Abstract
We report in vivo development of cefiderocol (FDC) resistance among four sequential Pseudomonas aeruginosa clinical isolates ST244 recovered from a single patient, without exposure to FDC, which raises concern about the effectiveness of this novel drug. The first recovered P. aeruginosa isolate (P-01) was susceptible to FDC (2 μg/mL), albeit this MIC value was higher than that of a wild-type P. aeruginosa (0.12–0.25 μg/ml). The subsequent isolated strains (P-02, P-03, P-04) displayed increasing levels of FDC MICs (8, 16, and 64 μg/ml, respectively). Those isolates also showed variable and gradual increasing levels of resistance to most β-lactams tested in this study. Surprisingly, no acquired β-lactamase was identified in any of those isolates. Whole-genome sequence analysis suggested that this resistance was driven by multifactorial mechanisms including mutational changes in iron transporter proteins associated with FDC uptake, ampC gene overproduction, and mexAB-oprM overexpression. These findings highlight that a susceptibility testing to FDC must be performed prior to any prescription.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Pseudomonas aeruginosa is one of the most frequent nosocomial pathogens, particularly as a source of acquired pneumonia in intensive care units with a tendency towards multidrug resistance [1]. Cefiderocol (FDC) is a novel siderophore cephalosporin that shows activity against most multidrug-resistant P. aeruginosa strains, including carbapenem-resistant P. aeruginosa [2]. Its broad and excellent activity is explained by its unique and so-called Trojan horse strategy relying on the active penetration into Gram-negative bacterial cells using its iron transport system [3]. There is some evidence of acquired resistance to FDC. Nevertheless, it seems that the potential for resistance acquisition remains low [4, 5]. The mechanisms underlying this resistance remain poorly understood. Resistance to FDC in P. aeruginosa has been demonstrated to be associated with alterations of iron uptake pathways [6], structural modification of the natural AmpC β-lactamase [7], and modification of the expression of efflux systems. The aim of this study was to decipher the mechanisms and associated genetic determinants responsible for increased resistance pattern to FDC among four sequential P. aeruginosa isolates recovered from a single patient who had never been treated with FDC.
Case history
A 65-year-old patient was hospitalized in the surgical intensive care unit of the Lille University Hospital for acute respiratory distress syndrome following pancreaticoduodenectomy. His medical history included fibrosing interstitial lung disease and rheumatoid arthritis. This patient developed ventilator-acquired pneumonia, for which four sequential clinical isolates of P. aeruginosa (P-01, P-02, P-03, and P-04) were recovered over a period of 3 weeks. The first and second isolates (P-01 and P-02) were from tracheal aspirate samples during the first week of ventilator-associated pneumonia. The second isolate (P-02) was already resistant to all tested β-lactams except ceftolozane-tazobactam (C/T). The patient was treated with meropenem (1 g q8h) IV associated with colistin IV (9 MUI q12h) because C/T was unavailable due to long-term drug shortage. The third and fourth isolates (P-03 and P-04) were recovered from tracheal aspirate samples during the second and third week of treatment, respectively.
Methods
Antimicrobial susceptibility testing was performed by using the disk diffusion method on Mueller–Hinton agar plates for selected antibiotics. Minimum inhibitory concentrations (MICs) were then determined using Etest strips (bioMérieux, La Balme-les-Grottes, France) on Mueller–Hinton agar plates at 37 °C for all antibiotics or antibiotic combinations except for FDC and colistin. MIC values of FDC were determined with the reference BMD method using iron-depleted cation-adjusted Mueller–Hinton (ID-CAMH) broth prepared following the protocol described by Hackel et al. [8]. MICs of colistin were determined using broth microdilution in cation-adjusted Mueller–Hinton broth (Bio-Rad). The results were interpreted according to the latest EUCAST breakpoints (https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_12.0_Breakpoint_Tables.pdf) [9]. The reference strain P. aeruginosa ATCC 27,853 was used as quality control for all testing.
Whole-genome sequencing (WGS) was performed for the four isolates with the ultimate goal to investigate the molecular mechanisms underlying such resistance pattern. The entire genome was sequenced using a MiSeq Illumina platform (Illumina, San Diego, CA, USA) using the Nextera sample preparation method with 2 × 150 bp paired end reads. Illumina short reads were assembled using the CLC Genomic Workbench (version 20.0.4; CLC Bio, Aarhus, Denmark), and contigs with a minimum contig length of 800 nucleotides (nt) were generated. The resulting assembled sequences were analyzed using ResFinder 4.1 software (for antimicrobial resistance genes) and MLST 2.0 software (for Multilocus sequence typing (MLST) analysis on the Center for Genomic Epidemiology server (http://www.genomicepidemiology.org/). The raw sequence data project had been deposited at GenBank under accession no PRJNA856996.
Results
According to results of antimicrobial susceptibility testing and considering the EUCAST resistance breakpoint for FDC at > 2 μg/ml, the first P. aeruginosa isolate recovered (P-01) was susceptible to FDC (2 μg/ml), albeit this MIC value was higher than that of wild-type P. aeruginosa (0.125–0.25 μg/ml). The subsequent isolates (P-02, P-03, P-04) displayed gradual elevation of FDC MICs (8, 16, and 64 μg/ml, respectively) (Table 1). Those P. aeruginosa isolates showed also variable and increasing levels of resistance to most β-lactams including meropenem (8 to > 32 μg/ml), meropenem/vaborbactam (4 to > 64 μg/ml), imipenem (> 32 μg/ml), imipenem/relebactam (3 to > 32 μg/ml), ceftazidime (16 to > 256 μg/ml), ceftazidime/avibactam (1.5 to > 256 μg/ml), ceftolozane/tazobactam (0.75 to > 2 μg/ml), cefepime (8 to 48 μg/ml), aztreonam (8 to > 256 μg/ml), tetracycline (2 to > 256 μg/ml), and chloramphenicol (> 256 μg/ml). The MIC of colistin remained unchanged and was found to be 1–2 μg/ml for all those isolates.
All isolates possessed identical intrinsic β-lactamase genes (blaOXA-847 [encoding a narrow-spectrum oxacillinase], blaPDC-1 [encoding an AmpC-type cephalosporinase]) but no acquired β-lactamase were identified. All four P. aeruginosa strains were found to belong to sequence-type ST244, one of the most widely distributed clones worldwide. WGS data of the four strains were analyzed compared to the reference strain P. aeruginosa PAO1 (GenBank no. AE004091.2).
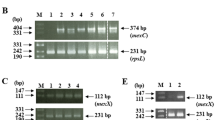
Considering that no acquired β-lactamases were found in any of those isolates, efforts were directed towards examining P. aeruginosa targets potentially involved in other known resistance to FDC. These included insertions, deletions, and mutations in pirS, piR, pirA, piuA, piuB, exbB-exbD-tonB3 or mutations in the pvdS, fecI, fecR, fecA, fpvA, fpvB, and fiuA—all components of the bacterial iron transport system. Also, proteins associated with impaired permeability were also assessed [7, 12]. Several identical mutations were identified in various TonB-dependent receptor proteins in all four strains including pirA (A370T), piuA (Q38H), piuB (I343L, AN573-574TD), TonB3 (F35L, V122A), fvpB (T67K, A125T, E262D), fecA (T339A, H363R) and fiuA (M670I, A677T, T771A) (Table 1). A single amino acid substitution (D89E) was identified in MexR, the negative regulator of the MexAB-OprM efflux pump, in the three FDC-resistant strains (P-02, P-03, P-04) but not in the FDC-susceptible strain P-01.
To evaluate whether this reduced susceptibility to FDC could be related to increased expression of the ampC gene, MIC values for FDC were determined in combination with cloxacillin, an inhibitor of AmpC activity (Table 1). Hence, MICs of FDC dropped to 0.5, 2, 2, and 2 μg/ml for P-01, P-02, P-03, and P-04, respectively, when combined with cloxacillin at a fixed concentration of 2000 μg/ml. Further analysis of the WGS data identified the absence of the ampD gene in all isolates, this feature being known to induce upregulation of the ampC gene. Moreover, a single amino acid substitution (Ala219Thr) was identified in AmpDh3 of the four isolates analyzed. By analyzing the outer membrane proteins of P. aeruginosa, the OprD outer membrane porin, which is involved in carbapenem uptake, was found to be truncated in all four strains that were actually resistant to carbapenem.
Discussion
The siderophore cephalosporin cefiderocol is one of the most promising commercialized agents against carbapenem-resistant Gram negatives including carbapenem-resistant P. aeruginosa. Although still uncommon, reduced susceptibility or resistance to FDC is being reported in that species. In this study, four sequential P. aeruginosa isolates were recovered from a single patient and analyzed using WGS. These isolates showed an increasing trend of resistance to broad-spectrum spectrum cephalosporins, carbapenems, and FDC over the time, without history of FDC exposure. Using the complete genome sequence data of the four P. aeruginosa isolates, all strains were shown to belong to the same sequence type, namely, ST244, a globally disseminated high-risk clone [10, 11].
The same mutations were detected in various iron transporters (pirA, piuA, piuB, TonB3, fvpB, fecA and fiuA), responsible for the active transport of FDC, for the four strains. These mutations may play an essential role in the basic increase of FDC MICs in all four strains and could be a potential mechanism of FDC resistance development in P. aeruginosa as previously reported [13,14,15,16]. However, those mutations in corresponding genes cannot explain by themselves the difference of susceptibility to FDC between those four strains.
The amino acid substitution found in MexR in the three FDC-resistant strains (P-02, P-03, P-04) was likely resulting in the overexpression of the mexAB-oprM multidrug efflux pump genes that may contribute to additional FDC resistance in those three strains as previously reported [17]. No mutation in the genes encoding TonB-dependent receptors (TBDRs) was identified in those isolates [17]. Very recently, Ikawa et al. indicated that the MexAB-OprM drug efflux system contributes to the intrinsic resistance to FDC in P. aeruginosa and found that the mexAB-oprM-deficient P. aeruginosa mutant displayed increased FDC susceptibility compared to the wild-type strain. On the other hand, the overexpression of mexAB-oprM in the mexAB-oprM-deficient mutant increased the MIC value of FDC [18]. In another study, MIC of FDC was slightly affected by the oprD gene deficiency or the overproduction of MexAB-OprM multidrug efflux pump due to a defect in the mexR or nalD regulatory genes in P. aeruginosa [4]. Although the association between MexAB-OprM overproduction and reduced FDC activity is still poorly understood, the role of mexAB-OprM overexpression in reducing FDC activity needs to be further explored as FDC could be a substrate of this efflux pump. Interestingly, truncation of the OprD-encoding gene had been previously reported among in vivo selected FDC-resistant clinical P. aeruginosa isolates (after FDC treatment) [14].
MICs of FDC were significantly decreased in the presence of cloxacillin, suggesting that overexpression of ampC gene was involved in the increased MICs of FDC in those four P. aeruginosa isolates. This increased expression of the ampC gene could be explained by the inactivation of ampD gene in the four isolates as previously described [19,20,21,22]. In a study, mutations in the ampD gene were associated with modest increases in FDC MICs to 2 μg/ml, remaining in the susceptible range in that latter case [17]. Moreover, the amino-acid substitution (Ala219Thr) identified in AmpDh3 of the four isolates might play an important role in overproduction of cephalosporinase leading to ceftazidime resistance, as previously reported [23], which likely cause collateral resistance to FDC since FDC combines chemical moieties of ceftazidime and cefepime. We noticed that the FDC-resistant P. aeruginosa strains (P-02, P-03, and P-04) showed a 4- to tenfold increase in FDC MICs compared to the FDC susceptible isolate (P-01). This increase in FDC MICs could be attributed to strong collateral-resistance with ceftazidime for which MICs were elevated by 4- to ≥ eightfold in those FDC-resistant P. aeruginosa strains compared to the FDC-susceptible isolate (P-01). Similar results were observed for cefepime and ceftazidime/avibactam (Table 1). Very recently, it has been shown that development of FDC resistance was often associated with collateral susceptibility changes towards other β-lactams such as increased resistance to ceftazidime and ceftazidime/avibactam [24].
In conclusion, we report here in vivo development of FDC resistance in P. aeruginosa clinical isolates without exposure to FDC is raising concerns about the effectiveness of this promising drug. Whole-genome sequence analysis suggests that this resistance was driven by multifactorial mechanisms including changes in iron transporter proteins, ampC gene overproduction, and mexAB-oprM overexpression.
References
De Bentzmann S, Plésiat P (2011) The Pseudomonas aeruginosa opportunistic pathogen and human infections. Environ Microbiol 13(7):1655–1665. https://doi.org/10.1111/j.1462-2920.2011.02469.x
Kazmierczak KM, Tsuji M, Wise MG et al (2019) In vitro activity of cefiderocol, a siderophore cephalosporin, against a recent collection of clinically relevant carbapenem-non-susceptible Gram-negative bacilli, including serine carbapenemase- and metallo-β-lactamase-producing isolates (SIDERO-WT-2014 Study). Int J Antimicrob Agents 53:177–184. https://doi.org/10.1016/j.ijantimicag.2018.10.007
Sato T, Yamawaki K (2019) Cefiderocol: discovery, chemistry, and in vivo profiles of a novel siderophore cephalosporin. Clin Infect Dis 69(Suppl 7):S538–S543. https://doi.org/10.1093/cid/ciz826
Ito A, Sato T, Ota M et al (2017) In vitro antibacterial properties of cefiderocol, a novel siderophore cephalosporin, against Gram-negative bacteria. Antimicrob Agents Chemother 62(1):e01454-e1517. https://doi.org/10.1128/AAC.01454-17
Kohira N, Hackel MA, Ishioka Y et al (2020) Reduced susceptibility mechanism to cefiderocol, a siderophore cephalosporin, among clinical isolates from a global surveillance programme (SIDERO-WT-2014). J Glob Antimicrob Resist 22:738–741. https://doi.org/10.1016/j.jgar.2020.07.009
Ito A, Nishikawa T, Ishii R et al (2018a) Mechanism of cefiderocol high MIC mutants obtained in non-clinical FoR studies. Poster presented at: IDWeek, San Francisco, CA, 3–7 October 2018. Poster 69.
Nordmann P, Shields RK, Doi Y et al (2022) Mechanisms of reduced susceptibility to cefiderocol among isolates from the CREDIBLE-CR and APEKS-NP clinical trials. Microb Drug Resist 28(4):398–407. https://doi.org/10.1089/mdr.2021.0180
Hackel MA, Tsuji M, Yamano Y, Echols R, Karlowsky JA, Sahm DF (2019) Reproducibility of broth microdilution MICs for the novel siderophore cephalosporin, cefiderocol, determined using iron-depleted cation-adjusted Mueller-Hinton broth. Diagn Microbiol Infect Dis 94(4):321–325. https://doi.org/10.1016/j.diagmicrobio.2019.03.003
EUCAST (2022) The European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters. Version 12.0, 2022. http://www.eucast.org
Moyo S, Haldorsen B, Aboud S et al (2015) Identification of VIM-2-producing Pseudomonas aeruginosa from Tanzania is associated with sequence types 244 and 640 and the location of blaVIM-2 in a TniC integron. Antimicrob Agents Chemother 59(1):682–685. https://doi.org/10.1128/AAC.01436-13
Del Barrio-Tofiño E, López-Causapé C, Oliver A (2020) Pseudomonas aeruginosa epidemic high-risk clones and their association with horizontally-acquired β-lactamases: 2020 update. Int J Antimicrob Agents 56(6):106196. https://doi.org/10.1016/j.ijantimicag.2020.106196
Lister PD, Wolter DJ, Hanson ND (2009) Antibacterial-resistant Pseudomonas aeruginosa: clinical impact and complex regulation of chromosomally encoded resistance mechanisms. Clin Microbiol Rev 22(4):582–610. https://doi.org/10.1128/CMR.00040-09
Luscher A, Moynié L, Auguste PS et al (2018) TonB-dependent receptor repertoire of Pseudomonas aeruginosa for uptake of siderophore-drug conjugates. Antimicrob Agents Chemother 62:e00097-e118. https://doi.org/10.1128/AAC.00097-18
Karakonstantis S, Rousaki M, Kitsotakis EI (2022) Cefiderocol: systematic review of mechanisms of resistance, heteroresistance and in vivo emergence of resistance. Antibiotics 11(6):723. https://doi.org/10.3390/antibiotics11060723
Malik S, Kaminski M, Landman D, Quale J (2020) Cefiderocol resistance in Acinetobacter baumannii: roles of β-Lactamases, siderophore receptors, and Penicillin Binding Protein 3. Antimicrob Agents Chemother 64(11):e01221-e1320. https://doi.org/10.1128/AAC.01221-20
McElheny CL, Fowler EL, Iovleva A, Shields RK, Doi Y (2021) In vitro evolution of cefiderocol resistance in an NDM-producing Klebsiella pneumoniae due to functional loss of CirA. Microbiol Spectr 9(3):e0177921. https://doi.org/10.1128/Spectrum.01779-21
Simner PJ, Beisken S, Bergman Y, Posch AE, Cosgrove SE, Tamma PD (2021) Cefiderocol activity against clinical Pseudomonas aeruginosa isolates exhibiting ceftolozane-tazobactam resistance. Open Forum Infect Dis 8(7):ofab311. https://doi.org/10.1093/ofid/ofab311
Ikawa S, Yamasaki S, Morita Y, Nishino K (2022) Role of the drug efflux pump in the intrinsic cefiderocol resistance of Pseudomonas aeruginosa. bioRxiv. https://doi.org/10.1101/2022.05.31.494263
Zamorano L, Moyá B, Juan C, Oliver A (2010) Differential beta-lactam resistance response driven by ampD or dacB (PBP4) inactivation in genetically diverse Pseudomonas aeruginosa strains. J Antimicrob Chemother 65(7):1540–1542. https://doi.org/10.1093/jac/dkq142
Bagge N, Ciofu O, Hentzer M, Campbell JI, Givskov M, Høiby N (2002) Constitutive high expression of chromosomal beta-lactamase in Pseudomonas aeruginosa caused by a new insertion sequence (IS1669) located in ampD. Antimicrob Agents Chemother 46(11):3406–3411. https://doi.org/10.1128/AAC.46.11.3406-3411.2002
Juan C, Maciá MD, Gutiérrez O, Vidal C, Pérez JL, Oliver A (2005) Molecular mechanisms of beta-lactam resistance mediated by AmpC hyperproduction in Pseudomonas aeruginosa clinical strains. Antimicrob Agents Chemother 49(11):4733–4738. https://doi.org/10.1128/AAC.49.11.4733-4738.2005
Langaee TY, Gagnon L, Huletsky A (2000) Inactivation of the ampD gene in Pseudomonas aeruginosa leads to moderate-basal-level and hyperinducible AmpC beta-lactamase expression. Antimicrob Agents Chemother 44(3):583–589. https://doi.org/10.1128/AAC.44.3.583-589.2000
Schmidtke AJ, Hanson ND (2008) Role of ampD homologs in overproduction of AmpC in clinical isolates of Pseudomonas aeruginosa. Antimicrob Agents Chemother 52(11):3922–3927. https://doi.org/10.1128/AAC.00341-08
Fröhlich C, Sørum V, Tokuriki N, Johnsen PJ, Samuelsen Ø (2022) Evolution of β-lactamase-mediated cefiderocol resistance. J Antimicrob Chemother dkac221 77(9):2429–2436. https://doi.org/10.1093/jac/dkac221
Funding
Open access funding provided by University of Fribourg This work was supported by I-Site ULNE—Grant R-TALENTS-20–004- and by Région Hauts de France, Project INTHREPIDE AntibioResistance – Grant No. 21008838.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sadek, M., Le Guern, R., Kipnis, E. et al. Progressive in vivo development of resistance to cefiderocol in Pseudomonas aeruginosa. Eur J Clin Microbiol Infect Dis 42, 61–66 (2023). https://doi.org/10.1007/s10096-022-04526-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-022-04526-0