Abstract
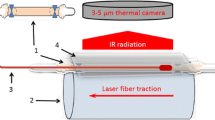
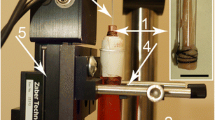
Minimally invasive treatment of varicose veins by endovenous laser ablation (EVLA) becomes more and more popular. However, despite significant research efforts performed during the last years, there is still a lack of agreement regarding EVLA mechanisms and therapeutic strategies. The aim of this article is to address some of these controversies by utilizing optical–thermal mathematical modeling. Our model combines Mordon's light absorption-based optical–thermal model with the thermal consequences of the thin carbonized blood layer on the laser fiber tip that is heated up to temperatures of around 1,000 °C due to the absorption of about 45 % of the laser light. Computations were made in MATLAB. Laser wavelengths included were 810, 840, 940, 980, 1,064, 1,320, 1,470, and 1,950 nm. We addressed (a) the effect of direct light absorption by the vein wall on temperature behavior, comparing computations by using normal and zero wall absorption; (b) the prediction of the influence of wavelength on the temperature behavior; (c) the effect of the hot carbonized blood layer surrounding the fiber tip on temperature behavior, comparing wall temperatures from using a hot fiber tip and one kept at room temperature; (d) the effect of blood emptying the vein, simulated by reducing the inside vein diameter from 3 down to 0.8 mm; (e) the contribution of absorbed light energy to the increase in total energy at the inner vein wall in the time period where the highest inner wall temperature was reached; (f) the effect of laser power and pullback velocity on wall temperature of a 2-mm inner diameter vein, at a power/velocity ratio of 30 J/cm at 1,470 nm; (g) a comparison of model outcomes and clinical findings of EVLA procedures at 810 nm, 11 W, and 1.25 mm/s, and 1,470 nm, 6 W, and 1 mm/s, respectively. Interestingly, our model predicts that the dominating mechanism for heating up the vein wall is not direct absorption of the laser light by the vein wall but, rather, heat flow to the vein wall and its subsequent temperature increase from two independent heat sources. The first is the exceedingly hot carbonized layer covering the fiber tip; the second is the hot blood surrounding the fiber tip, heated up by direct absorption of the laser light. Both mechanisms are about equally effective for all laser wavelengths. Therefore, our model concurs the finding of Vuylsteke and Mordon (Ann Vasc Surg 26:424–433, 2012) of more circumferential vein wall injury in veins (nearly) devoid of blood, but it does not support their proposed explanation of direct light absorption by the vein wall. Furthermore, EVLA appears to be a more efficient therapy by the combination of higher laser power and faster pullback velocity than by the inverse combination. Our findings suggest that 1,470 nm achieves the highest EVLA efficacy compared to the shorter wavelengths at all vein diameters considered. However, 1,950 nm of EVLA is more efficacious than 1,470 nm albeit only at very small inner vein diameters (smaller than about 1 mm, i.e., veins quite devoid of blood). Our model confirms the efficacy of both clinical procedures at 810 and 1,470 nm. In conclusion, our model simulations suggest that direct light absorption by the vein wall is relatively unimportant, despite being the supposed mechanism of action of EVLA that drove the introduction of new lasers with different wavelengths. Consequently, the presumed advantage of wavelengths targeting water rather than hemoglobin is flawed. Finally, the model predicts that EVLA therapy may be optimized by using 1,470 nm of laser light, emptying of the vein before treatment, and combining a higher laser power with a greater fiber tip pullback velocity.











Similar content being viewed by others
References
Vuylsteke ME, Mordon SR (2012) Endovenous laser ablation: a review of mechanisms of action. Ann Vasc Surg 26:424–433
Van Gemert MJC, van der Geld CWM, Bruijninckx CMA, Verdaasdonk RM, Neumann HAM (2012) Comment to Vuylsteke ME and Mordon SR. Endovenous laser ablation: a review of mechanisms of action. Ann Vasc Surg 2012;26:424–33. Ann Vasc Surg 26:881–883
Navarro L, Navarro N, Salat CB, Gomez JF, Min RJ. (2002) Endovascular laser device and treatment of varicose veins. US 6,398,777 B1 (patent filed in 1999, granted in 2002)
Mordon SR, Wassmer B, Zemmouri J (2007) Mathematical modeling of 980-nm and 1320-nm endovenous laser treatment. Lasers Surg Med 39:256–265
Welch AJ, van Gemert MJC (eds) (2011) Optical-thermal response of laser-irradiated tissue, 2nd edn. Springer, Dordrecht
van den Bos RR, Kokaert MA, Neumann HAM, Bremmer RH, Nijsten T, van Gemert MJC (2009) Heat conduction from the exceedingly hot fiber tip contributes to the endovenous laser ablation of varicose veins. Lasers Med Sci 24:247–251, Erratum Lasers Med Sci 2009;24:679
Amzayyb M, van den Bos RR, Kodach VM, de Bruin DM, Nijsten T, Neumann HAM, van Gemert MJC (2010) Carbonised blood deposited on fibers during 810, 940 and 1,470 nm endovenous laser ablation: thickness and absorption by optical coherence tomography. Lasers Med Sci 25:439–447
Proebstle TM, Lehr HA, Kargl A, Espinola-Klein C, Rother W, Bethge S, Knop J (2002) Endovenous treatment of the greater saphenous vein with a 940-nm diode laser: thrombotic occlusion after endoluminal thermal damage by laser-generated steam bubbles. J Vasc Surg 35:729–736
Disselhof BCVM, Rem AI, Verdaasdonk RM, der Kinderen DJ, Moll FL (2008) Endovenous laser ablation: an experimental study on the mechanism of action. Phlebology 23:69–76
van der Geld CWM, van den Bos RR, van Ruijven PWM, Nijsten T, Neumann HAM, van Gemert MJC (2010) The heat-pipe resembling action of boiling bubbles in endovenous laser ablation. Lasers Med Sci 25:907–909
Goldman MP, Mauricio M, Rao J (2004) Intravascular 1320-nm laser closure of the great saphenous vein: a 6- to 12-month follow-up study. Dermatol Surg 30:1380–1385
Almeida J, Mackay E, Javier J, Mauriello J, Raines J (2009) Saphenous laser ablation at 1470 nm targets the vein wall, not blood. Vasc Endovascular Surg 43:467–472
Van Ruijven PWM, Poluektova AA, van Gemert MJC, Neumann HAM, Nijsten T, van der Geld CWM (2013) Optical-thermal mathematical model for Endovenous Laser Ablation of varicose veins. Lasers Med Sci (this issue)
van den Bos RR, van Ruijven PWM, van der Geld CWM, van Gemert MJC, Neumann HAM, Nijsten T (2012) Endovenous simulated laser experiments at 940 nm and 1470 nm suggest wavelength independent temperature profiles. Eur J Vasc Endovasc Surg 44:77–81
Zonios G, Dimou A (2006) Modeling diffuse reflectance from semi-infinite turbid media: application to the study of skin optical properties. Opt Express 14:8661–8674
Lister T, Wright PA, Chappell PH (2012) Optical properties of human skin. J Biomed Opt 17:1–15, 090901
Brown JH, BJ E, West GB (1997) Allometric scaling laws in biology. Science 278:369–373
Faber DJ, Aalders MCG, Mik EG, Hooper B, van Gemert MJC, van Leeuwen TG (2004) Oxygen saturation dependent absorption and scattering of blood. Phys Rev Lett 93:1–4, 028102
Barton JK (2011) Dynamic changes in optical properties. In: Welch AJ, van Gemert MJC (eds) Optical-thermal response of laser-irradiated tissue, 2nd edn. Springer, Dordrecht, Chapter 9
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1
The mathematical formulation of the heat conduction governed by Fourier's law supplemented with appropriate boundary and initial conditions is given by the following:
with q the volumetric heat generation given by the product of absorption coefficient and fluence rate (watts per cubic meter) [2]; μ a the absorption coefficient (1/m); μ s the scattering coefficient (1/m) and g the average cosine of the scattering angle (the anisotropy factor); r fiber the fiber radius (meters); and V tip the volume of the carbonized layer (cubic meters), which thickness is about 0.1 mm and does not change during the computation. We assumed that 45 % of the light propagating towards the fiber tip is absorbed by the carbonized layer [3].
The rectangular computational domain is described by Ω = {(r,z) R2|, 0 ≤ r ≤ R, 0 ≤ z ≤ L}, where R is the radial size of the computational domain (meters), and L the axial size of the computational domain (meters).
The optical parameters such as reduced scattering coefficient, μ ' s , the optical diffusion constant, D dif, the effective attenuation coefficient, μ eff, are defined by the following:
Heat transfer due to boiling bubbles is not explicitly simulated, but it is approximately taken into account by increasing the coefficient of heat conductivity by a factor of 200 in the region where temperature exceeds the threshold of 95 °C. This approach limits the maximum temperatures of the blood to about 100 °C. This procedure assures energy conservation.
This model is discussed in detail elsewhere [13].
Appendix 2
The amount of volumetric light energy absorbed at the inner vein wall at z = 40 mm and r = r i, in the time period between t = 0 and t = t end, where t end is the time at which the inner wall temperature reaches its maximum value, E light(r i,t end) , is given by the following:
μ a (r i) is the light absorption coefficient and ϕ(r i,t) the fluence rate (watts per square meter) of the vein wall at point r i and time t and product μ a (r i)ϕ(r i,t) is the absorbed power in an infinitesimally small volume at r i, t. In the same period of time, from t = 0 to t = t end, the total volumetric increase in energy, E total(r i,t end), is given by
\( {\left.\frac{ dT}{ dt}\right|}^{+} \) indicates the positive value of the derivative, which by definition is zero if the time rate of change of T is negative. Ratio E light/E total has been computed for all wavelengths and vein diameters used.
Rights and permissions
About this article
Cite this article
Poluektova, A.A., Malskat, W.S.J., van Gemert, M.J.C. et al. Some controversies in endovenous laser ablation of varicose veins addressed by optical–thermal mathematical modeling. Lasers Med Sci 29, 441–452 (2014). https://doi.org/10.1007/s10103-013-1450-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-013-1450-y