Abstract
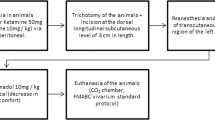
The reconstructive techniques have been widely used in Veterinary Medicine. The post-operative adjuvants therapies like the low-level laser therapy (LLLT) are used to decrease inherent complications to reconstructive surgeries. This article purposed to define the LLLT effects on the healing, inflammation, and vascularization of the skin grafts in applicable time intervals to veterinary surgical routine. Forty rats (Rattus norvegicus albinus wistar) were used and each one was submitted to autogenous cutaneous mesh grafting in the interescapular region. The rats were randomly distributed in five groups (G1, G2, G3, G4, and G5) in accordance with the 6 J/cm2 or 10 J/cm2 dose every 3 or 5 days. These treatments were applied on the skin graft for 15 days. The histochemical evaluation with Picrosirius showed greater expression of collagen type 1 – red in grafts of G5 (p < 0.05), while in G1 did not; the expression of collagen type III – green was not induced by LLLT. The histochemical evaluation with hematoxylin-eosin showed greater numbers of fibroblasts in grafts of G4 (p < 0.05) and less hemorrhage in grafts of G5 (p < 0.05). There was modulation of the inflammatory response in irradiated skin grafts. It is concluded the exhibition of the skin grafts to 6 J/cm2 or 10 J/cm2 dose every 5 days improved the healing and the modulation of the local inflammation.



Similar content being viewed by others
References
Amsellen P (2011) Complications of reconstructive surgery in companion animals. Vet Clin Small Anim 41:995–1006. https://doi.org/10.1016/j.cvsm.2011.05.005
Martins MIM, Elias BC, Justino RC, Hilst CLS (2015) Cirurgia reconstrutiva com retalho cutâneo de avanço como técnica alternativa para tratamento de carcinoma de células escamosas em cães: relato de caso. Revista Brasileira de Ciência Veterinária 22:131–136. https://doi.org/10.4322/rbcv.2016.001
Stanley BJ, Pitt KA, Weder CD, Fritz MC, Hauptman JG, Steficek BA (2013) Effects of negative pressure wound therapy on lealing of free full-thickness skin grafts in dogs. Vet Surg 42:511–522. https://doi.org/10.1111/j.1532-950X.2013.12005.x
Montinaro V (2014) Lateral caudal axial pattern flap in 13 dogs. Vet Surg 9999:1–6. https://doi.org/10.1111/j.1532-950X.2014.12305.x
Audrain H, Bray A, De Berker D (2015) Full-thickness skin grafts for lower leg defects: na effective repair option. Dermatol Surgery 41:493–498. https://doi.org/10.1097/DSS.0000000000000330
Pazzini JM, Moraes PC (2015) Princípios e técnicas para realização de enxertos cutâneos. In: Castro JL, De Nardi AB, Huppes RR, Pazzini JM (eds) Princípios e técnicas de cirurgias reconstrutivas da pele de cães e gatos (atlas colorido), 1rd edn. Medvep, Curitiba, pp 95–102
Isaac C, Ladeira PRS, Rêgo FMP, Aldunate JCB, Ferreira MC (2010) Processo de cura das feridas: cicatrização fisiológica. Rev Med 89:125–131. https://doi.org/10.11606/issn.1679-9836.v89i3/4p125-131
Kazemikhoo N et al (2018) Evaluation of the effects of low level laser therapy on the healing process after skin graft surgery in burned patients (a randomized clinical trial). J Lasers Med Sci 9:139–143. https://doi.org/10.15171/jlms.2018.26
Samaneh R, Ali Y, Mostafa J, Mahmud NA, Zohre R (2015) Laser therapy for wound healing: a review of currrent techniques and mechanisms of action. Biosci Biotechnol Res Asia 12:217–223. https://doi.org/10.13005/bbra/162610
Silva IHM, Andrade SC, Faria ABS, Fonsêca DDD, Gueiros LAM et al (2016) Increase in the nitric oxide release without changes in cell viability of macrophages after laser therapy with 660 and 808 nm lasers. Lasers Med Sci 31:1855–1862. https://doi.org/10.1007/s10103-016-2061-1
Ramos FS, Maifrino LBM, Alves S, Alves BCA, Perez MM, Feder D, Azzalis LA et al (2018) The effects of tanscutaneous low-level laser therapy on the skin healing process: an experimental model. Lasers Med Sci 33:967–976. https://doi.org/10.1007/s10103-017-2429-x
Busnardo VL, Biondo-Simões MLPB (2010) Os efeitos do laser hélio-neônio de baixa intensidade na cicatrização de lesões cutâneas induzidas em ratos. Rev Bras Fis 14:45–51. https://doi.org/10.1590/S1413-35552010000100008
Chaves MEA, Araújo AR, Piancastelli ACC, Pinotti M (2014) Effects of low-power light therapy on wound healing: Laser X Led. Anais Brasileiros de Bras DDermatologia 89:616–623. https://doi.org/10.1590/abd1806-4841.20142519
Farivar S, Malekshahabi T, Shiari R (2014) Biological effects of low level laser therapy. Journal of Lasers in Medical Sciences 5:58–62
Loreti EH, Pascoal VLW, Nogueira BV, Silva IV, Pedrosa DF (2015) Use of laser therapy in the healing process: a literature review. Photomed Laser Surg 33:104–116. https://doi.org/10.1089/pho.2014.3772
Cury V, Moretti AIS, Assis L, Bossini CJS, Benatti Neto C, Fangel R et al (2013) Low level laser therapy increases angiogenesis in a model of ischemic skin flap in rats mediated by VEGF, HIF-1α and MMP-2. J of Photochem Photobiol 125:164–170. https://doi.org/10.1016/j.jphotobiol.2013.06.004
Hawkins D, Abrahamse H (2005) Biological effects of helium-neon laser irradiation on normal and wounded human skin fibroblastos. Photomed Laser Surg 23:251–259. https://doi.org/10.1089/pho.2005.23.251
Andrade FSSD, Clark RMO, Ferreira ML (2014) Efeitos da laserterapia de baixa potência na cicatrização de feridas cutâneas. Revista do Colégio Brasileiro de Cirurgia 41:129–133. https://doi.org/10.1590/S0100-69912014000200010
Fiório FB, Albertini R, Leal-Júnior ECP, Carvalho PTC (2013) Effect of low-level laser therapy on types I and III colagen and inflammatory cells in rats with induced third-degree burns. Lasers Med Sci 29:313–319. https://doi.org/10.1007/s10103-013-1341-2
Mathur RK, Sahu K, Saraf S, Patheja P, Khan F, Gupta PK (2016) Low-level laser therapy as na adjunct to conventional therapy in the treatment of diabetic foot ulcers. Lasers Med Sci 32:275–282. https://doi.org/10.1007/s10103-016-2109-2
Brassolatti P, Bossini PS, Oliveira MCD, Kido HW, Tim CR, Almeida-Lopes L, De Avó LRS et al (2016) Comparative effects of two different doses of low-level laser therapy on wound healing third-degree burns in rats. Microsc Res Tech 79:313–320. https://doi.org/10.1002/jemt.22632
Almeida JM, Moraes RO, Gusman DJR, Faleiros PL, Nagata MJH, Garcia VG, Theodoro LH, Bosco AF (2017) Influence of low-level laser therapy on the healing process of autogenous boné block grafts in the jaws of systemically nicotine-modified rats: a histomorphometric study. Arch Oral Biol 75:21–30. https://doi.org/10.1016/j.archoralbio.2016.12.003
Bedoya SAO, Conceição LG, Viloria MIV, Loures FH, Valenta FL, Amorim RL, Silva FF (2016) Caracterização de colágenos tipos I e III no estroma do carcinoma de células escamosas cutâneo em cães. Arquivo Brasileiro de Medicina Veterinária e Zootecnia 68:147–154. https://doi.org/10.1590/1678-4162-8484
Fortuna T, Gonzalez AC, Sá MF, Andrade ZA, Reis SRA, Medrado ARAP (2017) Effect of 670 nm laser photobiomodulation on vascular density and fibroplasia in late stages of tissue repair. Int Wound J 15:274–282. https://doi.org/10.1111/iwj.12861
Dahmardehei M, Kazemikhoo N, Vaghardoost R, Mokmeli S, Momeni M, Nilforoushzadeh MA et al (2016) Effects of low level laser therapy on the prognosis of split-thickness skin graft in type 3 burn of diabetic patients: a case series. Lasers Med Sci 31:497–502. https://doi.org/10.1007/s10103-016-1896-9
Carvalho PTC, Silva IS, Reis FA, Pereira DM, Aydos RD (2010) Influence of ingaalp laser (660 nm) on the healing of skin wounds in diabetic rats. Acta Cir Bras 25:71–79. https://doi.org/10.1590/S0102-86502010000100016
Esteves Júnior I, Masson IB, Oshima CTF, Paiotti APR, Liebano RE, Plaper H (2012) Low-level laser irradiation, cyclooxygenase-2 (COX-2) expression and necrosis of random skin flaps in rats. Lasers Med Sci 27:655–660. https://doi.org/10.1007/s10103-011-1011-1
Renno ACM, Iwama AM, Shima P, Fernandes KR, Carvalho JG, Oliveira P, Ribeiro DA (2011) Effect of low-level laser therapy (660nm) on the healing of second-degree skin burns in rats. J Cosmet Laser Ther 13:237–242. https://doi.org/10.3109/14764172.2011.606466
Silva AA, Leal-Júnior ECP, Alves ACA, Rambo CS, Santos AS, Vieira RP, Carvalho PTC (2013) Wound-healing effects of low-level laser therapy in diabetic rats involve the modulation of MMP-2 and MMP-9 and the redistribution of collagen types I and III. J Cosmet Laser Ther 15:210–216. https://doi.org/10.3109/14764172.2012.761345
Medeiros ML, Araújo Filho I, Silva EMN, Queiroz WSS, Soares CD, Carvalho MGF, Maciel MAM (2017) Effect of low-level laser therapy on angiogenesis and matrix metalloproteinase-2 immunoexpression in wound repair. Lasers Med Sci 32:35–43. https://doi.org/10.1007/s10103-016-2080-y
Medrado ARAP, Pugliese LS, Reis SRA, Andrade ZA (2003) Influence of low level laser therapy on wound healing and its biological action upon myofibroblasts. Lasers Surg Med 32:293–244. https://doi.org/10.1002/lsm.10126
Garcia VG, Macarini VC, Almeida JM, Bosco AF, Nagata MJ, Okamoto T, Longo M et al (2012) Influence of low-level laser therapy on wound healing in nicotine-treated animals. Lasers Med Sci 27:437–443. https://doi.org/10.1007/s10103-011-0956-4
Funding
This study was funded by São Paulo Research Foundation (FAPESP) research fellowship to Moreira SH (Protocol 2017/25951-9).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study followed the guidelines of the Animal Experimentation Code of Ethics of the Brazilian College of Animal Experimentation and was approved by the Ethics Committee of Animals Use (CEUA) from FCAV, Unesp (Protocol 010401/17).
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Moreira, S.H., Pazzini, J.M., Álvarez, J.L.G. et al. Evaluation of angiogenesis, inflammation, and healing on irradiated skin graft with low-level laser therapy in rats (Rattus norvegicus albinus wistar). Lasers Med Sci 35, 1103–1109 (2020). https://doi.org/10.1007/s10103-019-02917-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-019-02917-y