Abstract
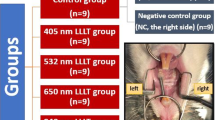
High-frequency near-infrared (NIR) semiconductor laser-irradiation has an unclear effect on nociception in the compressed lateral periodontal ligament region, a peripheral nerve region. This study aimed to investigate the effects of NIR semiconductor laser irradiation, with a power of 120 J, on inflammatory pain markers and neuropeptides induced in the compressed lateral periodontal ligament area during ETM. A NIR semiconductor laser [910 nm wavelength, 45 W maximum output power, 300 mW average output power, 30 kHz frequency, and 200 ns pulse width (Lumix 2; Fisioline, Verduno, Italy)] was used. A nickel-titanium closed coil that generated a 50-g force was applied to the maxillary left-side first molars and incisors in 7-week-old Sprague–Dawley (280–300 g) rats to induce experimental tooth movement (ETM) for 24 h. Ten rats were divided into two groups (ETM + laser, n = 5; ETM, n = 5). The right side of the ETM group (i.e., the side without induced ETM) was evaluated as the untreated group. We performed immunofluorescent histochemistry analysis to quantify the interleukin (IL)-1β, cyclooxygenase-2 (COX2), prostaglandin E2 (PGE2), and neuropeptide [calcitonin gene-related peptide (CGRP)] expression in the compressed region of the periodontal tissue. Post-hoc Tukey–Kramer tests were used to compare the groups. Compared with the ETM group, the ETM + laser group showed significant suppression in IL-1β (176.2 ± 12.3 vs. 310.8 ± 29.5; P < 0.01), PGE2 (104.4 ± 14.34 vs. 329.6 ± 36.52; P < 0.01), and CGRP (36.8 ± 4.88 vs. 78.0 ± 7.13; P < 0.01) expression. High-frequency NIR semiconductor laser irradiation exerts significant effects on ETM-induced inflammation. High-frequency NIR semiconductor laser irradiation can reduce periodontal inflammation during orthodontic tooth movement.






Similar content being viewed by others
Data availability
Not applicable.
References
Dimberg L, Arnrup K, Bondemark L (2015) The impact of malocclusion on the quality of life among children and adolescents: a systematic review of quantitative studies. Eur J Orthod 37:238–247. https://doi.org/10.1093/ejo/cju046
Kragt L, Dhamo B, Wolvius EB, Ongkosuwito EM (2016) The impact of malocclusions on oral health-related quality of life in children-a systematic review and meta-analysis. Clin Oral Investig 20:1881–1894. https://doi.org/10.1007/s00784-015-1681-3
Erdinç AM, Dinçer B (2004) Perception of pain during orthodontic treatment with fixed appliances. Eur J Orthod 26:79–85. https://doi.org/10.1093/ejo/26.1.79
Krishnan V (2007) Orthodontic pain: from causes to management—a review. Eur J Orthod 29:170–179. https://doi.org/10.1093/ejo/cjl081
Bergius M, Berggren U, Kiliaridis S (2002) Experience of pain during an orthodontic procedure. Eur J Oral Sci 110:92–98. https://doi.org/10.1034/j.1600-0722.2002.11193.x
Celebi F, Turk T, Bicakci AA (2019) Effects of low-level laser therapy and mechanical vibration on orthodontic pain caused by initial archwire. Am J Orthod Dentofacial Orthop 156:87–93. https://doi.org/10.1016/j.ajodo.2018.08.021
Polat O, Karaman AI (2005) Pain control during fixed orthodontic appliance therapy. Angle Orthod 75:214–219. https://doi.org/10.1043/0003-3219(2005)075%3c0210:PCDFOA%3e2.0.CO;2
Oliver RG, Knapman YM (1985) Attitudes to orthodontic treatment. Br J Orthod 12:179–188. https://doi.org/10.1179/bjo.12.4.179
O’Connor PJ (2000) Patients’ perceptions before, during, and after orthodontic treatment. J Clin Orthod 34:591–592
Xiaoting L, Yin T, Yangxi C (2010) Interventions for pain during fixed orthodontic appliance therapy: a systematic review. Angle Orthod 80:925–932. https://doi.org/10.2319/010410-10.1
Monk AB, Harrison JE, Worthington HV, Teague A (2017) Pharmacological interventions for pain relief during orthodontic treatment. Cochrane Database Syst Rev 11:CD003976. https://doi.org/10.1002/14651858.CD003976.pub2
Sandhu SS, Cheema MS, Khehra HS (2016) Comparative effectiveness of pharmacologic and nonpharmacologic interventions for orthodontic pain relief at peak pain intensity: a Bayesian network meta-analysis. Am J Orthod Dentofacial Orthop 150:13–32. https://doi.org/10.1016/j.ajodo.2015.12.025
Gupta M, Kandula S, Laxmikanth SM, Vyavahare SS, Reddy SBH, Ramachandra CS (2014) Controlling pain during orthodontic fixed appliance therapy with non-steroidal anti-inflammatory drugs (NSAID): a randomized, double-blinded, placebo-controlled study. J Orofac Orthop 75:471–476. https://doi.org/10.1007/s00056-014-0243-7
Bernhardt MK, Southard KA, Batterson KD, Logan HL, Baker KA, Jakobsen JR (2001) The effect of preemptive and/or postoperative ibuprofen therapy for orthodontic pain. Am J Orthod Dentofacial Orthop 120:20–27. https://doi.org/10.1067/mod.2001.115616
Ren C, McGrath C, Yang Y (2015) The effectiveness of low-level diode laser therapy on orthodontic pain management: a systematic review and meta-analysis. Lasers Med Sci 30:1881–1893. https://doi.org/10.1007/s10103-015-1743-4
Nóbrega C, da Silva EMK, de Macedo CR (2013) Low-level laser therapy for treatment of pain associated with orthodontic elastomeric separator placement: a placebo-controlled randomized double-blind clinical trial. Photomed Laser Surg 31:10–16. https://doi.org/10.1089/pho.2012.3338
Fleming PS, Strydom H, Katsaros C, MacDonald L, Curatolo M, Fudalej P, Pandis N (2016) Non-pharmacological interventions for alleviating pain during orthodontic treatment. Cochrane Database Syst Rev 12:CD010263. https://doi.org/10.1002/14651858.CD010263.pub2
Li FJ, Zhang JY, Zeng XT, Guo Y (2015) Low-level laser therapy for orthodontic pain: a systematic review. Lasers Med Sci 30:1789–1803. https://doi.org/10.1007/s10103-014-1661-x
Capon A, Mordon S (2003) Can thermal lasers promote skin wound healing? Am J Clin Dermatol 4:1–4. https://doi.org/10.2165/00128071-200304010-00001
Walsh LJ (1997) The current status of low level laser therapy in dentistry. Part 2. Hard tissue applications. Aust Dent J 42:302–306. https://doi.org/10.1111/j.1834-7819.1997.tb00134.x
Bjordal JM, Couppé C, Chow RT, Tunér J, Ljunggren EAA (2003) A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Aust J Physiother 49:107–116. https://doi.org/10.1016/s0004-9514(14)60127-6
Barretto SR, de Melo GC, dos Santos JC, de Oliveira MGB, Pereira-Filho RN, Alves AVF, Ribeiro MAG, Lima-Verde IB, Quintans Júnior LJ, de Albuquerque-Júnior RLC, Bonjardim LR (2013) Evaluation of anti-nociceptive and anti-inflammatory activity of low-level laser therapy on temporomandibular joint inflammation in rodents. J Photochem Photobiol B 129:135–142. https://doi.org/10.1016/j.jphotobiol.2013.10.002
Hashmi JT, Huang YY, Sharma SK, Kurup DB, De Taboada L, Carroll JD, Hamblin MR (2010) Effect of pulsing in low-level light therapy. Lasers Surg Med 42:450–466. https://doi.org/10.1002/lsm.20950
Joensen J, Ovsthus K, Reed RK, Hummelsund S, Iversen VV, Lopes-Martins RÁ, Bjordal JM (2012) Skin penetration time-profiles for continuous 810 nm and superpulsed 904-nm lasers in a rat model. Photomed Laser Surg 30:688–694. https://doi.org/10.1089/pho.2012.3306
Kilmer PD (2010) Review article: review article: review article. Journalism 11:369–373. https://doi.org/10.1177/1461444810365020
Chae HS, Park HJ, Hwang HR, Kwon A, Lim WH, Yi WJ, Han DH, Kim YH, Baek JH (2011) The effect of antioxidants on the production of pro-inflammatory cytokines and orthodontic tooth movement. Mol Cells 32:189–196. https://doi.org/10.1007/s10059-011-0071-1
Fujiyoshi Y, Yamashiro T, Deguchi T, Sugimoto T, Takano-Yamamoto T (2000) The difference in temporal distribution of c-fos immunoreactive neurons between the medullary dorsal horn and the trigeminal subnucleus oralis in the rat following experimental tooth movement. Neurosci Lett 283:205–208. https://doi.org/10.1016/s0304-3940(00)00962-9
Watanabe M, Tanaka E, Suemune S, Satoda T, Maeda N, Uchida T, Tanne K (2003) Expression of c-fos protein in the trigeminal nuclear complex resulting from quantified force application to the rat molar. J Oral Rehabil 30:1128–1137. https://doi.org/10.1046/j.1365-2842.2003.01158.x
Nakatani A, Kunimatsu R, Tsuka Y et al (2022) Effects of high-frequency NIR laser irradiation on experimental tooth movement-induced pain in rats. Lasers Med Sci. https://doi.org/10.1007/s10103-022-03543-x
Kunimatsu R, Kimura A, Tsuka Y et al (2020) Baicalin inhibits root resorption during tooth movement in a rodent model. Arch Oral Biol 116:104770. https://doi.org/10.1016/j.archoralbio.2020.104770
Kawasaki K, Shimizu N (2000) Effects of low-energy laser irradiation on bone remodeling during experimental tooth movement in rats. Lasers Surg Med 26:282–291. https://doi.org/10.1002/(sici)1096-9101(2000)26:3%3c282::aid-lsm6%3e3.0.co;2-x
Gunji H, Kunimatsu R, Tsuka Y et al (2018) Effect of high-frequency near-infrared diode laser irradiation on periodontal tissues during experimental tooth movement in rats. Lasers Surg Med 780:772–780. https://doi.org/10.1002/lsm.22797
Storey E (1973) The nature of tooth movement. Am J Orthod 63:292–314. https://doi.org/10.1016/0002-9416(73)90353-9
Kyomen S, Tanne K (1997) Influences of aging changes in proliferative rate of PDL cells during experimental tooth movement in rats. Angle Orthod 67:67–72. https://doi.org/10.1043/0003-3219(1997)067%3c0067:IOACIP%3e2.3.CO;2
Ren Y, Vissink A (2008) Cytokines in crevicular fluid and orthodontic tooth movement. Eur J Oral Sci 116:89–97. https://doi.org/10.1111/j.1600-0722.2007.00511.x
Kapoor P, Monga N, Kharbanda OP, Kapila S, Miglani R, Moganty R (2014) Effect of orthodontic forces on levels of enzymes in gingival crevicular fluid (GCF): a systematic review. Prog Orthod 15:1–22. https://doi.org/10.1590/2177-6709.24.2.40.e1-22.onl
Baba S, Kuroda N, Arai C, Nakamura Y, Sato T (2011) Immunocompetent cells and cytokine expression in the rat periodontal ligament at the initial stage of orthodontic tooth movement. Arch Oral Biol 56:466–473. https://doi.org/10.1016/j.archoralbio.2010.11.010
Kanjanamekanant K, Luckprom P, Pavasant P (2013) Mechanical stress-induced interleukin-1beta expression through adenosine triphosphate/P2X7 receptor activation in human periodontal ligament cells. J Periodont Res 48:169–176. https://doi.org/10.1111/j.1600-0765.2012.01517.x
Matsumoto Y, Sringkarnboriboon S, Ono T (2017) Proinflammatory mediators related to orthodontically induced periapical root resorption in rat mandibular molars. Eur J Orthod 39:686–691. https://doi.org/10.1093/ejo/cjx033
Norevall LI, Forsgren S, Matsson L (1995) Expression of neuropeptides (CGRP, substance P) during and after orthodontic tooth movement in the rat. Eur J Orthod 17:311–325. https://doi.org/10.1093/ejo/17.4.311
Long H, Liao L, Gao M, Ma W, Zhou Y, Jian F, Wang Y, Lai W (2015) Periodontal CGRP contributes to orofacial pain following experimental tooth movement in rats. Neuropeptides 52:31–37. https://doi.org/10.1016/j.npep.2015.06.006
Sakurai Y, Yamaguchi M, Abiko Y (2000) Inhibitory effect of low-level laser irradiation on LPS-stimulated prostaglandin E2 production and cyclooxygenase-2 in human gingival fibroblasts. Eur J Oral Sci 108:29–34. https://doi.org/10.1034/j.1600-0722.2000.00783.x
Shimizu N, Yamaguchi M, Goseki T, Shibata Y, Takiguchi H, Iwasawa T, Abiko Y (1995) Inhibition of prostaglandin E2 and interleukin 1-β production by low-power laser irradiation in stretched human periodontal ligament cells. J Dent Res 74:1382–1388. https://doi.org/10.1177/00220345950740071001
Mayahara K, Yamaguchi A, Sakaguchi M, Igarashi Y, Shimizu N (2010) Effect of Ga-A1-As laser irradiation on COX-2 and cPLA2-α expression in compressed human periodontal ligament cells. Lasers Surg Med 42:489–493. https://doi.org/10.1002/lsm.20871
de Jesus JF, Spadacci-Morena DD, dos Anjos Rabelo ND, Pinfildi CE, Fukuda TY, Plapler H (2015) Low-level laser therapy in IL-1β, COX-2, and PGE2 modulation in partially injured Achilles tendon. Lasers Med Sci 30:153–158. https://doi.org/10.1007/s10103-014-1636-y
Sharma SK, Kharkwal GB, Sajo M, Huang YY, De Taboada L, McCarthy T, Hamblin MR (2011) Dose response effects of 810-nm laser light on mouse primary cortical neurons. Lasers Surg Med 43:851–859. https://doi.org/10.1002/lsm.21100
Ohshiro T, Ohshiro T, Sasaki K, Takenouchi K, Kageyama Y, Kozuma M, Ohshiro N (2016) History of medical laser devices and recommendations for clinical use of laser devices. Nippon Laser Igakkaishi 36:494–498. https://doi.org/10.2530/jslsm.jslsm-36_0047
Wagner VP, Curra M, Webber LP, Nör C, Matte U, Meurer L, Martins MD (2016) Photobiomodulation regulates cytokine release and new blood vessel formation during oral wound healing in rats. Lasers Med Sci 31:665–671. https://doi.org/10.1007/s10103-016-1904-0
Fekrazad R, Chiniforush N, Bouraima SA, Valipour M (2012) Low level laser therapy in management of complications after intra oral surgeries. J Lasers Med Sci 3:135–140
Kunimatsu R, Gunji H, Tsuka Y et al (2018) Effects of high-frequency near-infrared diode laser irradiation on the proliferation and migration of mouse calvarial osteoblasts. Lasers Med Sci 33:959–966. https://doi.org/10.1007/s10103-017-2426-0
Wu JY, Chen CH, Wang CZ, Ho ML, Yeh ML, Wang YH (2013) Low-power laser irradiation suppresses inflammatory response of human adipose-derived stem cells by modulating intracellular cyclic AMP level and NF-κB activity. PLoS One 8:e54067. https://doi.org/10.1371/journal.pone.0054067
Yin K, Zhu R, Wang S, Zhao RC (2017) Low level laser (LLL) attenuate LPS-induced inflammatory responses in mesenchymal stem cells via the suppression of NF-κB signaling pathway in vitro. PLoS One 12:e0179175. https://doi.org/10.1371/journal.pone.0179175
Karu T (2010) Mitochondrial mechanisms of photobiomodulation in context of new data about multiple roles of ATP. Photomed Laser Surg 28:159–160. https://doi.org/10.1089/pho.2010.2789
Sakata S, Kunimatsu R, Tsuka Y et al (2020) High-frequency near-infrared diode laser irradiation attenuates IL-1β-induced expression of inflammatory cytokines and matrix metalloproteinases in human primary chondrocytes. J Clin Med 9:881. https://doi.org/10.3390/jcm9030881
Sakata S, Kunimatsu R, Tsuka Y et al (2022) High-frequency near-infrared diode laser irradiation suppresses IL-1β-induced inflammatory cytokine expression and NF-κB signaling pathways in human primary chondrocytes. Lasers Med Sci 37:1193–1201. https://doi.org/10.1007/s10103-021-03371-5
Silveira LB, Prates RA, Novelli MD, Marigo HA, Garrocho AA, Amorim JC, Sousa GR, Pinotti M, Ribeiro MS (2008) Investigation of mast cells in human gingiva following low-intensity laser irradiation. Photomed Laser Surg 26:315–321. https://doi.org/10.1089/pho.2007.2140
Acknowledgements
The authors would like to thank Emeritus Professor Kazuo Tanne of the Department of Orthodontics and Craniofacial Developmental Biology, Hiroshima University Graduate School of Biomedical Sciences, for kindly providing advice to this work. This work was performed at the Research Center for Molecular Medicine, Hiroshima University.
Funding
This work was funded by grants from the Japan Society for Promotions of Science (grant numbers: 19K10385, 20K10226 and 21K21041).
Author information
Authors and Affiliations
Contributions
Ayaka Nakatani conducted the main experiments and prepared the manuscript. Ayaka Nakatani and Ryo Kunimatsu analyzed the data and contributed clarifications and guidance on the manuscript. Ryo Kunimatsu and Yuji Tsuka conceived and designed the experiments. Ayaka Nakatani, Shuzou Sakata, and Shota Ito performed the experiments. Ayaka Nakatani,Ryo Kunimatsu, Isamu Kado, Shota Ito and Nurul Aisyah Rizky Putranti prepared the manuscript. Totaro Tanimoto and Ryuji Terayama designed and supervised the study.
All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval statement
All experimental protocols were approved by the Ethics Committee for Animal Experiments of Hiroshima University School of Dentistry (approval number A17-187). All procedures performed in the study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflicts of interest statement
The authors declare no conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nakatani, A., Kunimatsu, R., Tsuka, Y. et al. High-frequency near-infrared semiconductor laser irradiation suppressed experimental tooth movement-induced inflammatory pain markers in the periodontal ligament tissues of rats. Lasers Med Sci 38, 109 (2023). https://doi.org/10.1007/s10103-023-03761-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-023-03761-x