Abstract
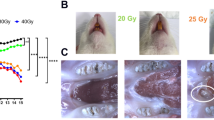
To investigate whether low-level laser therapy (LLLT), at different times of application (immediate and late) in the region of the parotid glands, has a distance effect on the microarchitecture of the trabecular bone in mandible of rats irradiated by volumetric modular arc therapy (VMAT). Thirty adult Wistar rats were randomly divided into placebo control groups (CG, n = 2), only radiotherapy (RG, n = 2), only LPLT (LG, n = 2), and two other groups using LLLT in the immediate time (24 h) (ILG, n = 12) and late (120 h) (LLG, n = 12) to radiotherapy by VMAT in a single dose of 12 Gy. LLLT with AsGaAl laser (660 nm, 100 mW), a spot size of 0.0028 cm2, was applied in three points in the region of the right parotid gland, with energy of 2 J/cm2, 20 s per point, for 10 consecutive days. After euthanasia, the right hemimandibles of each animal were dissected, prepared, and analyzed by computerized microtomography (micro-CT) and histomorphometry. The different groups were analyzed by the Tukey and Bonferroni multiple comparison tests. The micro-CT analysis found statistically significant differences between the groups, especially in the LLG, which had the highest average bone volume compared to the CG (p = 0.001) and ILG (p = 0.002) and a greater number of trabeculae than the CG (p = 0.000) and ILG (p = 0.031). The ILG also had a higher number of trabeculae than the CG (p = 0.005). Trabecula separation (Tb.Sp) was lower in the LLG (p = 0.000) and ILG (p = 0.002) when compared to the CG. In the histomorphometry, there was no statistical difference between the groups in relation to all the analyzed variables. Micro-CT analysis showed that the LLLT, even applied at a distance, both in the immediate and late VMAT times, has an effect on the mandibular bone microarchitecture by increasing the volume and number of trabeculae and decreasing the spaces between them.




Similar content being viewed by others
References
Dai X, Zhao Y, Liang Z, Dassarath M, Wang L, Jin L, Chen L, Dong J, Preço RA, Ma CM (2015) Volumetric-modulated arc therapy for oropharyngeal carcinoma: a dosimetric and delivery efficiency comparison with static-field IMRT. Physica Med 31:54–59. https://doi.org/10.1016/j.ejmp.2014.09.003
Lee SW, Kang KW, Wu HG (2016) Prospective investigation and literature review of tolerance dose on salivary glands using quantitative salivary gland scintigraphy in the intensity-modulated radiotherapy era. Head Neck 38(Suppl 1):1746–1755. https://doi.org/10.1002/hed.24310
Bahl A, Arun SO, Satinder K, Roshan V, Arun E, Sudhir B, Jaimanti B, Naresh P, Sushmita G (2017) Evaluation of acute toxicity and early clinical outcome in head and neck cancers treated with conventional radiotherapy and simultaneous integrated boost arc radiotherapy. World J Oncol, 8(4):117–121. https://doi.org/10.14740/wjon1049w
Garibaldi C, Jereczek-Fossa BA, Marvaso G, Dicuonzo S, Rojas DP, Cattani F, Starzyńska A, Ciardo D, Surgo A, Leonardi MC, Ricotti R (2017) Recent advances in radiation oncology. Ecancermedicalscience 30(11):785. https://doi.org/10.3332/ecancer.2017.785
Mallya SM, Tetradis S (2018) Imaging of radiation and medication related osteonecrosis. Radiol Clin North Am 56(1):77–89. https://doi.org/10.1016/j.rcl.2017.08.006
Rivero JA, Shamji O, Kolokythas A (2017) Osteoradionecrosis: a review of pathophysiology, prevention and pharmacologic management using pentoxifylline, α-tocopherol, and clodronate. Oral Surg Oral Med Oral Pathol Oral Radiol 124(5):464–471. https://doi.org/10.1016/j.oooo.2017.08.004
Poort LJ, Ludlage JHB, Lie N, Böckmann RA, Odekerken JCE, Hoebers FJ, Kessler PAWH (2017) The histological and histomorphometric changes in the mandible after radiotherapy: an animal model. J Craniomaxillofac Surg 45(5):716–721. https://doi.org/10.1016/j.jcms.2017.02.014
Peng H, Chen BB, Chen L, Chen YP, Liu X, Tang LL, Mao YP, Li WF, Zhang Y, Lin AH, Sun Y, Ma J (2017) A network meta-analysis in comparing prophylactic treatments of radiotherapy-induced oral mucositis for patients with head and neck cancers receiving radiotherapy. Oral Oncol 75:89–94. https://doi.org/10.1016/j.oraloncology.2017.11.001
Sroussi HY, Epstein JB, Bensadoun RJ, Saunders DP, Lalla RV, Migliorati CA, Heaivilina N, Zumsteg ZS (2017) Common oral complications of head and neck cancer radiation therapy: mucositis, infections, saliva change, fibrosis, sensory dysfunctions, dental caries, periodontal disease, and osteoradionecrosis. Oral Complications of Radiation Therapy Cancer Medicine 6(12):2918–2931. https://doi.org/10.1002/cam4.1221
Acauan MD, Gomes APN, Braga-Filho A, de Figueiredo MAZ, Cherubini K, Salum FG (2015) Effect of low-level laser therapy on irradiated parotid glands—study in mice. J Biomed Opt 20(10):108002. https://doi.org/10.1117/1.jbo.20.10.108002
Gonnelli FAS, Palma LF, Giordani AJ, Deboni ALS, Dias RS, Segreto RA et al (2016) Low-level laser therapy for the prevention of low salivary flow rate after radiotherapy and chemotherapy in patients with head and neck cancer. Radiol Bras 49(2):86–91. https://doi.org/10.1590/0100-3984.2014.0144
Weber JB, Pinheiro AL, de Oliveira MG, Oliveira FA, Ramalho LM (2006) Laser therapy improves healing of bone defects submitted to autologous bone graft. Photomed Laser Surg 24:38–44. https://doi.org/10.1089/pho.2006.24.38
Vázquez MB, Santillán-Díaz G, González-Pérez M, Gallego-Izquierdo T, Pecos-Martín D, Plaza-Manzano G, Romero-Franco N (2015) Low power laser stimulation of the bone consolidation in tibial fractures of rats: a radiologic and histopathological analysis. Lasers Med Sci 30(1):333–338. https://doi.org/10.1007/s10103-014-1673-6
Almeida JM, de Moraes RO, Gusman DJ, Faleiros PL, Nagata MJ, Garcia VG, Theodoro LH, Bosco AF (2017) Influence of low-level laser therapy on the healing process of autogenous bone block grafts in the jaws of systemically nicotine-modified rats: a histomorphometric study. Arch Oral Biol 75:21–30. https://doi.org/10.1016/j.archoralbio.2016.12.003
Cunha SSD, Sarmento VA, Ramalho LMP (2007) Effects of radiotherapy on bone tissue. Radiol Bras 40:189–192. https://doi.org/10.1590/s0100-39842007000300011
Britz HM, Jokihaara J, Leppanen OV, Jarvinen T, Cooper DML (2010) 3D visualization and quantification of rat cortical bone porosity using a desktop micro-CT system: a case study in the tibia. J Microsc 1–6. https://doi.org/10.1111/j.1365-2818.2010.03381.x
Hsu JT, Ying-Ju C, Jung-Ting H, Heng-Li H, Shun-Ping W, Fu-Chou C, Jay W, Ming-Tzu T (2014) A comparison of micro-CT and dental CT in assessing cortical bone morphology and trabecular bone microarchitecture. PLOS ONE, Issue 9. https://doi.org/10.1371/journal.pone.0107545
Rao NJ, Jing YW, Ru QY, Yiu YL, Li WZ (2017) Role of periapical diseases in medication-related osteonecrosis of the jaws. Biomed Res Int 2017. https://doi.org/10.1155/2017/1560175
Auersvald CM, Santos FR, Nakano MM, Leoni GB, Neto MDS, Scariot R, Giovanini AF, Deliberador TM (2017) The local administration of parathyroid hormone encourages the healing of bone defects in the rat calvaria: micro-computed tomography, histological and histomorphometric evaluation. Arch Oral Biol 79(2017):14–19. https://doi.org/10.1016/j.archoralbio.2017.02.016
Pires PM, Santos TP, Gonçalves AF, Pithon MM, Lopes RT, Neves AA (2018) A dual energy micro-CT methodology for visualization and quantification of biofilm formation and dentin demineralization. Arch Oral Biol 85:10–15. https://doi.org/10.1016/j.archoralbio.2017.09.034
Krueger GF, de Oliveira MC, Gassen HT, Sganzerla JT, Simon D, Grivicich I, Quevedo Miguens, SA (2020). Evaluation of aquaporins 1 and 5 expression in rat parotid glands after volumetric modulated arc radiotherapy and use of low-level laser therapy at different times. J Lasers Med Sci 11(3):262–267. https://doi.org/10.34172/jlms.2020.44
Yanaguizawa MS, Suzuki SS, Martinez EF, Suzuki H, Pelegrin MC, Garcez AS (2017) Effects of low-level laser therapy in orthodontic patients on immediate inflammatory response after mini-implants insertion: a preliminary report. Photomed Laser Surg 35(1):57–63. https://doi.org/10.1089/pho.2015.3959
Farhadi F, Eslami H, Majidi A, Fakhrzadeh V, Ghanizadeh M, KhademNeghad S (2017). Evaluation of adjunctive effect of low-level laser therapy on pain, swelling and trismus after surgical removal of impacted lower third molar: a double blind randomized clinical trial. Laser Ther 30;26(3): 181–187. https://doi.org/10.5978/islsm.17-OR-13
Abramoff MMF, Pereira MD, Alves MTS, Segreto RA, Guilherme A, Ferreira ML (2014). Low-level laser therapy on bone repair of rat tibiae exposed to ionizing radiation. Photomed Laser Surg 32(11). https://doi.org/10.1089/pho.2013.3692
Batista JD, Zanetta-Barbosa D, Cardoso SV, Dechichi P, Rocha FS, Pagnoncelli RM (2014) Effect of low-level laser therapy on repair of the bone compromised by radiotherapy. Lasers Med Sci 29(6):1913–1918. https://doi.org/10.1007/s10103-014-1602-8
Batista DJ, Sargenti-Neto S, Dechichi P, Rocha FS, Pagnoncelli RM (2015) Low-level laser therapy on bone repair: is there any effect outside the irradiated field? Lasers Med Sci 30(5):1569–1574. https://doi.org/10.1007/s10103-015-1752-3
Santinoni CD, Oliveira HF, Batista VE, Lemos CA, Verri FR (2017) Influence of low-level laser therapy on the healing of human bone maxillofacial defects: a systematic review. J Photochem Photobiol 169:83–89. https://doi.org/10.1016/j.jphotobiol.2017.03.004
Skondra FG, Koletsi D, Eliades T, Farmakis ET (2017) The effect of low level laser therapy on bone healing after rapid maxillary expansion: a systematic review. Photomed Laser Surg 36(2):61–71. https://doi.org/10.1089/pho.2017.4278
Garavello-Freitas I, Baranauskas V, Joazeiro PP, Padovani CR, Dal Pai-Silva M, da Cruz-Höfling MA (2003) Low-power laser irradiation improves histomorphometrical parameters and bone matrix organization during tibia wound healing in rats. J Photochem Photobiol B 70:81–89
Pinheiro AL (2009) Advances and perspectives on tissue repair and healing. Photomed Laser Surg 27:833–836. https://doi.org/10.1016/S1011-1344(03)00058-7
Pinheiro AL, Gerbi ME (2006) Photoengineering of bone repair processes. Photomed Laser Surg 24:169–178. https://doi.org/10.1089/pho.2006.24.169
Silva RV, Camilli JA (2006) Repair of bone defects treated with autogenous bone graft and low-power laser. J Craniofac Surg 17(297–301):30. https://doi.org/10.1097/00001665-200603000-00017
Karu T (1989) Laser biostimulation: a photobiological phenomenon. J Photochem Photobiol B 3:638–640. https://doi.org/10.1016/1011-1344(89)80088-0
Saito S, Shimizu N (1997) Stimulatory effects of low-power laser irradiation on bone regeneration in midpalatal suture during expansion in the rat. Am J Orthod Dentofacial Orthop 111:525–532. https://doi.org/10.1016/S0889-5406(97)70152-5
Gestel DV, Weyngaert DVD, Schrijvers D, Weyler J, Vermorken JB (2011) Intensity-modulated radiotherapy in patients with head and neck cancer: a European single-centre experience. The British J of Radiol 84:367–374. https://doi.org/10.1259/bjr/67058055
Veldeman L, Madani I, Hulstaert F, De Meerleer G, Mareel M, De Neve W (2008) Evidence behind use of intensity modulated radiotherapy: a systematic review of comparative clinical studies. Lancet Oncol 9:367–375. https://doi.org/10.1016/S1470-2045(08)70098-6
Zhang WZ, Lu JY, Chen JZ, Huang ZTT, BT, Li DR, Chen CZ, (2016) A dosimetric study of using fixed-jaw volumetric modulated arc therapy for the treatment of nasopharyngeal carcinoma with cervical lymph node metastasis. PLoS ONE 11(5):e0156675. https://doi.org/10.1371/journal.pone.0156675
Lerouxel E, Moreau A, Bouler JM, Giumelli B, Daculsi G, Weiss P, Malard O (2009) Effects of high doses of ionising radiation on bone in rats: a new model for evaluation of bone engineering. Br J Oral Maxillofac Surg 47:602–607. https://doi.org/10.1016/j.bjoms.2008.12.011
Jegoux F, Malard O, Goyenvalle E, Aguado E, Daculsi G (2010) Radiation effects on bone healing and reconstruction: interpretation of the literature. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology 109(2):173–184. https://doi.org/10.1016/j.tripleo.2009.10.001
Parsa A, Ibrahim N, Hassan B, van der Stelt P, Wismeijer D (2015) CT bone quality assessment at implant site. Bone quality evaluation at dental implant site using multislice CT, micro-CT, and cone beam CT. Clin Oral Impl Res 26:1–7. https://doi.org/10.1111/clr.12315
Michel G, Blery P, Pilet P, Guicheux J, Weiss P, Malard O, Espitalier F (2015) Micro-CT analysis of radiation-induced osteopenia and bone hypovascularization in rat. Calcif Tissue Int 97(1):62–68. https://doi.org/10.1007/s00223-015-0010-9
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Meller, S.N., de Oliveira, M.C., Krueger, G.F. et al. Micro-CT analysis of the mandibular bone microarchitecture of rats after radiotherapy and low-power laser therapy. Lasers Med Sci 37, 2645–2653 (2022). https://doi.org/10.1007/s10103-022-03532-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-022-03532-0