Abstract
The tick-borne bacterium Candidatus (Ca.) Neoehrlichia (N.) mikurensis is a cause of “fever of unknown origin” because this strict intracellular pathogen escapes detection by routine blood cultures. Case reports suggest that neoehrlichiosis patients may display serological reactivity to Anaplasma (A.) phagocytophilum. Since Anaplasma serology is part of the diagnostic work-up of undetermined fever in European tick-exposed patients, we wanted to investigate (1) the prevalence of A. phagocytophilum seropositivity among neoehrlichiosis patients, (2) the frequency of misdiagnosed neoehrlichiosis patients among A. phagocytophilum seropositive patients, and (3) the frequency of A. phagocytophilum and Ca. N. mikurensis co-infections. Neoehrlichiosis patients (n = 18) were analyzed for A. phagocytophilum IgM and IgG serum antibodies by indirect immunofluorescence assay. Serum samples from suspected anaplasmosis patients (n = 101) were analyzed for bacterial DNA contents by singleplex PCR specific for A. phagocytophilum and Ca. N. mikurensis, respectively. One fifth of the neoehrlichiosis patients (4/18) were seropositive for IgM and/or IgG to A. phagocytophilum at the time of diagnosis. Among the patients with suspected anaplasmosis, 2% (2/101) were positive for Ca. N. mikurensis by PCR whereas none (0/101) had detectable A. phagocytophilum DNA in the serum. To conclude, patients with suspected anaplasmosis may in fact have neoehrlichiosis. We found no evidence of A. phagocytophilum and Ca. N. mikurensis co-infections in humans with suspected anaplasmosis or confirmed neoehrlichiosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Candidatus (Ca.) Neoehrlichia (N.) mikurensis is a tick-borne pathogen found in Europe and Asia [1], which was first reported to be a human pathogen in 2010 [2,3,4]. It can give rise to a severe infectious disease named neoehrlichiosis that features fever and vascular events in immunocompromised patients [5]. Immunocompetent individuals infected by Ca. N. mikurensis may present with fever and symptoms indicative of systemic infection, isolated erythematous skin rashes, or no symptoms at all [2, 4, 6,7,8,9].
Like all members of the Anaplasmataceae family, Ca. N. mikurensis is a strict intracellular pathogen, and consequently does not grow in cell-free media, which is why it escapes detection by routine blood cultures [1]. At present, the only microbiological diagnostic option is PCR since there are no serological assays available. The restricted diagnostic alternatives, together with the novelty of this emerging pathogen, explain why many patients with severe neoehrlichiosis remain undiagnosed and fall under the epithet of “fever of unknown origin” [5]. In central and northern Europe, A. phagocytophilum serology is part of the diagnostic work-up of (tick-exposed) patients with unexplained fever. There are at least three case reports of immunocompetent patients infected by Ca. N. mikurensis who were seropositive for A. phagocytophilum as determined by indirect immunofluorescence assay (IFA): two of the cases had de novo production of Anaplasma-reactive antibodies, whereas the third one had pre-existing antibodies [2, 6]. This might indicate that Ca. N. mikurensis infection can trigger the production of Anaplasma cross-reactive antibodies or the occurrence of double infections with Ca. N. mikurensis and A. phagocytophilum. Consequently, neoehrlichiosis patients may be wrongly diagnosed with anaplasmosis. The aims of this study were to address these issues. Specifically, the goals were to investigate (1) the prevalence of Anaplasma seropositivity among patients diagnosed with neoehrlichiosis, (2) whether neoehrlichiosis patients are misdiagnosed as anaplasmosis patients based on serological findings, and (3) the existence of A. phagocytophilum and Ca. N. mikurensis co-infections.
Methods
Study subjects
Eighteen patients diagnosed with neoehrlichiosis based on PCR-positive blood samples were investigated for A. phagocytophilum-reactive antibodies in serum (Table 1). Clinical data pertaining to some of these patients have been published previously [3, 5, 10,11,12]. Serum samples derived from a total of 101 anonymous patients queried for A. phagocytophilum antibodies were analyzed by PCR for the presence of bacterial DNA corresponding to Ca. N. mikurensis and A. phagocytophilum, respectively. The sera were obtained from three clinical microbiology laboratories, two in Sweden (Sahlgrenska University Hospital in Göteborg, n = 68, and Ryhov County Hospital in Jönköping, n = 22), and one in Denmark (Statens Serum Institut in Copenhagen, n = 11). These laboratories are the only ones that perform serological analyses of human antibodies to A. phagocytophilum in Sweden and Denmark, respectively. Over half of the blood samples submitted to Sahlgrenska University Hospital (38/68) for analysis of A. phagocytophilum antibodies and Ca. N. mikurensis DNA were from a prospective study on human tick-borne infections conducted at the Center of Vector-borne Infections, Uppsala University Hospital, Sweden. The study was approved by the local Ethical Review Boards of Göteborg and Uppsala, Sweden. All analyses were performed on thawed blood samples that had been stored frozen at either − 20 °C (sera tested for A. phagocytophilum antibodies) or − 120 °C (plasma from neoehrlichiosis patients).
A. phagocytophilum serology
A commercial IFA assay for analysis of IgG and IgM antibodies to a human isolate of A. phagocytophilum (Focus Diagnostics, Cypress, CA, USA) was used according to the manufacturer’s recommendations. Semi-quantitative endpoint antibody titers were obtained by serial twofold dilutions of reactive serum or EDTA-plasma samples. IgM titers ≥ 1:20 were regarded as positive. IgG titers of ≥ 1:64 were regarded as positive at Sahlgrenska University Hospital and Statens Serum Institut in Copenhagen, whereas a cutoff of ≥ 1:80 was employed at Ryhov Hospital in Jönköping using the same assay.
Ca. N. mikurensis PCR
Bacterial DNA was robot extracted (MagNA Pure Compact Extraction Robot, Roche, Basel, Switzerland) from 400 μL of serum or EDTA-plasma (Nucleic Acid Isolation Kit I, Roche) and analyzed by using a real-time TaqMan PCR specific for a 169-bp segment of the groEL gene of Ca. N. mikurensis as previously described [6]. A synthetic plasmid containing the 169-bp sequence cloned into a pUC57 vector (Genscript, Piscataway, NJ, USA) was used to establish a standard curve and the limit of detection, which was 1 × 103 copies/mL. All positive isolates were confirmed by 16S rRNA-PCR and sequenced [6].
A. phagocytophilum PCR
Bacterial DNA was extracted as described above and analyzed by using two different TaqMan real-time PCR assays: the first targeted the msp2 gene of A. phagocytophilum and was adapted from a duplex to a simplex assay [13]. The forward primer (5′-TTGGTCTTGAAGCGCTCGTA) and reverse primer (5′-AATACCATAACCAACACTGCCTTCCAT) generated a 77-bp fragment, which was detected with a TaqMan probe labeled with FAM (5′-CAATCTCAAGCTCAACCCTGGCACCA-MGB). The second PCR targeted the groEL gene of A. phagocytophilum [14]. The probe was modified to a TaqMan probe (5′FAM-TAACACACTGTGCAATCTTACT-MGB) and the PCR reaction generated a 61-bp-long fragment. Both PCR-reactions contained 1× FastStart Taqman Probe Master (Roche, Basel, Switzerland), 600 nM of each primer, 150 nM of probe, and 5 μL of DNA template. Real-time PCR was performed by using Rotorgene 6000 (QIAGEN, Hilden, Germany). Reaction conditions were 95 °C for 10 min, followed by 45 cycles at 95 °C for 15 s, and 56 °C (53 °C for groEL) for 1 min. The limit of detection for both assays was 1 × 104 copies/mL and was established using a synthetic plasmid (Genscript).
Results
Participants and study material
There were 18 neoehrlichiosis patients included in the study, all of whom were diagnosed by PCR analysis of blood samples (Table 1). The majority of the patients (17/18) was immunocompromised and had typical risk factors for severe neoehrlichiosis, e.g. an underlying hematologic or systemic autoimmune disease, splenectomy, rituximab treatment, chemotherapy, and/or systemic corticosteroids. Every one of the immunocompromised patients presented with febrile disease, but for one who suffered from nightly sweats and headache (SE16) (Table 1). All of the patients responded completely to treatment with doxycycline and cleared the infection with one exception (SE18), who was given 100 mg doxycycline for 10 days as empiric treatment for unexplained fever instead of the recommended dose of 200 mg doxycycline for 2–3 weeks [1]; the patient in question had PCR-positive and symptomatic recurrence of the infection about 40 days later.
In addition, clinical serum samples originating from 101 anonymous patients submitted to the three clinical laboratories that currently perform A. phagocytophilum serology in Sweden and Denmark were analyzed. Whereas the serum samples from County Hospital Ryhov (n = 22) and Statens Serum Institut (n = 11) were selected based on being positive for Anaplasma antibodies, those from Sahlgrenska University Hospital were mostly consecutive samples (n = 68) submitted to the laboratory for analysis of Anaplasma serology, of which 21 (31%) turned out to have an IgG titer of 1:64 or higher. The serum samples from Sahlgrenska University Hospital were obtained from patients aged between 19 and 80 with a median age of 58, with an even sex distribution (53% women), similar to the serum samples from County Hospital Ryhov (Jönköping), which were from patients 32 to 76 years old (median age 56 years; 45% women). The majority of the serum samples from Statens Serum Institut (Copenhagen) was from women (73%) having an age range of 27 to 67 years and a median age of 53 years.
A. phagocytophilum seropositivity among neoehrlichiosis patients
First, we investigated the blood samples from the 18 patients diagnosed with neoehrlichiosis regarding serologic reactivity to A. phagocytophilum. Four of the 18 patients (22%) were Anaplasma seropositive at the time of diagnosis (Table 2): the only immunocompetent patient included in the study and 3 out of the 17 who were immunocompromised. One patient had both IgM and IgG antibodies to Anaplasma and three had only IgG antibodies. All of the IgG titers were below 1:256.
Ca. N. mikurensis and A. phagocytophilum DNA in the blood of patients with suspected anaplasmosis
Two out of the 101 serum samples queried for Anaplasma antibodies were positive for Ca. N. mikurensis DNA by PCR (SE15 and SE18; Table 2). Both of these patients had typical symptoms of neoehrlichiosis and a characteristic risk profile (an underlying systemic autoimmune or hematologic disease, rituximab therapy, splenectomy) (Table 1). Neither of these two patients developed antibodies to A. phagocytophilum (Table 1). Moreover, not a single one of the 54 patients seropositive for A. phagocytophilum was positive in either of the two A. phagocytophilum PCRs (data not shown).
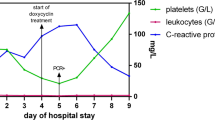
Kinetics of antibody levels to A. phagocytophilum in neoehrlichiosis patients
Repeated (paired) serum samples were only available from five of the neoehrlichiosis patients. Three of these patients (SE02, SE13, SE18) were seronegative for A. phagocytophilum on both sampling occasions. One patient developed IgM antibodies 1 week after diagnosis (NO01) that decreased 4-fold over a 5-week period (Fig. 1). Another patient (SE10) had IgG antibodies with a titer of 1:320 that was halved over a period of 41 days (Fig. 1).
Discussion
The main finding of this study is that every fifth of the neoehrlichiosis patients had low titers of A. phagocytophilum antibodies in the blood at the time of diagnosis. This is a surprisingly high figure in view of the fact that the majority of the patients were immunocompromised. This seroreactivity to A. phagocytophilum might represent (1) previous exposure to or infection with A. phagocytophilum, (2) co-infection with Ca. N. mikurensis and A. phagocytophilum, or (3) Anaplasma-crossreactive antibodies elicited or boosted by Ca. N. mikurensis infection.
Estimates of the seroprevalence of A. phagocytophilum antibodies in the general population in Scandinavia vary greatly. Two older studies report seroprevalence figures of 2.0 and 2.5% among Danish and Norwegian blood donors [15, 16], but a newer Norwegian study gives a figure of 16% [17]. The estimates of the A. phagocytophilum seroprevalence in populations that are heavily tick-exposed range from 10% in Norway [15], 11–17% in Sweden [18, 19], to 21% in Denmark [16]. It should be noted that the more recent seroepidemiologic surveys have utilized the same IFA as in the present study, which is based on a human isolate of A. phagocytophilum [16, 17, 19], whereas the older studies have used an equine A. phagocytophilum isolate [15, 18]. In contrast to the relatively high seroprevalence of A. phagocytophilum antibodies, there is a scarcity of case reports of anaplasmosis from the Scandinavian countries [20, 21]. The main explanation for this disparity is that the European variant of this infectious disease is relatively mild in humans, at least compared to human anaplasmosis in North America [22]. Presumably, the human-tropic European A. phagocytophilum strains are less virulent than the American ones and give rise to discrete symptoms or only subclinical infections in the majority of cases. Thus, symptomatic anaplasmosis appears to be a rare disease in Scandinavia. This may account for our inability to detect A. phagocytophilum DNA in the serum samples derived from the Anaplasma-reactive anonymous patient samples, even when using two different PCRs targeting different A. phagocytophilum genes. However, we cannot exclude that our use of serum or plasma may have given a poorer DNA yield compared to if we had used buffy coat or whole blood in view of the intracellular nature of A. phagocytophilum, which resides within granulocytes.
It is possible that the Anaplasma seroreactivity we have detected among neoehrlichiosis patients reflects previous exposure to A. phagocytophilum. We have no evidence to suggest that the neoehrlichiosis patients were doubly infected with A. phagocytophilum and Ca. N. mikurensis since all patients were negative for A. phagocytophilum by PCR and confirmatory sequencing of the Ca. N. mikurensis PCR amplicons was in no case ambiguous.
The third possible explanation for why up to every fifth of the neoehrlichiosis patients presented with Anaplasma antibodies is that these antibodies were in fact directed against Ca. N. mikurensis and cross-reactive with A. phagocytophilum antigens. One indication that this might be the case is the semblance of an antibody response among the few neoehrlichiosis patients from whom it was possible to obtain repeated blood samples in the present study. Two published studies have also implied that neoehrlichiosis patients may respond with Anaplasma-reactive antibodies, indicative of cross-reactivity [2, 6]. However, the issue of cross-reactivity will only be addressable once Ca. N. mikurensis antigens are available, which will require its cultivation.
Irrespective of the underlying mechanisms behind the A. phagocytophilum seroreactivity demonstrated by some neoehrlichiosis patients, the main significance of this finding is that a certain degree of vigilance is warranted: patients believed to have anaplasmosis may in fact have neoehrlichiosis. Moreover, patients queried for A. phagocytophilum antibodies that turn out to be seronegative may have neoehrlichiosis. Two of the neoehrlichiosis patients described in this study were discovered among patient samples submitted for A. phagocytophilum serology thanks to relevant clinical data, both of whom were seronegative for Anaplasma. A correct diagnosis is of utmost importance since these two infectious diseases differ with regard to one vital aspect: neoehrlichiosis patients have a substantial risk of contracting vascular events such as deep vein thrombosis, arterial aneurysms or transitory ischemic attacks, which are not recognized to be part of an infectious process [5]. If neoehrlichiosis patients with vascular complications are correctly diagnosed and adequately treated with antibiotics, they do not incur new vascular events [5].
To conclude, patients with fever of uncertain origin or with suspected anaplasmosis may in fact have neoehrlichiosis. Misdiagnosed or undiagnosed cases of neoehrlichiosis may be identified either among Anaplasma seropositive patients or among patient samples queried for Anaplasma antibodies that are negative by A. phagocytophilum IFA but have typical risk factors for severe neoehrlichiosis. We recommend that such patients be assayed for the presence of Ca. N. mikurensis DNA by PCR performed on EDTA blood or plasma to determine if they have contracted neoehrlichiosis.
References
Wenneras C (2015) Infections with the tick-borne bacterium Candidatus Neoehrlichia mikurensis. Clin Microbiol Infect 21(7):621–630
Fehr J, Bloemberg G, Ritter C, Hombach M, Lüscher T, Weber R, Keller P (2010) Septicemia caused by tick-borne bacterial pathogen Candidatus Neoehrlichia mikurensis. Emerg Infect Dis 16(7):1127–1129
Welinder-Olsson C, Kjellin E, Vaht K, Jacobsson S, Wenneras C (2010) First case of human “Candidatus Neoehrlichia mikurensis” infection in a febrile patient with chronic lymphocytic leukemia. J Clin Microbiol 48(5):1956–1959
von Loewenich F, Geissdörfer W, Disqué C, Matten J, Schett G, Sakka S, Bogdan C (2010) Detection of “Candidatus Neoehrlichia mikurensis” in two patients with severe febrile illnesses: evidence for a European sequence variant. J Clin Microbiol 48(7):2630–2635
Grankvist A, Andersson PO, Mattsson M, Sender M, Vaht K, Hoper L, Sakiniene E, Trysberg E, Stenson M, Fehr J, Pekova S, Bogdan C, Bloemberg G, Wenneras C (2014) Infections with the tick-borne bacterium “Candidatus Neoehrlichia mikurensis” mimic noninfectious conditions in patients with B cell malignancies or autoimmune diseases. Clin Infect Dis 58(12):1716–1722
Grankvist A, Sandelin LL, Andersson J, Fryland L, Wilhelmsson P, Lindgren PE, Forsberg P, Wenneras C (2015) Infections with Candidatus Neoehrlichia mikurensis and cytokine responses in 2 persons bitten by ticks, Sweden. Emerg Infect Dis 21(8):1462–1465
Li H, Jiang J, Liu W, Zheng Y, Huo Q, Tang K, Zuo S, Liu K, Jiang B, Yang H, Cao W (2012) Human infection with Candidatus Neoehrlichia mikurensis, China. Emerg Infect Dis 18(10):1636–1639
Quarsten H, Grankvist A, Hoyvoll L, Myre IB, Skarpaas T, Kjelland V, Wenneras C, Noraas S (2017) Candidatus Neoehrlichia mikurensis and Borrelia burgdorferi sensu lato detected in the blood of Norwegian patients with erythema migrans. Ticks Tick Borne Dis 8(5):715–720
Welc-Faleciak R, Sinski E, Kowalec M, Zajkowska J, Pancewicz SA (2014) Asymptomatic “Candidatus Neoehrlichia mikurensis” infections in immunocompetent humans. J Clin Microbiol 52(8):3072–3074
Grankvist A, Moore ER, Svensson Stadler L, Pekova S, Bogdan C, Geissdorfer W, Grip-Linden J, Brandstrom K, Marsal J, Andreasson K, Lewerin C, Welinder-Olsson C, Wenneras C (2015) Multilocus sequence analysis of clinical “Candidatus Neoehrlichia mikurensis” strains from Europe. J Clin Microbiol 53(10):3126–3132
Dadgar A, Grankvist A, Wernbro L, Wennerås C (2017) Oklar feber hos patient med MS och rituximab-behandling var neoehrlichios—ny fästingburen infektion som är svår att diagnosticera. Läkartidningen 114:1–4
Frivik JO, Noraas S, Grankvist A, Wenneras C, Quarsten H (2017) A man in his sixties from Southern Norway with intermittent fever. Tidsskr Nor Laegeforen 137(23–24)
Courtney JW, Kostelnik LM, Zeidner NS, Massung RF (2004) Multiplex real-time PCR for detection of Anaplasma phagocytophilum and Borrelia burgdorferi. J Clin Microbiol 42(7):3164–3168
Haschke-Becher E, Bernauer R, Walleczek AM, Apfalter P, Afazel-Saeedi S, Kraus J, Ladurner G, Strasser P (2010) First detection of the Anaplasma phagocytophilum groEL-A genotype in man. J Inf Secur 60(4):300–305
Bakken JS, Krueth J, Tilden RL, Dumler JS, Kristiansen BE (1996) Serological evidence of human granulocytic ehrlichiosis in Norway. Eur J Clin Microbiol Infect Dis 15(10):829–832
Skarphedinsson S, Sogaard P, Pedersen C (2001) Seroprevalence of human granulocytic ehrlichiosis in high-risk groups in Denmark. Scand J Infect Dis 33(3):206–210
Hjetland R, Henningsson AJ, Vainio K, Dudman SG, Grude N, Ulvestad E (2015) Seroprevalence of antibodies to tick-borne encephalitis virus and Anaplasma phagocytophilum in healthy adults from western Norway. Infect Dis (Lond) 47(1):52–56
Dumler JS, Dotevall L, Gustafson R, Granstrom M (1997) A population-based seroepidemiologic study of human granulocytic ehrlichiosis and Lyme borreliosis on the west coast of Sweden. J Infect Dis 175(3):720–722
Henningsson AJ, Wilhelmsson P, Gyllemark P, Kozak M, Matussek A, Nyman D, Ekerfelt C, Lindgren PE, Forsberg P (2015) Low risk of seroconversion or clinical disease in humans after a bite by an Anaplasma phagocytophilum-infected tick. Ticks Tick Borne Dis 6(6):787–792
Bjoersdorff A, Berglund J, Kristiansen BE, Soderstrom C, Eliasson I (1999) Varying clinical picture and course of human granulocytic ehrlichiosis. Twelve Scandinavian cases of the new tick-borne zoonosis are presented. Läkartidningen 96(39):4200–4204
Bjoersdorff A, Wittesjo B, Berglun J, Massung RF, Eliasson I (2002) Human granulocytic ehrlichiosis as a common cause of tick-associated fever in Southeast Sweden: report from a prospective clinical study. Scand J Infect Dis 34(3):187–191
Blanco JR, Oteo JA (2002) Human granulocytic ehrlichiosis in Europe. Clin Microbiol Infect 8(12):763–772
Acknowledgments
Charlotte Sværke-Jørgensen, Head of the Serology Laboratory at Statens Serum Institut, Denmark, is thanked for provision of the relevant serum samples. Anneli Bjoersdorff, AniCura, Sweden, is recognized for provision of positive control samples containing A. phagocytophilum DNA.
Funding
The project was supported by EU Interreg ScandTick Innovation, Västra Götaland Regional Research and Development Fund (94510), ALF Research Fund (71580), and by the Cancer and Allergy Foundation (16-113).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the local Ethical Review Boards of Göteborg and Uppsala, Sweden.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the regional research committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Wass, L., Grankvist, A., Mattsson, M. et al. Serological reactivity to Anaplasma phagocytophilum in neoehrlichiosis patients. Eur J Clin Microbiol Infect Dis 37, 1673–1678 (2018). https://doi.org/10.1007/s10096-018-3298-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3298-3