Abstract
Catheter-related bloodstream infections (CRBSI) are major complications for patients with life-threatening conditions requiring chronic vascular catheterization. The wide range of etiologic microbes and the ongoing development of resistance to antimicrobials with specific mechanisms of action make this an appropriate target for applying a nonspecific antimicrobial therapeutic. Taurolidine hydrolyzes into two antimicrobial moieties, formaldehyde and methylene glycol, which react with microbial surfaces. Neutrolin® (taurolidine, heparin, calcium citrate) was recently introduced in Germany as an antimicrobial catheter lock solution. This postmarketing experience collected data on 201 patients at 20 centers from January 2014 through September 2016. Likely CRBSI was observed in 13 episodes in 47,118 days (0.2759 per 1000 days [0.1468, 0.4718]). Thrombosed catheter was observed in seven catheters in 47,118 days (0.1486 per 1000 days [0.0595, 0.3061]). No adverse drug reactions that led to the discontinuation of Neutrolin® use were reported. Two patients experienced occasional transient dysgeusia. Neutrolin®, when used in conjunction with guideline-based catheter care, showed reduction in the rate of both CRBSI and catheter thrombosis relative to recent historical controls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
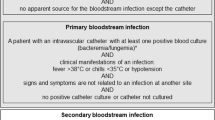
Catheter-related bloodstream infections (CRBSI) and thrombosis are the major complications in hemodialysis patients [1]. Microbes known to cause CRBSI include Gram-positive and Gram-negative bacteria, and yeasts [2]. CRBSI are associated with substantial morbidity, mortality, and excess healthcare costs. Patients who receive dialysis through the catheter are 2–3 times more likely to be hospitalized for infection and to die of septic complications than dialysis patients with grafts or fistula [1, 3]. Guideline-based care has had a dramatic impact where implemented. CRBSI rate reduction to 0.5 infections per 1000 patient days was reported in a compliant hemodialysis unit in 2017 [4]. Neutrolin® (CorMedix, Berkeley Heights, NJ, USA) contains taurolidine as its active antimicrobial, which has demonstrated efficacy in children and adults [5, 6]. Taurolidine is a nonspecific antimicrobial with a broad spectrum of activity [7], and no microbial resistance has been observed [8]. Neutrolin® was recently introduced in Germany as an antimicrobial catheter lock solution. Postmarketing experience is important in assessing the CRBSI rate impact of Neutrolin® when used in routine practice.
Methods
A surveillance program monitoring Neutrolin® use in hemodialysis patients receiving dialysis through tunneled central venous catheters was undertaken at 20 dialysis centers in Germany from January 2014 to September 2016. Hemodialysis patients with new tunneled central venous catheters who had not been hospitalized within the previous 6 months due to CRBSI or catheter thrombosis were selected. Patients received Neutrolin® 2–3 times per week and were followed until either the catheter failed due to clotting or CRBSI, or it is removed due to fistula maturation. Data describing dialysis sessions, likely CRBSI, and catheter thrombi were collected. Investigators reported adverse drug reactions according to postmarketing standards. A total of 201 patients were exposed to more than or equal to one dose of Neutrolin® and they had 15,706 dialysis sessions. Catheter days were estimated by multiplying dialysis sessions by 3. 95% confidence intervals (CIs) of infection rate and thrombosis rate were calculated using Byar’s approximation and the Poisson method, and verified using open source software (http://www.openepi.com).
Results
The results are displayed in Table 1.
Adverse drug reactions
No adverse drug reactions leading to the discontinuation of Neutrolin® use were reported. Two patients experienced occasional transient dysgeusia.
Discussion
This paper describes the postmarketing experience with Neutrolin® in dialysis units in Germany after the publication of new guidelines [9, 10] to prevent infection. Though this was an open-label experience, there are two relevant historical controls whose data are displayed in Table 1; Napalkov et al. [1], where the data were collected prior to the institution of these guidelines, and Youssouf et al. [4], where the data were collected afterwards. Comparison of the two historical controls shows a dramatic improvement in infection rates prior to this Neutrolin® experience. The Youssouf et al. [4] experience describes a focused implementation of guidelines with resultant improvement in infection rates. In order to obtain a perspective on whether the low rates observed with Neutrolin® are due to chance alone, 95% CIs were calculated. As can be seen in Table 1, the upper bound of the 95% CI is less than the mean result from Youssouf et al. [4]. Though this cannot be interpreted as a statistically significant difference from historical controls, it is interesting reinforcement of the observed trend. Currently, there is a large, double-blind, randomized, active control study comparing Neutrolin® to heparin in the United States that is statistically powered to deliver definitive results (LOCK-IT-100; see Clinicaltrials.gov). In conclusion, Neutrolin®, when used in conjunction with guideline-based catheter care, can reduce the rate of both CRBSI and catheter thrombosis relative to recent historical controls.
References
Napalkov P, Felici DM, Chu LK, Jacobs JR, Begelman SM (2013) Incidence of catheter-related complications in patients with central venous or hemodialysis catheters: a health care claims database analysis. BMC Cardiovasc Disord 13:86. https://doi.org/10.1186/1471-2261-13-86
Gahlot R, Nigam C, Kumar V, Yadav G, Anupurba S (2014) Catheter-related bloodstream infections. Int J Crit Illn Inj Sci 4(2):162–167
Katneni R, Hedayati SS (2007) Central venous catheter-related bacteremia in chronic hemodialysis patients: epidemiology and evidence-based management. Nat Clin Pract Nephrol 3(5):256–266
Youssouf S, Nache A, Wijesekara C, Middleton RJ, Lewis D, Shurrab AE, O’Riordan E, Lappin LP, O’Donoghue D, Kalra PA, Hegarty J (2017) Effect of a quality improvement program to improve guideline adherence and attainment of clinical standards in dialysis care: report of outcomes in year 1. Nephron 136(2):75–84
Dümichen MJ, Seeger K, Lode HN, Kühl JS, Ebell W, Degenhardt P, Singer M, Geffers C, Querfeld U (2012) Randomized controlled trial of taurolidine citrate versus heparin as catheter lock solution in paediatric patients with haematological malignancies. J Hosp Infect 80(4):304–309
Olthof ED, Versleijen MW, Huisman-de Waal G, Feuth T, Kievit W, Wanten GJ (2014) Taurolidine lock is superior to heparin lock in the prevention of catheter related bloodstream infections and occlusions. PLoS One 9(11):e111216
Shah CB, Mittelman MW, Costerton JW, Parenteau S, Pelak M, Arsenault R, Mermel LA (2002) Antimicrobial activity of a novel catheter lock solution. Antimicrob Agents Chemother 46(6):1674–1679
Liu Y, Zhang AQ, Cao L, Xia HT, Ma JJ (2013) Taurolidine lock solutions for the prevention of catheter-related bloodstream infections: a systematic review and meta-analysis of randomized controlled trials. PLoS One 8(11):e79417
Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O’Grady NP, Raad II, Rijnders BJA, Sherertz RJ, Warren DK (2009) Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis 49(1):1–45
Vanholder R, Canaud B, Fluck R, Jadoul M, Labriola L, Marti-Monros A, Tordoir J, Van Biesen W (2010) Diagnosis, prevention and treatment of haemodialysis catheter-related bloodstream infections (CRBSI): a position statement of European Renal Best Practice (ERBP). NDT Plus 3(3):234–246
Acknowledgements
The authors and CorMedix, Inc. and CorMedix Europe GmbH wish to gratefully acknowledge the contributions of the following investigators at the dialysis units: Dr. Iwig at Meiningen, Dr. Scholl at Mühlhausen/Bad Langensalza, Dr. Knittel at Witten, Dr. Rahman at Magdeburg, Dr. Fierlbeck at Dillenburg, Dr. Rettig at Quedlinburg, Dr. Menzer at Homburg, Dr. Tröster at Westerstede, Dr. Sina Küllmer at DZ Kirchhain, Dr. Kuehn at Tangermünde/Genthin, Dr. Krebs at Menden, Dr. Winkelmann at Ilfeld/Sondershausen, Dr. M. Peuters at Leverkusen, Dr. Schlee at Weissenfels, Dr. Busch at Lünen, Dr. Müller at Erftstadt, Dr. Anger at Arnstadt, Dr. Bunia at Iserlohn, and Drs D. Kaapke and Bachmann at Arnsberg.
The authors and CorMedix also wish to gratefully acknowledge the assistance of Frau Ute Petrak of CorMedix Europe GmbH, who ensured that documentation and approvals were maintained.
Funding
This work was funded by CorMedix, Inc., Bedminster, NJ, USA.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics
Neutrolin® was used consistent with its marketing authorization in the EU. Accordingly, as specified in German Medical Device Law (§ 23b MPG), if a CE-marked medical device is used in a clinical trial within its intended purpose, the respective study is not subject to ethics approval.
Informed consent
Patient consent was not required, because individually identified data were anonymized and aggregated by the reporting physicians, consistent with EU data protection law (Directive 95/46/EC).
Potential conflict of interest
BER and BP are members of CorMedix, Inc.’s Scientific Advisory Board.
CW is a Data Safety Monitoring Board Member for CorMedix, Inc.
AS was an employee of CorMedix, Inc.
AEP is an employees of CorMedix, Inc.
DS is an employee of CorMedix Europe GmbH.
MC has no conflict of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Reidenberg, B.E., Wanner, C., Polsky, B. et al. Postmarketing experience with Neutrolin® (taurolidine, heparin, calcium citrate) catheter lock solution in hemodialysis patients. Eur J Clin Microbiol Infect Dis 37, 661–663 (2018). https://doi.org/10.1007/s10096-017-3157-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-017-3157-7