Abstract
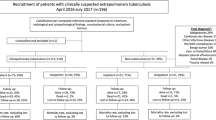
The burden of extrapulmonary tuberculosis (EPTB) has gradually increased in recent years, but not enough epidemiological data is available from central Guangxi. To better understand the epidemiology of EPTB in central Guangxi and identify risk factors associated with them, we retrospectively investigated the epidemiology of tuberculosis (TB), especially EPTB, among patients admitted to the Chest Hospital of Guangxi Zhuang Autonomous Region between 2016 and 2021. We excluded those infected with both pulmonary tuberculosis (PTB) and EPTB, reported the proportion and incidence of PTB or EPTB, and compared the demographic characteristics and risk factors of EPTB and PTB cases using univariate and multivariate logistic regression models. Among 30,893 TB patients, 67.25% (20,774) had PTB and 32.75% (10,119) had EPTB. Among EPTB, pleural, skeletal, lymphatic, pericardial, meningeal, genitourinary, intestinal, and peritoneal TB accounted for 49.44%, 27.20%, 8.55%, 4.39%, 3.36%, 1.48%, 0.87%, and 0.79%, respectively. Patients who were younger (age < 25), from rural areas, Zhuang and other ethnic groups, and diagnosed with anemia and HIV infection were more likely to develop EPTB. However, patients with diabetes and COPD were less likely to have EPTB. From 2016 to 2021, the proportion of PTB cases decreased from 69.73 to 64.07%. The percentage of EPTB cases increased from 30.27 to 35.93%, with the largest increase in skeletal TB from 21.48 to 34.13%. The epidemiology and risk factors of EPTB in central Guangxi are different from those of PTB. The incidence of EPTB is increasing and further studies are needed to determine the reasons for it.



Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are not publicly available because of ethical and legal reasons but are available from the corresponding author Jing Leng on reasonable request.
References
WHO (2020) Tuberculosis. Available from: https://www.who.int/health-topics/tuberculosis#tab=tab_1.
Yadav J et al (2019) Tuberculosis: current status, diagnosis, treatment and development of novel vaccines. Curr Pharm Biotechnol 20(6):446–458
Solovic I et al (2013) Challenges in diagnosing extrapulmonary tuberculosis in the European Union, 2011. Euro Surveillance : Bulletin Europeen Sur Les Maladies Transmissibles = European Communicable Disease Bulletin 18(12)
Bomanji J et al (2020) PET/CT features of extrapulmonary tuberculosis at first clinical presentation: a cross-sectional observational F-FDG imaging study across six countries. Eur Respir J 55(2)
Banta JE et al (2020) Pulmonary vs. extra-pulmonary tuberculosis hospitalizations in the US [1998-2014]. J Infect Public Health 13(1):131–139
Thakur K et al (2018) The global neurological burden of tuberculosis. Semin Neurol 38(2):226–237
Mazza-Stalder J, Nicod L, Janssens JP (2012) Extrapulmonary tuberculosis. Rev Mal Respir 29(4):566–578
Sharma SK, Mohan A, Kohli M (2021) Extrapulmonary tuberculosis. Expert Rev Respir Med 15(7):931–948
Rodriguez-Takeuchi SY, Renjifo ME, Medina FJ (2019) Extrapulmonary tuberculosis: pathophysiology and imaging findings. Radiographics : a Review Publication of the Radiological Society of North America, Inc,. 39(7):2023–2037
WHO (2021) Tuberculosis data. Available from: https://www.who.int/teams/global-tuberculosis-programme/data
Qian X et al (2018) Risk factors for extrapulmonary dissemination of tuberculosis and associated mortality during treatment for extrapulmonary tuberculosis. Emerg Microbes Infect 7(1):102
Khan AH et al (2019) Treatment outcomes and risk factors of extra-pulmonary tuberculosis in patients with co-morbidities. BMC Infect Dis 19(1):691
Sotgiu G et al (2017) Determinants of site of tuberculosis disease: An analysis of European surveillance data from 2003 to 2014. PLoS One 12(11):e0186499
Chakaya J et al (2021) Global Tuberculosis Report 2020 - Reflections on the Global TB burden, treatment and prevention efforts. Int J Infect Dis IJID Off Publ Int Soc For Infect Dis 113:Suppl 1
Cui Z et al (2017) Risk factors associated with Tuberculosis (TB) among people living with HIV/AIDS: A pair-matched case-control study in Guangxi, China. PLoS One 12(3):e0173976
Zeng H et al (2021) Analysis of clinical characteristics of 556 spinal tuberculosis patients in two tertiary teaching hospitals in Guangxi Province. Biomed Res Int 2021:1344496
Zheng Y et al (2020) Statistical methods for predicting tuberculosis incidence based on data from Guangxi, China. BMC Infect Dis 20(1):300
Pang Y et al (2019) Epidemiology of extrapulmonary tuberculosis among inpatients, China, 2008–2017. Emerg Infect Dis 25(3):457–464
Liu Y et al (2020) Description of demographic and clinical characteristics of extrapulmonary tuberculosis in Shandong. China Hippokratia 24(1):27–32
Chen L et al (2021) Upward trends in new, rifampicin-resistant and concurrent extrapulmonary tuberculosis cases in northern Guizhou Province of China. Sci Rep 11(1):18023
WHO (2009) Treatment of tuberculosis guidelines. Available from: http://whqlibdoc.who.int/publications/2010/9789241547833_eng.pdf
Health MO (2004) Guidelines for diabetes control and prevention in China., Beijing: Peking University Press
Ohene S-A et al (2019) Extra-pulmonary tuberculosis: A retrospective study of patients in Accra, Ghana. PLoS One 14(1):e0209650
Wang X et al (2014) Insight to the epidemiology and risk factors of extrapulmonary tuberculosis in Tianjin, China during 2006–2011. PLoS One 9(12):e112213
Norbis L et al (2014) Challenges and perspectives in the diagnosis of extrapulmonary tuberculosis. Expert Rev Anti Infect Ther 12(5):633–647
Minnies S et al (2021) Xpert MTB/RIF ultra is highly sensitive for the diagnosis of tuberculosis lymphadenitis in a High-HIV setting. J Clin Microbiol 59(12):e0131621
Zhou Y et al (2021) Aptamer detection of mannose-capped lipoarabinomannan in lesion tissues for tuberculosis diagnosis. Front Cell Infect Microbiol 11:634915
Khosravi AD et al (2017) Identification of in clinical specimens of patients suspected of having extrapulmonary tuberculosis by application of nested PCR on five different genes. Front Cell Infect Microbiol 7:3
Singh BK et al (2020) Evaluation of genotype MTBDRplus V2 and genotype MTBDRsl V2 for the diagnosis of extrapulmonary tuberculosis in India. Tuberculosis (Edinb) 125:102014
Mandal N et al (2017) Diagnosis and treatment of paediatric tuberculosis: An insight review. Crit Rev Microbiol 43(4):466–480
Roy A et al (2014) Effect of BCG vaccination against Mycobacterium tuberculosis infection in children: systematic review and meta-analysis. BMJ (Clinical Research ed) 349:g4643
Pang Y et al (2016) Current status of new tuberculosis vaccine in children. Hum Vaccin Immunother 12(4):960–970
Wang J et al (2021) Two cases of disseminated BCG disease following vaccination in the same family: case reports and review of the literature in China. Hum Vaccin Immunother 17(5):1382–1386
Han J et al (2020) Mechanisms of BCG in the treatment of bladder cancer-current understanding and the prospect. Biomed Pharmacother = Biomed Pharmacother 129:110393
Kang W et al (2020) The epidemiology of extrapulmonary tuberculosis in China: A large-scale multi-center observational study. PLoS One 15(8):e0237753
Sreeramareddy CT et al (2008) Comparison of pulmonary and extrapulmonary tuberculosis in Nepal- a hospital-based retrospective study. BMC Infect Dis 8:8
Al-Otaibi F, El Hazmi MM (2010) Extra-pulmonary tuberculosis in Saudi Arabia. Indian J Pathol Microbiol 53(2):227–231
Guler SA et al (2015) Evaluation of pulmonary and extrapulmonary tuberculosis in immunocompetent adults: a retrospective case series analysis. Med Princ Pract Int J Kuwait Univ Health Sci Cent 24(1):75–79
Davis AG et al (2019) The pathogenesis of tuberculous meningitis. J Leukoc Biol 105(2):267–280
Rajagopalan S (2016) Tuberculosis in Older Adults. Clin Geriatr Med 32(3):479–491
Wu X-R et al (2012) Pediatric tuberculosis at Beijing Children’s Hospital: 2002–2010. Pediatrics 130(6):e1433–e1440
Apidechkul T (2016) A 20-year retrospective cohort study of TB infection among the Hill-tribe HIV/AIDS populations, Thailand. BMC Infect Dis 16:72
Zhou Y-B et al (2014) HIV-, HCV-, and co-infections and associated risk factors among drug users in southwestern China: a township-level ecological study incorporating spatial regression. PLoS One 9(3):e93157
Pan D et al (2019) Infectivity of Genotypes and Outcome of Contact Investigation in Classroom in Guangxi, China. BioMed Res Int 2019:3980658
Culqui-Lévano DR, Rodriguez-Valín E, Donado-Campos JdM (2017) Analysis of extrapulmonary tuberculosis in Spain: 2007-2012 National Study. Enferm Infecc Microbiol Clin 35(2):82–87
Shivakoti R et al (2017) Association of HIV infection with extrapulmonary tuberculosis: a systematic review. Infection 45(1):11–21
Piskur ZI, Mykolyshyn LI (2021) Comorbidities at the Tuberculosis among Children. Wiadomosci Lekarskie (Warsaw, Poland : 1960). 74(10 pt 1):2433–2438
Schümann K, Solomons NW (2017) Perspective: What Makes It So Difficult to Mitigate Worldwide Anemia Prevalence? Advances In Nutrition (Bethesda, Md.) 8(3):401–408
Chhabra S et al (2021) Anemia and Nutritional Status in Tuberculosis Patients. Int J Appl Basic Med Res 11(4):226–230
Mukherjee A et al (2019) Prevalence, characteristics, and predictors of tuberculosis associated anemia. J Fam Med Prim Care 8(7):2445–2449
Kerkhoff AD et al (2016) Anaemia in patients with HIV-associated TB: relative contributions of anaemia of chronic disease and iron deficiency. Int J Tuberc Lung Dis Off J Int Union Against Tuberc Lung Dis 20(2):193–201
Leeds IL et al (2012) Site of extrapulmonary tuberculosis is associated with HIV infection. Clin Infect Dis Off Publ Infect Dis Soc Am 55(1):75–81
Gomes T et al (2014) Epidemiology of extrapulmonary tuberculosis in Brazil: a hierarchical model. BMC Infect Dis 14:9
Le Y et al (2020) Infection of Promotes Both M1/M2 Polarization and MMP Production in Cigarette Smoke-Exposed Macrophages. Front Immunol 11:1902
Jin J et al (2018) Emphysema and bronchiectasis in COPD patients with previous pulmonary tuberculosis: computed tomography features and clinical implications. Int J Chron Obstruct Pulmon Dis 13:375–384
Shirzad-Aski H et al (2020) Incidence, risk factors and clinical characteristics of extra-pulmonary tuberculosis patients: a ten-year study in the North of Iran. Trop Med Int Health TM IH 25(9):1131–1139
Magee MJ et al (2016) Diabetes mellitus and extrapulmonary tuberculosis: site distribution and risk of mortality. Epidemiol Infect 144(10):2209–2216
Lee MK et al (2021) Risk factors for the delayed diagnosis of extrapulmonary TB. Int J Tuberc Lung Dis Off J Int Union Against Tuberc Lung Dis 25(3):191–198
Khanna K, Sabharwal S (2019) Spinal tuberculosis: a comprehensive review for the modern spine surgeon. Spine J Off J North Am Spine Soc 19(11):1858–1870
Pigrau-Serrallach C, Rodríguez-Pardo D (2013) Bone and joint tuberculosis. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cervic Spine Res Soc 22(Suppl 4):556–566
Zhu B et al (2018) Tuberculosis vaccines: Opportunities and challenges. Respirology (Carlton, Vic.). 23(4):359–368
Acknowledgements
We thank Peng Zhang for his help in data processing techniques. Thanks to all participants of this study and Guangxi Chest Hospital for their support.
Funding
This research was supported by Guangxi Key Research and Development Program (Nos. GuikeAB20072005 and GuikeAB22035027). Jing Leng and Yanling Hu were received research grants from these two funds, respectively.
Author information
Authors and Affiliations
Contributions
All authors contributed to study conception and design. Y.L.H, J.L, J.N.L, Y.Z.W, A.M.L: designed the study and provided the correlative knowledge. D.W, L.S.S, Q.Y.L, and K.L: collected and provided the data. L.X.L, X.W.P, B.X, Z.J.L, and X.H.W extracted data and cleaned data. L.X.L, X.W.P, and B.X generated the figures and tables. L.X.L, J.L, Y.Z.W, Y.L.H, and J.N.L: wrote and edited the manuscript. All of the authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical considerations
This study was approved by the Ethics Committee of the Chest Hospital of Guangxi Zhuang Autonomous Region (approval number: 2022–09). The study used data collected from the patient records of the hospital inpatient information management system. To protect the privacy of patients, the hospital gave them a digital password and kept their names, ID numbers, and other details confidential. The hospital’s Institutional Review Board approved the waiver of patients’ informed consent because the study posed no risks for patients.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, L., Lv, Y., Su, L. et al. Epidemiology of extrapulmonary tuberculosis in central Guangxi from 2016 to 2021. Eur J Clin Microbiol Infect Dis 42, 129–140 (2023). https://doi.org/10.1007/s10096-022-04524-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-022-04524-2