Abstract
Alveolar echinococcosis (AE) is caused by the larval stage of Echinococcus multilocularis. Chemotherapy for AE involves albendazole (ABZ), which has shown insufficient efficacy. More effective chemotherapy for AE is needed. Previously, we have demonstrated that atovaquone (ATV), an antimalarial, inhibits mitochondrial complex III of E. multilocularis and restricts the development of larval cysts in in vivo experiments. Therefore, in this study, we evaluated the efficacy of ABZ and ATV combination therapy on E. multilocularis in culture and in vivo experiments. Protoscoleces were treated with 50 μM ABZ and/or ATV in the medium; the duration of parasite elimination was determined under aerobic and anaerobic culture. In the in vivo experiment, the effects of ABZ and ATV combination treatment in BALB/c mice infected orally with eggs from the feces of an adult-stage E. multilocularis-infected dog were compared with those of standard oral ABZ therapy. In the culture assay, the duration of elimination associated with ABZ and ATV combination treatment was shorter than that associated with ATV alone under aerobic conditions. Protoscolex viability progressively reduced owing to the combination treatment under anaerobic conditions; however, either drug used singly did not exhibit antiparasitic effects under hypoxia. Furthermore, compared with ABZ alone, the combination treatment significantly reduced the growth of the primary cyst in the liver of mice infected orally with parasite eggs (P = .011). ATV enhances the effect of ABZ in the treatment of AE in mice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alveolar echinococcosis (AE) is a helminthic zoonotic disease caused by infection with the larval stage of the cestode parasite Echinococcus multilocularis [1]. The prevalence of AE is highest in China, Central Asia, Russia, parts of Europe, and Japan [1]. Adult-stage E. multilocularis release their eggs into the feces of the definitive host. The accidental ingestion of the eggs by intermediate hosts, such as small rodents, leads to the release of infective larvae (oncospheres) in the intestinal lumen. The oncospheres mainly reach the liver via the circulatory system, in which they grow into metacestodes (larval cysts) containing protoscoleces. After predation of the infected rodent by Canidae such as foxes, the protoscoleces transform and develop into adult tapeworms in the small intestine. Humans are infected as an aberrant intermediate host upon accidentally swallowing the parasite eggs. The growth of larval cysts in the liver leads to life-threatening conditions, such as organ dysfunction, several years after infection.
Radical surgical resection of the parasitic mass is the basis of treatment for AE and is usually accompanied by chemotherapy [1, 2]. In cases with inoperable advanced cysts of AE, the chemotherapeutic treatment involves albendazole (ABZ), which is not adequately efficacious [3]. During the clinical course, chemotherapy plays an important role in the process of treatment as an increase in the number of larval cysts in the liver is associated with a poor prognosis. Hence, many in vivo experiments have been performed to assess the efficacy of combination therapy with ABZ and other compounds [4].
We focused on the mitochondrial respiratory systems of the parasite as the drug target in this study. E. multilocularis employs an aerobic respiratory pathway, oxidative phosphorylation, or an anaerobic pathway, fumarate respiration, for its survival in various oxygen conditions [5,6,7]. The eggs of E. multilocularis excreted from the definitive host are exposed to oxygen in the long term. The oncosphere and metacestodes (larval cysts) reside in the artery and liver of the intermediate host, respectively. These stages, which are the target of treatment, can access the portal vein and hepatic vein that exhibit high arterial oxygen tension. However, it is difficult for these stages to access oxygen owing to their size and site of infection. Adult worms live in the intestine of the definitive host, under low-oxygen conditions. A similar change in the respiratory system is also found in other parasites [8,9,10,11].
Briefly, oxidative phosphorylation generally involves complexes I to IV and V. Complex I oxidizes NADH and passes electrons to ubiquinone. Complex II receives electrons from succinate and functions as succinate-quinone reductase. Ubiquinone transfers the reducing equivalent to complex III, which passes it to complex IV via cytochrome c. Proton-motive force is generated across the inner mitochondrial membrane at complexes I, III, and IV, which drive ATP synthesis through complex V. In contrast, fumarate respiration involves complexes I, II, and rhodoquinone. Complex I acts as a proton pump that is driven by the oxidation of NADH and contributes to the reduction of rhodoquinone. Complex II accepts electrons from rhodoquinol and catalyzes the reduction of fumarate to succinate as a terminal oxidase. Quinol-fumarate reductase activity is the reverse reaction of the succinate-quinone reductase activity of complex II under anaerobic conditions. As the advantage of fumarate respiration, ATP can be synthesized by the proton-pump activity of complex I and ATP synthase (complex V) even under low-oxygen conditions.
We have previously reported that atovaquone (ATV), a cytochrome bc1 complex inhibitor and antimalarial agent, inhibits mitochondrial complex III of E. multilocularis at extremely low concentrations and decreases the development of larval cysts in in vivo experiments [5]. However, in the case of E. multilocularis, the effect of ATV alone is limited compared with that of ABZ in treated mice because ATV inhibits only aerobic respiration [5]. Therefore, in this study, the in vivo effects of combination therapy with ABZ and ATV were compared to those of standard oral ABZ treatments in mice with primary hydatid cysts after being orally infected with eggs of E. multilocularis as a natural infection model.
Methods
Culture assay of live E. multilocularis protoscoleces
A culture assay was performed to determine the efficacy of the combination of ABZ and ATV. The protoscoleces obtained were cultured in Connaught Medical Research Laboratories 1066 medium (Gibco, Grand Island, NY, USA) containing 0.5% (w/v) yeast extract (Difco Laboratories, Detroit, MI, USA), 23 mM 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid, 0.5% (w/v) D (+)-glucose, 0.4 mM sodium taurocholate (Wako Pure Chemical Industries, Osaka, Japan), 57 mM sodium hydrogen carbonate, 2 mM L-glutamine (Gibco), 100 U/mL penicillin, and 100 μg/mL streptomycin (Gibco). Half of the medium was changed on day 3. For anaerobic cultures, six-well plates were sealed in plastic containers with oxygen-detecting agents and oxygen scavengers (Aneromeito®, Nissui Pharmaceutical, Tokyo, Japan) to maintain the oxygen concentration under 0.3% at 37 °C. The protoscoleces were treated with ABZ (Tokyo Chemical Industry, Tokyo, Japan) and/or ATV (Tokyo Chemical Industry) at a final concentration of 50 μM in the culture medium, and the duration of parasite elimination was determined. The control group was supplemented with 0.5% (v/v) dimethyl sulfoxide (DMSO), and all conditions were assayed in triplicate. The viability of protoscoleces was determined by microscopic observation of more than 170 protoscoleces per well using the trypan blue exclusion test.
In vivo studies to determine the efficacy of ABZ and ATV combination treatment in BALB/c mice with primary hydatid cysts
The in vivo effects of ABZ and ATV combination treatment were evaluated and compared with those of standard oral ABZ treatments. BALB/c mice (female, body weight of 25 g, 9 weeks old, and daily average food intake of 4.0 g) were infected orally with 100 μL of a suspension containing 200 eggs obtained from the feces of an adult E. multilocularis-infected dog in biosafety level 3. Three mice were euthanized to confirm the presence of cysts (diameter, 1–2 mm; length, 1–2 mm) in the liver 4 weeks after infection (Fig. 2a). After confirming the growth of larval cysts, 33 BALB/c mice were divided into the following 4 groups: 6 mice in the ABZ group, 9 mice in the ABZ and ATV combination treatment group, 9 mice without treatment, and 9 mice in the ATV group. The no-treatment and ATV groups were considered as the control group to assess whether this in vivo experiment was performed appropriately compared with that reported previously. ABZ and ATV were mixed into the feed at doses of 125 mg/100 g and 133 mg/100 g, respectively, as reported previously [5]. Each agent was blended with pulverized feed by using a Waring blender until a uniform consistency was achieved [12]. Water was added to the clayish feed, and pellets (2 × 2 × 3 cm) were prepared using a spatula. The treatments were performed for 8 weeks by feeding the mice with the drug-mixed feed ad libitum from 8 weeks after infection. The mice were euthanized to investigate the 8-week therapeutic effect. Necropsies were performed, and the proportion of cysts on the liver surface was determined using digital image analysis software (ImageJ, Bethesda, MD, USA) to evaluate the development of larval cysts.
Statistical analysis
The culture assays were performed in triplicate, and the results were each expressed as the mean ± standard error of the mean (SEM) calculated using Microsoft Office Excel 2016 (Microsoft Corporation, Redmond, WA, USA). The results of the in vivo experiments were analyzed using one-way analysis of variance and a multiple comparison test. P < .05 was considered significant. All statistical analyses were performed using EZR (version R3.6.3; Saitama Medical Center, Jichi Medical University, Saitama, Japan) [13].
Results
The results of the culture assay under aerobic and anaerobic conditions are shown in Fig. 1. The protoscoleces in the DMSO control group maintained 98 to 100% viability throughout the experimental period under both conditions. In the culture assay under aerobic conditions, ATV treatment eliminated E. multilocularis protoscoleces completely by day 7. ABZ killed only 10% of the protoscoleces by day 7. The viability of the protoscoleces progressively reduced during in vitro treatment with ABZ plus ATV compared with ATV alone. In the culture assay under anaerobic conditions, ABZ or ATV did not kill any protoscolex by day 7. However, ABZ plus ATV resulted in the elimination of 55% of the protoscoleces by day 7 in the hypoxic culture.
Culture assay under aerobic and anaerobic conditions (O2 < 0.3%). Echinococcus multilocularis protoscoleces were treated with albendazole (ABZ), atovaquone (ATV), and ABZ plus ATV at a final concentration of 50 μM in each culture medium. One control group was supplemented with 0.5% (v/v) dimethyl sulfoxide alone. The protoscoleces were observed daily for seven consecutive days, and their viability was assessed by performing the trypan blue exclusion test. The results represent the means and standard deviation values of at least three samples
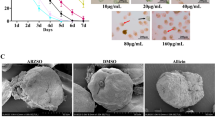
Figure 2 shows representative liver conditions around large cysts before and after treatment to allow a better understanding of the primary hydatid cysts in the mouse liver. Larval cysts, 0.04 to 0.09 cm in diameter, were disseminated on the surface of the liver 4 weeks after infection and before treatment (Fig. 3a). Larval cysts of various shapes and sizes were observed, with a maximum size of 0.3 cm 16 weeks after the oral administration of eggs in the untreated mouse liver (Fig. 3b). The cysts treated by ATV had irregular shapes and various sizes on the liver (Fig. 3c). After ABZ treatment, cysts with uniform shape and diameter of 0.05 to 0.1 cm were observed on the liver (Fig. 3d). In the samples treated by the combination of ABZ and ATV, cysts had a diameter of 0.03 to 0.1 cm and a slightly irregular margin (Fig. 3e). The proportion of cysts on the surface of the liver in Fig. 3a–e was 0.74, 6.5, 4.0, 0.65, and 0.29%, respectively.
Liver lesions in mice (BALB/c) infected orally with a suspension containing 200 eggs obtained from the feces of a dog infected with adult E. multilocularis. Representative samples are selected around large cysts. Before treatment (a): cysts on the liver 4 weeks after infection. No treatment (b): the condition of the liver of an untreated mouse 16 weeks after oral infection with parasite eggs. Atovaquone (ATV) (c), albendazole (ABZ) (d), and ABZ plus ATV (e): all groups were orally administered with each agent for 8 weeks from 8 weeks after infection. The whitish dots and cystic masses on the livers represent infection with established parasites. The proportion of the cyst area on the liver was determined in detail with the digital image analysis software. The proportion of cysts on the liver surface was a 0.73%, b 6.5%, c 4.0%, d 0.65%, and e 0.29%
In vivo effects of albendazole (ABZ) and atovaquone (ATV) combination therapy on primary alveolar hydatid cysts in a mouse model. The cyst area on the liver in the ABZ/ATV treatment group was compared with that in the group treated with standard oral ABZ treatment. No-treatment and ATV groups were created to assess whether this in vivo experiment was performed appropriately compared with that reported previously [6]. The proportion of cysts on the surface of the liver was measured by digital image analysis. *P-value of <.05 at 95% confidence level was considered significant
A significant difference in the area of the larval cysts was observed between the no-treatment and ATV groups (P = .025). Compared with ABZ alone, combination treatment with ABZ and ATV significantly reduced the formation of cysts in the mouse liver (P = .011; Fig. 3).
Discussion
In this study, we assessed the viability of protoscoleces under normoxic and hypoxic culture conditions upon treatment with ABZ and/or ATV. ATV eliminated the parasites strongly under aerobic conditions but not under anaerobic conditions because the target of ATV is complex III, which is not a component in the anaerobic respiratory chain (fumarate respiration) [5]. ABZ only eliminated less than 10% of the protoscoleces under aerobic and anaerobic conditions, although it inhibited the growth of cysts in vivo. It is not clear how the elimination speed in ABZ culture changes after day 8 in this study. The metabolites of ABZ and the immune system of the host might contribute to the effects of ABZ in vivo, although the mechanism of action of ABZ involves the inhibition of tubulin polymerization in the intestinal cells of the parasite [14]. Moreover, the duration of elimination associated with the combined administration of ABZ and ATV was 1 day shorter than that associated with ATV alone under aerobic conditions. Notably, the viability of protoscoleces progressively decreased during the culture assay of the parasite with the coadministration of ABZ and ATV under anaerobic conditions, although the administration of either agent alone did not result in any antiparasitic effect. The result of culture assay supports the significant reduction of the cyst area by the in vivo combination treatment.
An in vivo experiment was performed to evaluate the efficacy of ABZ and ATV combination treatment against primary hydatid cysts in infected mice. We demonstrated that the area of the cysts in vivo was significantly restricted by the combination of ABZ and ATV. Under aerobic conditions, ABZ permeation might be enhanced by cell membrane damage due to reactive oxygen species (ROS) generation caused by ATV in cyst areas, from the aerobic respiratory chain, considering that complexes I, II, and III of the electron transport chain are reported to be the major sites of ROS production [15, 16]. The oxidation of either complex I or II substrates in the presence of complex III inhibitors increases the production of ROS [17, 18]. Damage to the respiratory chain by the excessive production of ROS leads to electron transfer dysfunction, which causes irreversible cell disorder. It is assumed that cellular dysfunction attributed to ROS contributed to the potentiating effect of ABZ under aerobic conditions. Additionally, under hypoxia, the efficacy of the treatment in vivo may be enhanced by the synergistic action of ABZ and ATV, as shown in the anaerobic culture assay. ATV inhibits not only complex III but also dihydroorotate dehydrogenase (DHODH), which has been annotated in the genome data of E. multilocularis [19] and other parasites [20, 21]. DHODH contributes to adaptation to anaerobiosis by regulating fumarate reductase activity and pyrimidine synthesis [22]. The dysfunction of anaerobic metabolism pathways may be synergistically induced by the inhibition of DHODH and the action of ABZ. However, little is known about the importance of DHODH in the biological functions of E. multilocularis.
Here, we focused on the culture assay and in vivo experiments. However, our study has limitations. First, the biochemical approach was not utilized to demonstrate the synergistic action and hypothesis mentioned above. Second, morphological and pathological changes were not observed through electron microscopy and tissue section of cysts before and after treatment. Further studies will demonstrate the role of ATV and ABZ in the enhancement of potency in the aerobic and anaerobic metabolic pathway.
In conclusion, compared with ABZ alone, combined treatment with ABZ and ATV reduced the area of larval cysts in mouse liver significantly. This finding can provide ideas for further study of the treatment of and drug development for E. multilocularis infection.
Data availability
Not applicable
References
Wen H, Vuitton L, Tuxun T, Li J, Vuitton DA, Zhang W, McManus DP (2019) Echinococcosis: advances in the 21st century. Clin Microbiol Rev 32: e00075-18. 10.1128/CMR.00075-18.
Mihmanli M, Idiz UO, Kaya C, Demir U, Bostanci O, Omeroglu S, Bozkurt E (2016) Current status of diagnosis and treatment of hepatic echinococcosis. World J. Hepatol. 8:1169–1181. https://doi.org/10.4254/wjh.v8.i28.1169
Reuter S, Buck A, Manfras B, Kratzer W, Seitz HM, Darge K, Reske SN, Kern P (2004) Structured treatment interruption in patients with alveolar echinococcosis. Hepatology 39:509–517. https://doi.org/10.1002/hep.20078
Siles-Lucas M, Casulli A, Cirilli R, Carmena D (2018) Progress in the pharmacological treatment of human cystic and alveolar echinococcosis: compounds and therapeutic targets. PLoS Negl Trop Dis 12:e0006422. https://doi.org/10.1371/journal.pntd.0006422
Enkai S, Inaoka DK, Kouguchi H, Irie T, Yagi K, Kita K (2020) Mitochondrial complex III in larval stage of Echinococcus multilocularis as a potential chemotherapeutic target and in vivo efficacy of atovaquone against primary hydatid cysts. Parasitol Int 75:102004. https://doi.org/10.1016/j.parint.2019.102004
Matsumoto J, Sakamoto K, Shinjyo N, Kido Y, Yamamoto N, Yagi K, Miyoshi H, Nonaka N, Katakura K, Kita K, Oku Y (2008) Anaerobic NADH-fumarate reductase system is predominant in the respiratory chain of Echinococcus multilocularis, providing a novel target for the chemotherapy of alveolar echinococcosis, Antimicrob. Agents Chemother 52:164–170. https://doi.org/10.1128/AAC.00378-07
Enkai S, Sakamoto K, Kaneko M, Kouguchi H, Irie T, Yagi K, Matsumoto J, Oku Y, Katakura K, Fujita O, Nozaki T, Kita K (2017) Medical treatment of Echinococcus multilocularis and new horizons for drug discovery: characterization of mitochondrial complex II as a potential drug target, In: Echinococcosis (Tnay Inceboz, ed.). InTechOpen, https://doi.org/10.5772/intechopen.68565.
Takamiya S, Fukuda K, Nakamura T, Aoki T, Sugiyama H (2010) Paragonimus westermani possesses aerobic and anaerobic mitochondria in different tissues, adapting to fluctuating oxygen tension in microaerobic habitats. Int J Parasitol 40:1651–1658. https://doi.org/10.1016/j.ijpara.2010.07.009
Iwata F, Shinjyo N, Amino H, Sakamoto K, Islam M.K, Tsuji N, Kita K. (2008) Change of subunit composition of mitochondrial complex II (Succinate-ubiquinone reductase/Quinol-fumarate reductase) in Ascaris suum during the migration in the experimental host. Parasitol. Int 57:54–61. https://doi.org/10.1016/j.parint.2007.08.002.
Cwiklinski K, Jewhurst H, McVeigh P, Barbour T, Maule AG, Tort J, O’Neill SM, Robinson MW, Donnelly S, Dalton JP (2018) Infection by the helminth parasite Fasciola hepatica requires rapid regulation of metabolic, virulence, and invasive factors to adjust to its mammalian host. Mol. Cell. Proteomics:17792–17809. https://doi.org/10.1074/mcp.RA117.000445
Müller M, Mentel M, van Hellemond JJ, Henze K, Woehle C, Gould SB, Yu, RY van der Giezen M, Tielens AG, Martin WF (2012) Biochemistry and evolution of anaerobic energy metabolism in eukaryotes. Microbiol. Mol. Biol 76: 444–495, https://doi.org/10.1128/MMBR.05024-11.
Nakaya K, Oomori Y, Kutsumi H, Nakao M (1998) Morphological changes of larval Echinococcus multilocularis in mice treated with albendazole or mebendazole. J. Helminthol 72:349–354
Kanda Y (2013) Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant 48:452–458. https://doi.org/10.1038/bmt.2012.244
Patel K, Doudican NA, Schiff PB, Orlow SJ (2011) Albendazole sensitizes cancer cells to ionizing radiation. Radiat Oncol 17:160. https://doi.org/10.1186/1748-717X-6-160
Chen Q, Vazquez EJ, Moghaddas S, Hoppel CL, Lesnefsky EJ (2003) Production of reactive oxygen species by mitochondria: central role of complex III. J Biol Chem 278:36027–36031. https://doi.org/10.1074/jbc.M304854200
De Sarkar S, Sarkar D, Sarkar A, Dighal A, Staniek K, Gille L, Chatterjee M (2019) Berberine chloride mediates its antileishmanial activity by inhibiting Leishmania mitochondria. Parasitol Res 118:335-45. https://doi.org/10.1007/s00436-018-6157-3.
Liu R, Cao P, Ren A, Wang S, Yang T, Zhu T, Shi L, Zhu J, Jiang AL, Zhao MW (2018) SA inhibits complex III activity to generate reactive oxygen species and thereby induces GA overproduction in Ganoderma lucidum. Redox Biol 16:388–400. https://doi.org/10.1016/j.redox.2018.03.018
Siebels I, Dröse S (2013) Q-site inhibitor induced ROS production of mitochondrial complex II is attenuated by TCA cycle dicarboxylates. Biochim Biophys Acta 1827:1156–1164. https://doi.org/10.1016/j.bbabio.2013.06.005
Tsai IJ, Zarowiecki M, Holroyd N, Garciarrubio A, Sanchez-Flores A, Brooks KL, Tracey A, Bobes RJ, Fragoso G, Sciutto E, Aslett M, Beasley H, Bennett HM, Cai J, Camicia F, Clark R, Cucher M, De Silva N, Day TA,Deplazes P, Estrada K, Fernández C, Holland PW, Hou J, Hu S, Huckvale T, Hung SS, Kamenetzky L, Keane JA, Kiss F, Koziol U, Lambert O, Liu K, Luo X, Luo Y, Macchiaroli N, Nichol S, Paps J, Parkinson J, Pouchkina-Stantcheva N, Riddiford N, Rosenzvit M, Salinas G, Wasmuth JD, Zamanian M, Zheng Y, Cai X, Soberón X, Olson PD, Laclette JP, Brehm K, Berriman M (2013) The genomes of four tapeworm species reveal adaptations to parasitism. Nature 496:57–63, https://doi.org/10.1038/nature12031.
de Mori RM, Aleixo MAA, Zapata LCC, Calil FA, Emery FS, Nonato MC (2020) Structural basis for the function and inhibition of dihydroorotate dehydrogenase from Schistosoma mansoni. FEBS J. https://doi.org/10.1111/febs.15367.
Kamyingkird K, Cao S, Tuvshintulga B, Salama A, Mousa AA, Efstratiou A, Nishikawa Y, Yokoyama N, Igarashi I, Xuan X (2017) Effects of dihydroorotate dehydrogenase (DHODH) inhibitors on the growth of Theileria equi and Babesia caballi in vitro. Exp Parasitol 176:59–65. https://doi.org/10.1016/j.exppara.2017.03.002
Annoura T, Nara T, Makiuchi T, Hashimoto T, Aoki T (2005) The origin of dihydroorotate dehydrogenase genes of kinetoplastids, with special reference to their biological significance and adaptation to anaerobic, parasitic conditions. J Mol Evol 60:113–127. https://doi.org/10.1007/s00239-004-0078-8
Acknowledgements
We wish to thank a grant from JSPS KAKENHI (grant number 17K08815) to Hirokazu Kouguchi, 20K06402 for Kinpei Yagi, and from Research Program on Emerging and Re-emerging Infectious Diseases (17fk0108119j0001) to Kiyoshi Kita for the financial support. We would like to thank Editage (www.editage.com) for English language editing.
Code availability
Not applicable
Funding
This study was funded by JSPS KAKENHI (grant numbers 17K08815 and 20K06402) to Hirokazu Kouguchi and Kinpei Yagi and Research Program on Emerging and Re-emerging Infectious Diseases (17fk0108119j0001) to Kiyoshi Kita.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection and analysis were performed by Shigehiro Enkai, Hirokazu Kouguchi, Daniel Ken Inaoka, Takao Irie, Kinpei Yagi, and Kiyoshi Kita. The first draft of the manuscript was written by Shigehiro Enkai, and all authors commented on previous versions of the manuscript. All authors also read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The procedures in this manuscript are in strict accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals. In addition, the protocol for animal experiments was approved by the ethics committee of the Hokkaido Institute of Public Health (permit numbers: K25-2 and K29-4).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Enkai, S., Kouguchi, H., Inaoka, D.K. et al. In vivo efficacy of combination therapy with albendazole and atovaquone against primary hydatid cysts in mice. Eur J Clin Microbiol Infect Dis 40, 1815–1820 (2021). https://doi.org/10.1007/s10096-021-04230-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-021-04230-5