Abstract
The primary goal of this systematic review article was to provide an outline of the use of diabetic autologous adipose-derived mesenchymal stem cells (DAAD-MSCs) in the treatment of wounds and ulcers in animal models and patients with diabetes mellitus (DM). The secondary goal was to present the outcomes of pretreatment of diabetic adipose-derived mesenchymal stem cells (DAD-MSCs) with probable different agents in the treatment of diabetic foot ulcers (DFUs) and wounds. In view of possible clinical applications of AD-MSC-mediated cell therapy for DFUs, it is essential to evaluate the influence of DM on AD-MSC functions. Nevertheless, there are conflicting results about the effects of DAAD-MSCs on accelerating wound healing in animals and DM patients. Multistep research of the MEDLINE, PubMed, Embase, Clinicaltrials.gov, Scopus database, and Cochrane databases was conducted for abstracts and full-text scientific papers published between 2000 and 2020. Finally, 5 articles confirmed that the usage of allogeneic or autologous AD-MSCs had encouraging outcomes on diabetic wound healing. One study reported that DM changes AD-MSC function and therapeutic potential, and one article recommended that the pretreatment of diabetic allogeneic adipose-derived mesenchymal stem cells (DAlD-MSCs) was more effective in accelerating diabetic wound healing. Recently, much work has concentrated on evolving innovative healing tactics for hastening the repair of DFUs. While DM alters the intrinsic properties of AD-MSCs and impairs their function, one animal study showed that the pretreatment of DAlD-MSCs in vitro significantly increased the function of DAlD-MSCs compared with DAlD-MSCs without any treatment. Preconditioning diabetic AD-MSCs with pretreatment agents like photobiomodulation (PBM) significantly hastened healing in delayed-healing wounds. It is suggested that further animal and human studies be conducted in order to provide more documentation. Hopefully, these outcomes will help the use of DAAD-MSCs plus PBM as a routine treatment protocol for healing severe DFUs in DM patients.

Similar content being viewed by others
Data availability
Since our work was a systematic review article without any statistical analysis requirement, we added a full text of the final approved articles which were evaluated in this work.
Abbreviations
- DM:
-
Diabetes mellitus
- DFU:
-
Diabetic foot ulcer
- MSC:
-
Mesenchymal stem cell
- AAD-MSC:
-
Autologous adipose-derived mesenchymal stem cells
- AD-MSC:
-
Adipose-derived mesenchymal stem cells
- DAAD-MSC:
-
Diabetic autologous adipose-derived mesenchymal stem cells
- VEGF:
-
Vascular endothelial growth factor
- TGF-β:
-
Transforming growth factor-beta
- Ga-Al-As:
-
Gallium-aluminum-arsenide laser
- h:
-
Human
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- STZ:
-
Streptozotocin
- DM1:
-
Type 1 diabetic
- scCO2 :
-
Supercritical carbon dioxide
- ADM:
-
Acellular dermal matrix
- CLI:
-
Critical limb ischemia
- PBM:
-
Photobiomodulation
- DAlD-MSCs:
-
Diabetic allogeneic adipose-derived stem cell
- i.p.:
-
Intraperitoneal
- CD:
-
Cluster of differentiation
- MTT:
-
3-[4,5-dimethylthiazol-2-yl]-2,5 diphenyl tetrazolium bromide assay
- PDT:
-
Population doubling time
- DM2:
-
Type 2 DM
- TLRs:
-
Toll-like receptors
- IL-1R1:
-
IL-1 receptors, type 1
- bFGF:
-
Basic fibroblast growth factor
- LLLT:
-
Low-level laser therapy
References
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE, Bright D, Williams R (2019) Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition, Diabetes. Res Clin Pract 157 107843
Patel S, Srivastava S, Singh MR, Singh D (2019) Mechanistic insight into diabetic wounds: pathogenesis, molecular targets and treatment strategies to pace wound healing. Biomed Pharmacother 112 108615
Amin N, Doupis J (2016) Diabetic foot disease: From the evaluation of the “foot at risk” to the novel diabetic ulcer treatment modalities, World. J Diabetes 7:153–164
Dormandy J, Heeck L, Vig S (1999) Major amputations: clinical patterns and predictors, in: Seminars in vascular surgery. 154–161
Moulik PK, Mtonga R, Gill GV (2003) Amputation and mortality in new-onset diabetic foot ulcers stratified by etiology. Diabet Care 26:491–494
Rice JB, Desai U, Cummings AK, Birnbaum HG, Skornicki M, Parsons NB (2014) Burden of diabetic foot ulcers for medicare and private insurers. Diabet Care 37:651–658
Everett E, Mathioudakis N (2018) Update on management of diabetic foot ulcers. Ann N Y Acad Sci 1411:153
Wang M, Yuan Q, Xie L (2018) Mesenchymal stem cell-based immunomodulation: properties and clinical application. Stem Cells Int 2018:3057624
Xu Y-X, Chen L, Wang R, Hou W-K, Lin P, Sun L, Sun Y, Dong Q-Y (2008) Mesenchymal stem cell therapy for diabetes through paracrine mechanisms. Med Hypotheses 71:390–393
TrojahnKølle S-F, Oliveri RS, Glovinski PV, Elberg JJ, Fischer-Nielsen A, Drzewiecki KT (2012) Importance of mesenchymal stem cells in autologous fat grafting: a systematic review of existing studies. J Plast Surg Hand Surg 46:59–68
Lopes L, Setia O, Aurshina A, Liu S, Hu H, Isaji T, Liu H, Wang T, Ono S, Guo X (2018) Stem cell therapy for diabetic foot ulcers: a review of preclinical and clinical research. Stem Cell Res Ther 9:188
Chu DT, Nguyen Thi Phuong T, Tien NLB, Tran DK, Minh LB, Thanh VV, Gia Anh P, Pham VH, Thi Nga V (2019) Adipose tissue stem cells for therapy: an update on the progress of isolation, culture, storage, and clinical application. J Clin Med 8
Zografou A, Papadopoulos O, Tsigris C, Kavantzas N, Michalopoulos E, Chatzistamatiou T, Papassavas A, Stavropoulou-Gioka C, Dontas I, Perrea D (2013) Autologous transplantation of adipose-derived stem cells enhances skin graft survival and wound healing in diabetic rats. Ann Plast Surg 71:225–232
Álvaro-Afonso FJ, Sanz-Corbalán I, Lázaro-Martínez JL, Kakagia D, Papanas N (2020) Adipose-derived mesenchymal stem cells in the treatment of diabetic foot ulcers: a review of preclinical and clinical studies. Angiology 71:853–863
Rennert RC, Sorkin M, Januszyk M, Duscher D, Kosaraju R, Chung MT, Lennon J, Radiya-Dixit A, Raghvendra S, Maan ZN (2014) Diabetes impairs the angiogenic potential of adipose-derived stem cells by selectively depleting cellular subpopulations. Stem Cell Res Ther 5:79
Cerqueira MT, Pirraco RP, Marques AP (2016) Stem cells in skin wound healing: are we there yet? Adv Wound Care 5:164–175
van de Vyver M (2017) Intrinsic mesenchymal stem cell dysfunction in diabetes mellitus: implications for autologous cell therapy. Stem Cells Dev 26:1042–1053
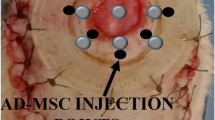
Ahmadi H, Amini A, Fathabady FF, Mostafavinia A, Zare F, Ebrahimpour-Malekshah R, Ghalibaf MN, Abrisham M, Rezaei F, Albright R (2020) Transplantation of photobiomodulation-preconditioned diabetic stem cells accelerates ischemic wound healing in diabetic rats. Stem Cell Res Ther 11:1–14
Khosravipour A, Amini A, MasteriFarahani R, Zare F, Mostafavinia A, Fallahnezhad S, Akbarzade S, Ava P, Asgari M, Mohammadbeigi A, Rezaei F, Ghoreishi SK, Chien S, Bayat M (2020) Preconditioning adipose-derived stem cells with photobiomodulation significantly increased bone healing in a critical size femoral defect in rats. Biochem Biophys Res Commun 531:105–111
Zare F, Moradi A, Fallahnezhad S, Ghoreishi SK, Amini A, Chien S, Bayat M (2019) Photobiomodulation with 630 plus 810 nm wavelengths induce more in vitro cell viability of human adipose stem cells than human bone marrow-derived stem cells. J Photochem Photobiol B Biol 201 111658
Kushibiki T, Hirasawa T, Okawa S, Ishihara M (2015) Low reactive level laser therapy for mesenchymal stromal cells therapies. Stem Cells Int 2015
Min KH, Byun JH, Heo CY, Kim EH, Choi HY, Pak CS (2015) Effect of low-level laser therapy on human adipose-derived stem cells: in vitro and in vivo studies. Aesthetic Plast Surg 39:778–782
Heo CY, Yoon YS, Min KH, Nam SY, Lee KS, Shin BH, Lee S, Lee M Effects of low-level laser therapy and adipose-derived stem cells on the viability of autologous fat grafts: a preliminary study. Arch Aesthetic Plast Surg 27 81–87
Cianfarani F, Toietta G, Di Rocco G, Cesareo E, Zambruno G, Odorisio T (2013) Diabetes impairs adipose tissue-derived stem cell function and efficiency in promoting wound healing. Wound Repair Regen 21:545–553
Nambu M, Ishihara M, Kishimoto S, Yanagibayashi S, Yamamoto N, Azuma R, Kanatani Y, Kiyosawa T, Mizuno H (2011) Stimulatory effect of autologous adipose tissue-derived stromal cells in an atelocollagen matrix on wound healing in diabetic db/db mice. J Tissue Eng 2011
Chou P-R, Lin Y-N, Wu S-H, Lin S-D, Srinivasan P, Hsieh D-J, Huang S-H (2020) Supercritical carbon dioxide-decellularized porcine acellular dermal matrix combined with autologous adipose-derived stem cells: its role in accelerated diabetic wound healing. Int J Med Sci 17:354
Marino G, Moraci M, Armenia E, Orabona C, Sergio R, De Sena G, Capuozzo V, Barbarisi M, Rosso F, Giordano G, Iovino F, Barbarisi A (2013) Therapy with autologous adipose-derived regenerative cells for the care of chronic ulcer of lower limbs in patients with peripheral arterial disease. J Surg Res 185:36–44
Bura A, Planat-Benard V, Bourin P, Silvestre J-S, Gross F, Grolleau J-L, Saint-Lebese B, Peyrafitte J-A, Fleury S, Gadelorge M (2014) Phase I trial: the use of autologous cultured adipose-derived stroma/stem cells to treat patients with non-revascularizable critical limb ischemia. Cytotherapy 16:245–257
Bura A, Planat-Benard V, Bourin P, Silvestre JS, Gross F, Grolleau JL, Saint-Lebese B, Peyrafitte JA, Fleury S, Gadelorge M, Taurand M, Dupuis-Coronas S, Leobon B, Casteilla L (2014) Phase I trial: the use of autologous cultured adipose-derived stroma/stem cells to treat patients with non-revascularizable critical limb ischemia. Cytotherapy 16:245–257
Jumabay M, Moon JH, Yeerna H, Boström KI (2015) Effect of diabetes mellitus on adipocyte-derived stem cells in rat. J Cell Physiol 230:2821–2828
An R, Zhang Y, Qiao Y, Song L, Wang H, Dong X (2020) Adipose stem cells isolated from diabetic mice improve cutaneous wound healing in streptozotocin-induced diabetic mice. Stem Cell Res Ther 11:1–11
Marino G, Moraci M, Armenia E, Orabona C, Sergio R, De Sena G, Capuozzo V, Barbarisi M, Rosso F, Giordano G (2013) Therapy with autologous adipose-derived regenerative cells for the care of chronic ulcer of lower limbs in patients with peripheral arterial disease. J Surg Res 185:36–44
Sumi M, Sata M, Toya N, Yanaga K, Ohki T, Nagai R (2007) Transplantation of adipose stromal cells, but not mature adipocytes, augments ischemia-induced angiogenesis. Life Sci 80:559–565
Harada Y, Yamamoto Y, Tsujimoto S, Matsugami H, Yoshida A, Hisatome I (2013) Transplantation of freshly isolated adipose tissue-derived regenerative cells enhances angiogenesis in a murine model of hind limb ischemia. Biomed Res 34:23–29
Li X, Xie X, Lian W, Shi R, Han S, Zhang H, Lu L, Li M (2018) Exosomes from adipose-derived stem cells overexpressing Nrf2 accelerate cutaneous wound healing by promoting vascularization in a diabetic foot ulcer rat model. Exp Mol Med 50:1–14
Gadelkarim M, Abushouk AI, Ghanem E, Hamaad AM, Saad AM, Abdel-Daim MM (2018) Adipose-derived stem cells: effectiveness and advances in delivery in diabetic wound healing. Biomed Pharmacother 107:625–633
Burdon TJ, Paul A, Noiseux N, Prakash S, Shum-Tim D (2011) Bone marrow stem cell derived paracrine factors for regenerative medicine: current perspectives and therapeutic potential, Bone marrow research, 2011
Zhang H, Hou JF, Shen Y, Wang W, Wei YJ, Hu S (2010) Low level laser irradiation precondition to create friendly milieu of infarcted myocardium and enhance early survival of transplanted bone marrow cells. JCell Mol Med 14:1975–1987
Furman BL (2015) Streptozotocin-induced diabetic models in mice and rats.Curr Prot Pharmacol 70 5.47. 41–45.47. 20
Boulton AJ (2008) The diabetic foot, in: Controversies in treating diabetes, Springer, pp. 251–267
Moradi A, Zare F, Mostafavinia A, Safaju S, Shahbazi A, Habibi M, Abdollahifar M-A, Hashemi SM, Amini A, Ghoreishi SK (2020) Photobiomodulation plus adipose-derived stem cells improve healing of ischemic infected wounds in type 2 diabetic rats. Sci Rep 10:1–15
Karina K, Rosliana I, Sobariah S, Rosadi I, Afini I, Widyastuti T, Remelia M, Sukmawati D, Pawitan JA (2019) Diabetes mellitus type 2 reduces the viability, proliferation, and angiogenic marker of adipose-derived stem cells cultured in low-glucose anti-oxidant-serum supplemented medium. Biomed Res Ther 6:3073–3082
Shin L, Peterson DA (2012) Impaired therapeutic capacity of autologous stem cells in a model of type 2 diabetes. Stem Cells Transl Med 1:125–135
Abdi J, Rashedi I, Keating A (2018) Concise review: TLR pathway-miRNA interplay in mesenchymal stromal cells: regulatory roles and therapeutic directions. Stem cells 36:1655–1662
Pugin J (2012) How tissue injury alarms the immune system and causes a systemic inflammatory response syndrome. Ann Intensive Care 2:27
Zampell JC, Yan A, Avraham T, Andrade V, Malliaris S, Aschen S, Rockson SG, Mehrara BJ (2011) Temporal and spatial patterns of endogenous danger signal expression after wound healing and in response to lymphedema, American Journal of Physiology-Cell. Physiology 300:C1107–C1121
Basith S, Manavalan B, Yoo TH, Kim SG, Choi S (2012) Roles of toll-like receptors in cancer: a double-edged sword for defense and offense. Arch Pharmacal Res 35:1297–1316
Julier Z, Park AJ, Briquez PS, Martino MM (2017) Promoting tissue regeneration by modulating the immune system. Acta Biomater 53:13–28
Martino MM, Maruyama K, Kuhn GA, Satoh T, Takeuchi O, Müller R, Akira S (2016) Inhibition of IL-1R1/MyD88 signalling promotes mesenchymal stem cell-driven tissue regeneration. Nat Commun 7:11051
Lin W, Xu L, Zwingenberger S, Gibon E, Goodman SB, Li G (2017) Mesenchymal stem cells homing to improve bone healing. J Orthopaedic Trans 9:19–27
Lee EY, Xia Y, Kim WS, Kim MH, Kim TH, Kim KJ, Park BS, Sung JH (2009) Hypoxia-enhanced wound-healing function of adipose-derived stem cells: increase in stem cell proliferation and up-regulation of VEGF and bFGF. Wound Repair Regen 17:540–547
Avci P, Gupta A, Sadasivam M, Vecchio D, Pam Z, Pam N, Hamblin MR (2013) Low-level laser (light) therapy (LLLT) in skin: stimulating, healing, restoring. Semin Cutan Med Surg 32:41–52
Fridoni M, Kouhkheil R, Abdollhifar MA, Amini A, Ghatrehsamani M, Ghoreishi SK, Chien S, Bayat S, Bayat M (2019) Improvement in infected wound healing in type 1 diabetic rat by the synergistic effect of photobiomodulation therapy and conditioned medium. J Cell Biochem 120:9906–9916
Amini A, Pouriran R, Abdollahifar MA, Abbaszadeh HA, Ghoreishi SK, Chien S, Bayat M (2018) Stereological and molecular studies on the combined effects of photobiomodulation and human bone marrow mesenchymal stem cell conditioned medium on wound healing in diabetic rats. J Photochem Photobiol B 182:42–51
Ebrahimpour-Malekshah R, Amini A, Zare F, Mostafavinia A, Davoody S, Deravi N, Rahmanian M, Hashemi SM, Habibi M, Ghoreishi SK, Chien S, Shafikhani S, Ahmadi H, Bayat S, Bayat M (2020) Combined therapy of photobiomodulation and adipose-derived stem cells synergistically improve healing in an ischemic, infected and delayed healing wound model in rats with type 1 diabetes mellitus. BMJ Open Diabet Res Care 8
Ahmadi H, Amini A, FadaeiFathabady F, Mostafavinia A, Zare F, Ebrahimpour-Malekshah R, Ghalibaf MN, Abrisham M, Rezaei F, Albright R, Ghoreishi SK, Chien S, Bayat M (2020) Transplantation of photobiomodulation-preconditioned diabetic stem cells accelerates ischemic wound healing in diabetic rats. Stem Cell Res Ther 11 494
Author information
Authors and Affiliations
Contributions
AA, MB, and SC gathered data, AA wrote the first draft, MB and SC edited it, and MB submitted it to the journal.
Corresponding authors
Ethics declarations
Ethics approval
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Amini, A., Chien, S. & Bayat, M. Effectiveness of preconditioned adipose-derived mesenchymal stem cells with photobiomodulation for the treatment of diabetic foot ulcers: a systematic review. Lasers Med Sci 37, 1415–1425 (2022). https://doi.org/10.1007/s10103-021-03451-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-021-03451-6