Abstract
Almost a decade ago our diagnostic laboratory implemented an in-house real-time PCR for the detection of Plasmodium DNA to diagnose malaria in parallel with conventional diagnostics, i.e., microscopy (thick and thin smears), quantitative buffy coat microscopy (QBC), and a rapid diagnostic test (RDT). Here we report our experiences and make a comparison between the different diagnostic procedures used in this non-endemic setting. All patients during the period February 2009–December 2017 suspected of malaria were prospectively tested at the moment of sample collection. Both PCR and conventional malaria diagnostics were carried out on a total of 839 specimens from 825 patients. In addition, three Plasmodium falciparum (Pf) patients were closely followed by real-time PCR and microscopy after treatment. Overall, 56 samples (55 patients) tested positive by real-time PCR, of which six were missed by microscopy and seven by QBC. RDT showed fairly good results in detecting Pf, whereas specificity was not optimal. RDT failed to detect 10 of 17 non-Pf PCR positive specimens. One Plasmodium malariae patient would have been missed if only conventional diagnostic tests had been used. The high sensitivity of the PCR was confirmed by the number of PCR positive, microscopy negative post-treatment samples. In conclusion, within our routine diagnostic setting, malaria real-time PCR not only showed a high level of agreement with the conventional methods used, but also showed higher sensitivity and better specificity. Still, for complete replacement of the conventional procedures in a non-endemic setting, the time-to-results of the real-time PCR is currently too long.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malaria is an infectious disease caused by Plasmodium parasites, which are transmitted by Anopheles mosquitoes in tropical and subtropical areas. The disease has a substantial impact on people’s health and life, not only in endemic areas, but also in travelers and migrants. Estimates of the World Health Organization (WHO) reported 216 million cases globally in 2016, leading to 445,000 deaths [1]. In the Netherlands, approximately 300 new malaria cases are reported each year; while many more potential cases are seen because a traveler or migrant shows clinical symptoms after being exposed in a malaria-endemic region [2]. Today, five different species of Plasmodium are known to cause disease in humans: Plasmodium falciparum (Pf), Plasmodium vivax (Pv), Plasmodium ovale (Po), Plasmodium malariae (Pm), and Plasmodium knowlesi (Pk). It has been recognized that Plasmodium ovale are in fact two closely related species: Plasmodium ovale curtisi (Po-c) and Plasmodium ovale wallikeri (Po-w) [3]. Pf is found most frequently worldwide and is the species responsible for most of the global morbidity and mortality due to malaria [1].
To diagnose a Plasmodium sp. infection, whole blood is drawn from a patient and assessed for the presence of Plasmodium parasites. In non-endemic countries, a combination of microscopy (thick and thin smears) and a rapid diagnostic test (RDT) is commonly used as first-line malaria diagnosis. Although microscopy is relatively inexpensive to perform and enables species differentiation and determination of parasitemia (parasite density), it is a subjective and labor intense procedure which needs well-trained personnel to achieve optimal results. The limit of detection (LoD) of Giemsa-stained thick blood film has been estimated to be 5–50 parasites/μl (p/μl) [4, 5]. The main advantage of RDTs is the simplicity in use and interpretation, as well as the short time to result (~ 5–20 min). In general, RDTs show good sensitivity for detection of Pf, whereas sensitivity in detecting other Plasmodium species is limited. In a laboratory-based evaluation of RDT performance, as performed by the WHO, including 46 different RDT products, the median panel detection score (the ability to detect Plasmodium parasites at a certain concentration) for Pf at a low concentration (200 p/μl) was 89.5%. [6]
To extend the diagnostic possibilities, a quantitative buffy coat microscopy (QBC) test for rapid diagnosis of malaria can be used as well. This technique is, in general, substantially faster than conventional microscopy by a thick smear examination, but also needs more training for appropriate reading and interpretation [7].
Although not widely used as a routine diagnostic tool in a clinical setting, nucleic acid amplification testing (NAAT) for the detection of Plasmodium DNA can be performed either by using real-time PCR or loop-mediated isothermal amplification (LAMP) [8, 9]. NAAT provides a limit of detection that is at least tenfold better than an experienced microscopist, and improved detection of mixed infections. Although quantification by NAAT is possible by determining the concentration of parasites per microliter, parasitemia is still established by microscopy. In non-endemic countries, this is commonly done by counting the percentage of infected red blood cells in a thin smear [4].
In our routine diagnostic laboratory, an in-house multiplex real-time PCR assay for the detection of the four most common Plasmodium species was introduced as a first line diagnostic test for malaria almost a decade ago. Since then, all first-blood specimens obtained from patients suspected of malaria have, in principle, been examined by all available conventional methods, i.e., thick smear microscopy, QBC and RDT, as well as by real-time PCR. Here we report the results of a comparative analysis of the malaria diagnostic procedures used and discuss which approach is most efficient in a routine diagnostic setting in a non-endemic malaria region.
Materials and methods
Specimens and inclusion
Whole blood specimens drawn from patients suspected of malaria during the period February 2009–December 2017 were tested at the clinical microbiology laboratory of the Leiden University Medical Center (LUMC) in the Netherlands. Per episode of suspected malaria, only the first specimen per patient had been examined by all available diagnostic procedures, i.e., microscopy (thick/thin smear), QBC, RDT, and real-time PCR. Only specimens that showed valid results for all assays were included in the comparative analysis. Arbitrarily, when a new specimen was received of a patient more than 3 months after the first specimen, without continuous follow-up during this time, it was considered a new episode of suspected malaria. Hence, these specimens were included in the present study as well. When multiple specimens were obtained from a single patient within the given timeframe of 3 months while different Plasmodium species were identified, additional specimens were also included.
Series of post-malaria treatment follow-up samples were available from three Pf patients. These patients were selected because of the high number of follow-up samples (5 to 12), which therefore could be used to further examine the association between parasite density (parasitemia) as determined by microscopy and the cycle of quantification (Cq-value) as determined by real-time PCR. All three cases had a severe clinical presentation, which explains the intense sampling and the prolonged presence of the parasite in the blood circulation. These follow-up samples were not collected systematically, but as determined by the clinical specialist in charge, based on the clinical conditions of the patient.
All data used for this study were retrieved from the laboratory information management system (LIMS) of our department. A patient and corresponding diagnostic data was included only if the patient had not specifically indicated that sample material and data could not be used for other purposes than diagnosis of disease, as regulated by law and stated in “Human tissue and medical research: code of conduct for responsible use” (2011).
Microscopy
For thick smear analysis, 15 μl of whole blood was spread onto a slide and stained with Giemsa, followed by microscopic examination by two technicians. If parasites were detected, the Plasmodium species was determined and parasitemia was calculated in Pf and Pk positive cases according to the Dutch national standard procedures using thin smear microscopy.
QBC was performed using the QBC Malaria test (Drucker Diagnostics, Port Matilda, PA, USA) followed by fluorescent microscopic examination, according to the manufacturer’s instructions. In short, an acridine orange-coated microhematocrit tube was filled with blood, sealed after gently mixing and subsequently centrifuged for 5 min at 12,000 rpm. Depending on the stage of Plasmodium present, the parasite stains green and orange under the fluorescent microscope because of the uptake of the dye [7].
Rapid diagnostic testing
The Binax NOW malaria immune chromatography test (RDT, Alere, Tilburg, Netherlands) was used for rapid diagnostic testing according to the manufacturer’s instructions. The test can detect and differentiate between Pf and Plasmodium species by targeting HRP2, specific to Pf, and pan-malarial aldolase [4].
Real-time PCR
DNA extraction was performed using the QIAamp DNA blood mini kit (Qiagen, Venlo, Netherlands) and, as of February 2016, the MagnaPure96 platform with the DNA and Viral NA Small volume kit 2.0 (Roche Diagnostics, Almere, Netherlands). Both DNA extraction methods used 200 μl of whole blood yielding a final NA eluate of 100 μl. To monitor the extraction process and the presence of potential PCR inhibitors, an aliquot of Phocine Herpes Virus (PhHV) was co-amplified as universal internal control. Real-time PCR was introduced in February 2009 and was tested in one multiplex assay in a 50 μl reaction volume using primers and probes as described previously and summarized in Table 1 [9,10,11]. Since February 2014, amplification reactions were performed in a volume of 25 μl including 12.5 μl Hotstar mastermix (Qiagen, Venlo, Netherlands), supplemented with 1.75 mM MgCl2 and primers/probes according to Table 1. Amplification was performed using the CFX real-time detection system (Bio-Rad laboratories, Veenendaal, Netherlands) and the following thermal profile: 15 min at 95 °C, followed by 45 cycles of 30 s at 95 °C, 30 s at 55 °C, and 30 s at 72 °C. No additional testing of Po was done in order to differentiate between Po-c and Po-w. In each run, negative and positive extraction controls were included, and real-time PCR was only interpreted when all controls showed results within the defined acceptance criteria. A sample was considered inhibited if the Cq-value of PhHV in the sample was > 3Cq points higher than the Cq-value of PhHV in the negative control and re-tested using a one in ten dilution of the eluate. A sample was reported as inhibited, and therefore excluded for comparison, when inhibition was observed upon re-testing.
Results
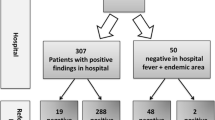
A total of 839 specimens obtained from 825 patients were included for comparison of the diagnostic outcome. As shown in Table 2, real-time PCR tested positive in 56 specimens that were collected from 55 patients. Two specimens of one patient were included since real-time PCR tested positive for Pf (November 2016) and subsequently for Po (January 2017). Overall, the 56 real-time PCR positive specimens included 39 Pf (median Cq-value 23.2, range 13.0–37.2), 6 Pv (median Cq-value 19.9, range 18.9–24.6), 7 Po (median Cq-value 25.9, range 25.1–31.9), and 4 Pm (median Cq-value 28.9, range 23.2–33.6). No Pk (microscopy) or mixed infections (microscopy or PCR) were found in the examined specimens. Thirty-five (89.7%) of 39 Pf PCR positive blood samples were found positive with thick smear microscopy, 34 (87.2%) by QBC, and 37 (94.9%) by RDT. All Pv and Po PCR positive specimens were identified using conventional microscopy, whereas microscopy detected only two of four Pm PCR positive specimens. Plasmodium was detected with QBC in all Pv and Po cases, but missed half of the Pm PCR positive samples. Pan-malarial aldolase was detected in the RDT in 7 of 17 non-Pf cases.
In-depth analysis of the mismatching data showed the following. In the four Pf PCR positive samples with a negative thick smear microscopy, Cq-values ranged from 31.1–37.2. One of these specimens (Cq-value of 33.3) tested negative by RDT. For this patient, originating from Sierra Leone, no information was available regarding a possible earlier infection or prior testing. While the QBC was reported negative for trophozoites, one single gametocyte was observed. Although a follow-up sample was requested by the clinical consultant, the patient did not show-up the following day and was therefore lost to follow-up. The three remaining Pf PCR positive patients tested negative in thick smear and QBC microscopy but showed a positive RDT result. All three patients had already been diagnosed as being Pf positive and had therefore been treated with anti-malarial therapy. Their pre-treatment samples were not included in this comparative analysis, as the QBC was not performed. The two Pm PCR positive samples were not only negative in thick smear microscopy, but also in the QBC, and RDT. Of one patient (Cq-value 30.2), a second specimen was obtained three days later and tested again Pm PCR positive (Cq-value 39.1). This patient had just returned from Tanzania and had locally received an anti-malarial treatment approximately a week before, because of high fever. The second Pm PCR positive patient (Cq-value 33.6), was not previously known to be positive. A second specimen was obtained 5 days later and again tested Pm positive in the real-time PCR assay (Cq-value 32.1). After extensive microscopic examination of multiple thick smear preparations, a few Pm schizonts and merozoites were found.
Seven patients tested positive by at least one of the conventional methods, but remained negative in real-time PCR. Six of the samples tested positive in RDT only and not in any of the other conventional tests. One of them was known to have been treated for malaria recently; the remaining five had no history of malaria infection. One patient tested negative in real-time PCR, while being positive in thick smear, QBC, and RDT. Again, this patient was known to have been treated for malaria recently.
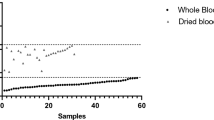
Three Pf patients were closely followed after anti-malarial treatment. These series (6–13 samples) were analyzed by conventional microscopy as well as real-time PCR (Fig. 1A–C). In all three cases, microscopy became negative before PCR, with the first microscopy negative sample showing Cq-value of 28.2, 31.1, and 31.2, respectively (Fig. 1A–C). All PCR positive samples in this series with a Cq-value higher than 30 were microscopy negative.
Microscopy (parasitemia) versus real-time PCR (Cq-value) in 3 (A, B and C) P. falciparum positive patients with follow-up samples after malaria treatment. Parasitemia in percentages (gray) is extrapolated on the right side, Cq-value (black) on the left side. On the horizontal axes, the date of sample collection is shown. A high Cq-value represents low Plasmodium DNA levels. A negative outcome is illustrated as Cq-value 45
Discussion
Here we present comparative data of almost 9 years of prospective testing by real-time PCR for the detection of Pf, Pv, Po, and Pm DNA in parallel with conventional malaria diagnostic methods. The real-time PCR assay was developed, validated, and approved for routine diagnostic use in 2009. Over the years, some minor changes in the DNA extraction method and in the volume of the PCR assay have been integrated following extensive in-house validation procedures. These adaptations did not change the analytical sensitivity of the assay (data not shown). Overall, we found reasonable agreement between the performance of real-time PCR and thick smear microscopy. Also the QBC performed well, although one Pf PCR (Cq 28.1) and thick smear positive sample was missed. This sample also tested positive in the RDT. A follow-up specimen of this patient tested positive in the QBC and it is not clear why the initial QBC was found to be negative.
As for the thick smear microscopy, the RDT also showed acceptable results for the detection of Pf in comparison to the real-time PCR assay, with 94.9% of the PCR positive specimens being RDT positive. However, one should be aware of the fact that Pf variants are circulating in which HRP-2 is not present, yielding false-negative RDT results. Since the prevalence of HRP-2 lacking Pf variants is increasing, this could potentially be of risk for rapid and correct detection of this species using HRP-2-based assay formats [12].
Despite the adequate performance of the RDT in diagnosing Pf infections, the performance of the RDT in the non-falciparum species was poor, which has been reported by others before [5, 13, 14]. Although Pf is the most common species, the present study again shows that diagnosing malaria using RDT only is not sufficient.
Out of 56 real-time PCR positive specimens, six were found negative by thick smear microscopy and QBC. Five of these positive real-time PCR results were of little clinical significance, since four (three Pf and one Pm) were actually post malaria-treatment samples and the fifth sample (Pf) only contained a single Pf gametocyte, most likely from a patient without asexual reproducing stages. On the other hand, the sixth malaria PCR-positive patient (Pm) with negative microscopy was indeed of clinical significance. Here, no history of previous malaria infection or treatment was recorded and with only the real-time PCR being positive on the initial sample, this malaria infection would have been missed when only conventional methods would have been used.
For one patient, who had already been treated for a Plasmodium infection, PCR remained negative while microscopy (both thick smear and QBC) and RDT were found positive for Pf. Thick smear microscopy showed five trophozoites in total in two different slides. A follow-up specimen of this patient, collected 5 days later, only tested positive by the RDT. This result was in contrast with other specimens included in this study, in which it was shown that real-time PCR can detect Pf in treated patients that tested negative in the thick smear microscopy. Testing the initial specimen by a nested Plasmodium genus PCR assay also remained negative.
RDT alone tested (weakly) positive in six patients. One of them had been recently treated for malaria, and therefore persistence of HRP-2 or aldolase in blood may have resulted in prolonged positivity of RDTs [5]. However, the remaining five patients had no history of malaria infection. False-positive results may be caused by, for instance, rheumatoid factor in blood and heterophile antibodies [14]. We therefore conclude that the RDT positive results which could not be confirmed by any of the other diagnostic tests were most likely either due to prolonged circulation of HRP-2 or cross-reaction with other immunological factors.
In the present study, multiple specimens were obtained from three patients following anti-malarial treatment. By using all of these specimens, the analytical sensitivity of conventional microscopy and real-time PCR could be compared. This evaluation showed higher sensitivity of real-time PCR, since Pf DNA could still be detected while microscopy became negative. This is in line with earlier studies that showed that PCR-based assays were found to be more sensitive than conventional methods [15]. Nevertheless, it should be mentioned that false-positive signals because of detection of remnant genetic material could not be ruled out. To determine a formal cut-off Cq-value as of which microscopy becomes negative, one should perform more extensive testing of both methods using a dilution series of a reference strain. Nevertheless, in our setting, we found microscopy to be negative when the real-time PCR showed a Cq-value of 30 or above.
During the 9 year period that the PCR had been used, mixed infections were noticed in four patients: one Pf/Pv and three Pf/Pm. Unfortunately, none of these cases could be included in the current comparative study. From three of these patients, we only received a little blood from an external laboratory for species confirmation by PCR only. The remaining case was a mixed infection found in a young child. While thick smear microscopy showed a Pm infection and the RDT indicated a Pf infection, real-time PCR identified a mixed infection of both species. No QBC was performed. This particular finding has been reported elsewhere [16]. Although these results showed that mixed infections are very rare in the Netherlands, it demonstrated the added value of real-time PCR being able to discriminate between Plasmodium species and identify mixed infections. Similarly, in a recent study, Grossman et al. even reported ten cases with mixed infections by real-time PCR of which only one could be identified by microscopy and RDT [17].
Obviously, this is not the first study comparing the performance of malaria (real-time) PCR with conventional diagnostic methods. Already in 2008, Berry et al. reviewed the literature and concluded that PCR-based methods should be included in the panel of diagnostic tools for imported malaria, given its high sensitivity and specificity [15]. Two more recent studies, conducted in Israel and Italy, confirmed the excellent diagnostic performance of real-time PCR in a non-endemic setting [17, 18]. Still, despite the high negative predictive value of molecular testing, the majority of laboratories in non-endemic settings do not use PCR as a first line diagnosis for all their malaria suspected cases. This attitude toward molecular diagnosis of imported malaria might change rapidly in the coming years with the introduction of simplified test procedures, such as the Illumigene loop-mediated isothermal amplification (LAMP) malaria assay, which makes it possible to perform molecular diagnostic testing 24/7 without the need of advanced laboratory equipment or high levels of expertise [8]. Preferably these tests have a quantitative output and can differentiate Plasmodium parasites at species level.
In conclusion, we found satisfactory results with the implementation of an in-house malaria multiplex real-time PCR within our routine non-endemic diagnostic setting, showing high sensitivity and specificity with the additional advantage of more accurate species differentiation and the indication of parasite load, as reflected by Cq-value. The major reason for not fully replacing existing conventional methods with this real-time PCR is the longer “time to results” period of the PCR. Most likely these technical aspects will further improve in the near future.
References
Anonymous (2017) World malaria report. World Health Organization, Geneva, p 2017
de Gier B, Suryapranata FS, Croughs M, van Genderen PJ, Keuter M, Visser LG, van Vugt M, Sonder GJ (2017) Increase in imported malaria in the Netherlands in asylum seekers and VFR travellers. Malar J 16:60
Sutherland CJ, Tanomsing N, Nolder D, Oguike M, Jennison C, Pukrittayakamee S, Dolecek C, Hien TT, do Rosario VE, Arez AP, Pinto J, Michon P, Escalante AA, Nosten F, Burke M, Lee R, Blaze M, Otto TD, Barnwell JW, Pain A, Williams J, White NJ, Day NP, Snounou G, Lockhart PJ, Chiodini PL, Imwong M, Polley SD (2010) Two nonrecombining sympatric forms of the human malaria parasite Plasmodium ovale occur globally. J Infect Dis 201:1544–1550
Chiodini PL (2014) Malaria diagnostics: now and the future. Parasitology 141:1873–1879
Wongsrichanalai C, Barcus MJ, Muth S, Sutamihardja A, Wernsdorfer WH (2007) A review of malaria diagnostic tools: microscopy and rapid diagnostic test (RDT). Am J Trop Med Hyg 77:119–127
WHO (2017) Results of WHO product testing of malaria RDTs: round 7 (2015–2016)
Prashanth GP (2012) Quantitative buffy coat (QBC) test for rapid diagnosis of malaria. Eur J Pediatr 171:199–200
De Koninck AS, Cnops L, Hofmans M, Jacobs J, Van den Bossche D, Philippe J (2017) Diagnostic performance of the loop-mediated isothermal amplification (LAMP) based illumigene((R)) malaria assay in a non-endemic region. Malar J 16:418
Wiria AE, Prasetyani MA, Hamid F, Wammes LJ, Lell B, Ariawan I, Uh HW, Wibowo H, Djuardi Y, Wahyuni S, Sutanto I, May L, Luty AJ, Verweij JJ, Sartono E, Yazdanbakhsh M, Supali T (2010) Does treatment of intestinal helminth infections influence malaria? Background and methodology of a longitudinal study of clinical, parasitological and immunological parameters in Nangapanda, Flores, Indonesia (ImmunoSPIN study). BMC Infect Dis 10:77
Muller-Stover I, Verweij JJ, Hoppenheit B, Gobels K, Haussinger D, Richter J (2008) Plasmodium malariae infection in spite of previous anti-malarial medication. Parasitol Res 102:547–550
Shokoples SE, Ndao M, Kowalewska-Grochowska K, Yanow SK (2009) Multiplexed real-time PCR assay for discrimination of Plasmodium species with improved sensitivity for mixed infections. J Clin Microbiol 47:975–980
Berhane A, Anderson K, Mihreteab S, Gresty K, Rogier E, Mohamed S, Hagos F, Embaye G, Chinorumba A, Zehaie A, Dowd S, Waters NC, Gatton ML, Udhayakumar V, Cheng Q, Cunningham J (2018) Major threat to malaria control programs by Plasmodium falciparum lacking histidine-rich protein 2, Eritrea. Emerg Infect Dis 24:462–470
Maltha J, Gillet P, Jacobs J (2013) Malaria rapid diagnostic tests in travel medicine. Clin Microbiol Infect 19:408–415
Mouatcho JC, Goldring JP (2013) Malaria rapid diagnostic tests: challenges and prospects. J Med Microbiol 62:1491–1505
Berry A, Benoit-Vical F, Fabre R, Cassaing S, Magnaval JF (2008) PCR-based methods to the diagnosis of imported malaria. Parasite 15:484–488
Terveer EM, Brienen EAT, Erkens MAA, van Lieshout L (2016) Late manifestation of a mixed Plasmodium falciparum and Plasmodium malariae infection in a non-immune toddler after traveling to Chad. Travel Med Infect Dis 14:533–534
Grossman T, Schwartz E, Vainer J, Agmon V, Glazer Y, Goldmann D, Marva E (2017) Contribution of real-time PCR to Plasmodium species identification and to clinical decisions: a nationwide study in a non-endemic setting. Eur J Clin Microbiol Infect Dis 36:671–675
Calderaro A, Piccolo G, Montecchini S, Buttrini M, Rossi S, Dell'Anna ML, De Remigis V, Arcangeletti MC, Chezzi C, De Conto F (2018) High prevalence of malaria in a non-endemic setting: comparison of diagnostic tools and patient outcome during a four-year survey (2013-2017). Malar J 17:63
Acknowledgments
We would like to thank the technicians of the clinical microbiology laboratory of the LUMC for performing the conventional and molecular diagnostics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Nijhuis, R.H.T., van Lieshout, L., Verweij, J.J. et al. Multiplex real-time PCR for diagnosing malaria in a non-endemic setting: a prospective comparison to conventional methods. Eur J Clin Microbiol Infect Dis 37, 2323–2329 (2018). https://doi.org/10.1007/s10096-018-3378-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3378-4