF1 and BMP2. PLoS One 7:e44027. https://doi.org/10.1371/journal.pone.0044027
Soares DM, Ginani F, Henriques ÁG, Barboza CA (2015) Effects of laser therapy on the proliferation of human periodontal ligament stem cells. Lasers Med Sci 30:1171–1174. https://doi.org/10.1007/s10103-013-1436-9
Doshi-Mehta G, Bhad-Patil WA (2012) Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. Am J Orthod Dentofacial Orthop 141:289–297. https://doi.org/10.1016/j.ajodo.2011.09.009
Capon A, Mordon S (2003) Can thermal lasers promote skin wound healing? Am J Clin Dermatol 4:1–12. https://doi.org/10.2165/00128071-200304010-00001
Hashmi JT, Huang YY, Sharma SK, Kurup DB, De Taboada L, Carroll JD, Hamblin MR (2010) Effect of pulsing in low-level light therapy. Lasers Surg Med 42:450–466. https://doi.org/10.1002/lsm.20950
Joensen J, Ovsthus K, Reed RK, Hummelsund S, Iversen VV, Lopes-Martins RÁ, Bjordal JM (2012) Skin penetration time-profiles for continuous 810 nm and Superpulsed 904-nm lasers in a rat model. Photomed Laser Surg 30:688–694. https://doi.org/10.1089/pho.2012.3306
Marini I, Bartolucci ML, Bortolotti F, Innocenti G, Gatto MR, Alessandri Bonetti G (2015) The effect of diode superpulsed low-level laser therapy on experimental orthodontic pain caused by elastomeric separators: a randomized controlled clinical trial. Lasers Med Sci 30:35–41. https://doi.org/10.1007/s10103-013-1345-y
Marini I, Gatto MR, Bonetti GA (2010) Effects of superpulsed low-level laser therapy on temporomandibular joint pain. Clin J Pain 26:611–616. https://doi.org/10.1097/AJP.0b013e3181e0190d
Kheshie AR, Alayat MS, Ali MM (2014) High-intensity versus low-level laser therapy in the treatment of patients with knee osteoarthritis: a randomized controlled trial. Lasers Med Sci 29:1371–1376. https://doi.org/10.1007/s10103-014-1529-0
Gunji H, Kunimatsu R, Tsuka Y, Yoshimi Y, Sumi K, Awada T, Nakajima K, Kimura A, Hiraki T, Hirose N, Yanoshita M, Tanimoto K (2018) Effect of high-frequency near-infrared diode laser irradiation on periodontal tissues during experimental tooth movement in rats. Lasers Surg Med. https://doi.org/10.1002/lsm.22797
Noda M, Aoki A, Mizutani K, Lin T, Komaki M, Shibata S, Izumi Y (2016) High-frequency pulsed low-level diode laser therapy accelerates wound healing of tooth extraction socket: an in vivo study. Lasers Surg Med 48:955–964. https://doi.org/10.1002/lsm.22560
Sakata S, Kunimatsu R, Tsuka Y, Nakatani A, Hiraki T, Gunji H, Hirose N, Yanoshita M, Putranti NAR, Tanimoto K (2020) High-frequency near-infrared diode laser irradiation attenuates IL-1β-induced expression of inflammatory cytokines and matrix metalloproteinases in human primary chondrocytes. J Clin Med 9:E881. https://doi.org/10.3390/jcm9030881
Kawasaki K, Shimizu N (2000) Effects of low-energy laser irradiation on bone remodeling during experimental tooth movement in rats. Lasers Surg Med 26:282–291. https://doi.org/10.1002/(SICI)1096-9101(2000)26:3%3c282::AID-LSM6%3e3.0.CO;2-X
Yang Z, Cao Y, Wang Y, Luo W, Hua X, Lu Y, Liao Z, Lai W, Zhao Z (2009) Behavioural responses and expression of P2X3 receptor in trigeminal ganglion after experimental tooth movement in rats. Arch Oral Biol 54:63–70. https://doi.org/10.1016/j.archoralbio.2008.09.003
Luo W, Fu R, Tan Y, Fang B, Yang Z (2014) Chemokine CCL2 up-regulated in the medullary dorsal horn astrocytes contributes to nocifensive behaviors induced by experimental tooth movement. Eur J Oral Sci 122:27–35. https://doi.org/10.1111/eos.12099
Liao L, Long H, Zhang L, Chen H, Zhou Y, Ye N, Lai W (2014) Evaluation of pain in rats through facial expression following experimental tooth movement. Eur J Oral Sci 122:121–124. https://doi.org/10.1111/eos.12110
Terayama R, Yamamoto Y, Kishimoto N, Tabata M, Maruhama K, Iida S, Sugimoto T (2016) Differential changes in neuronal excitability in the spinal dorsal horn after spinal nerve ligation in rats. Neurochem Res 41:2880–2889. https://doi.org/10.1007/s11064-016-2003-0
Terayama R, Tabata M, Maruhama K, Iida S (2018) A3 adenosine receptor agonist attenuates neuropathic pain by suppressing activation of microglia and convergence of nociceptive inputs in the spinal dorsal horn. Exp Brain Res 236:3203–3213. https://doi.org/10.1007/s00221-018-5377-1
Yang Z, Luo W, Hou J, Zhao Z, Jian F, Wamalwa P, Lai W, Wang J, Wang Y, Liao Z (2009) Development of a behavior model of pain induced by experimental tooth movement in rats. Eur J Oral Sci 117:380–384. https://doi.org/10.1111/j.1600-0722.2009.00639.x
Qiao H, Gao Y, Zhang C, Zhou H (2015) Increased expression of TRPV1 in the trigeminal ganglion is involved in orofacial pain during experimental tooth movement in rats. Eur J Oral Sci 123:17–23. https://doi.org/10.1111/eos.12158
Long H, Wang Y, Jian F, Liao LN, Yang X, Lai WL (2016) Current advances in orthodontic pain. Int J Oral Sci 8:67–75. https://doi.org/10.1038/ijos.2016.24
Fujiyoshi Y, Yamashiro T, Deguchi T, Sugimoto T, Takano-Yamamoto T (2000) The difference in temporal distribution of c-Fos immunoreactive neurons between the medullary dorsal horn and the trigeminal subnucleus oralis in the rat following experimental tooth movement. Neurosci Lett 283:205–208. https://doi.org/10.1016/s0304-3940(00)00962-9
Watanabe M, Tanaka E, Suemune S, Satoda T, Maeda N, Uchida T, Tanne K (2003) Expression of c-Fos protein in the trigeminal nuclear complex resulting from quantified force application to the rat molar. J Oral Rehabil 30:1128–1137. https://doi.org/10.1046/j.1365-2842.2003.01158.x
Hattori Y, Watanabe M, Iwabe T, Tanaka E, Nishi M, Aoyama J, Satoda T, Uchida T, Tanne K (2004) Administration of MK-801 decreases c-Fos expression in the trigeminal sensory nuclear complex but increases it in the midbrain during experimental movement of rat molars. Brain Res 1021:183–191. https://doi.org/10.1016/j.brainres.2004.06.048
Sagar SM, Sharp FR, Curran T (1988) Expression of c-fos protein in brain: metabolic mapping at the cellular level. Science 240:1328–1331. https://doi.org/10.1126/science.3131879
Watkins LR, Maier SF (2003) Glia: a novel drug discovery target for clinical pain. Nat Rev Drug Discov 2:973–985. https://doi.org/10.1038/nrd1251
Imai Y, Ibata I, Ito D, Ohsawa K, Kohsaka S (1996) A novel gene iba1 in the major histocompatibility complex class III region encoding an EF hand protein expressed in a monocytic lineage. Biochem Biophys Res Commun 224:855–862. https://doi.org/10.1006/bbrc.1996.1112
Utans U, Arceci RJ, Yamashita Y, Russell ME (1995) Cloning and characterization of allograft inflammatory factor-1: a novel macrophage factor identified in rat cardiac allografts with chronic rejection. J Clin Invest 95:2954–2962. https://doi.org/10.1172/JCI118003
Jacque CM, Vinner C, Kujas M, Raoul M, Racadot J, Baumann NA (1978) Determination of glial fibrillary acidic protein (GFAP) in human brain tumors. J Neurol Sci 35:147–155. https://doi.org/10.1016/0022-510x(78)90107-7
Pekny M, Stanness KA, Eliasson C, Betsholtz C, Janigro D (1998) Impaired induction of blood–brain barrier properties in aortic endothelial cells by astrocytes from GFAP-deficient mice. Glia 22:390–400. https://doi.org/10.1002/(SICI)1098-1136(199804)22:4%3c390::AID-GLIA8%3e3.0.CO;2-7
Deguchi T, Kim DG, Kamioka H (2017) CO2 low-level laser therapy has an early but not delayed pain effect during experimental tooth movement. Orthod Craniofac Res 20 Suppl 1:172–176. https://doi.org/10.1111/ocr.12158
Seiryu M, Deguchi T, Fujiyama K, Sakai Y, Daimaruya T, Takano-Yamamoto T (2010) Effects of CO2 laser irradiation of the gingiva during tooth movement. J Dent Res 89:537–542. https://doi.org/10.1177/0022034510363230
Acknowledgements
We are grateful to Drs. P. K. DenBesten, W. Li, T.Q. Le, Y. Zhang, L. Zhu, and Y. Nakano of the Department of Orofacial Sciences, University of California at San Francisco, who gave us opportunity and advice to start this research project. The authors would like to thank Emeritus Professor Kazuo Tanne of the Department of Orthodontics and Craniofacial Developmental Biology, Hiroshima University Graduate School of Biomedical Sciences, for kindly providing advice to this work. This work was performed at the Research Center for Molecular Medicine, Hiroshima University.
Funding
This work was funded by grants from the Japan Society for Promotions of Science (grant numbers: 19K10385, 20K18759, and 20K10226).
Author information
Authors and Affiliations
Contributions
Ayaka Nakatani conducted the main experiments and prepared the manuscript. Ayaka Nakatani and Ryo Kunimatsu analyzed the data and contributed clarifications and guidance on the manuscript. Ryo Kunimatsu and Yuji Tsuka conceived and designed the experiments. Ayaka Nakatani, Kayo Horie, Hidemi Gunji, Shuzou Sakata, Shota Ito, and Ryuji Terayama performed the experiments. Ryo Kunimatsu, Isamu Kado, and Nurul Aisyah Rizky Putranti prepared the manuscript. Totaro Tanimoto and Ryuji Terayama designed and supervised the study. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval
All experimental protocols were approved by the Ethics Committee for Animal Experiments of Hiroshima University School of Dentistry (approval number A17-187). All procedures performed in studies were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nakatani, A., Kunimatsu, R., Tsuka, Y. et al. Effects of high-frequency near infrared laser irradiation on experimental tooth movement–induced pain in rats. Lasers Med Sci 37, 2697–2706 (2022). https://doi.org/10.1007/s10103-022-03543-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-022-03543-x