Abstract
Recurrent human cytomegalovirus (HCMV) infection during pregnancy could lead to congenital HCMV infection and permanent sequelae. However, knowledge regarding the risk factors associated with recurrent HCMV infection is limited. In the present study, 1,659 paired serum samples from the natural population were collected in Guangxi Province, China, from 2003 to 2004 with a 1-year interval. The serum anti-pp150 titre was quantitatively determined using a homemade recombinant pp150-based ELISA, and the IgG titre that increased at least 4-fold was defined as a recurrent infection. The HCMV seroprevalence was above 98.6% (1,636/1,659) in Guangxi in 2003, and the infection rate during the 1-year follow-up was approximately 10% (171/1,659). The seronegative population has the highest infection risk, while the risk of recurrent infection in the seropositive population was negatively correlated with the baseline anti-pp150 titre. With a cutoff of 1:80 (the baseline anti-pp150 IgG titre), the sensitivity and specificity were 73.1% (125/171) and 85.7% (1,275/1,488) respectively, and the relative risk of infection in the high-risk group compared to the low-risk group was 10.6 (95% CI: 7.7–14.6). In conclusion, the baseline anti-pp150 IgG was negatively correlated with the risk of HCMV infection and could be an excellent predictor of HCMV infection in HCMV seropositive populations.
Similar content being viewed by others
Introduction
The majority of the hazards associated with human cytomegalovirus (HCMV) infection come from congenital infections [1]. For a long time, it was believed that there would be no serious outcomes of congenitally infected children born to mothers with preexisting antibodies [2]. However, emerging studies demonstrated that the risk for symptomatic infection at birth and the sequelae in children born to mothers who are seropositive may be similar to that in infants born to mothers experiencing a primary infection [3–6]. These studies underscored the importance of recurrent HCMV infection in seropositive populations; however, knowledge regarding risk factors associated with recurrent HCMV infection remains scarce.
In previous studies, antibodies specific to gB (strain specific) of different HCMV strains were used for the detection of HCMV reinfection during pregnancy [7, 8]. However, acquisition of antibodies against the gB protein of new HCMV strains would only reflect the reinfection of a specific HCMV strain and not the reactivation of latent infection. In these studies, we also noted that serum anti-HCMV IgG and anti-gB IgG levels were lower in mothers whose infants had congenital HCMV infection than those without infected infants [8]. Thus, we speculated that the baseline antibody titre may be correlated with the risk of recurrent infection.
Different from the neutralizing antigen gB, the tegument protein pp150 was conserved among different HCMV strains, and it was the most immunogenic protein [9]. In the present study, a population from a high HCMV endemic area was serologically followed, and the serum samples were examined with a recombinant pp150 based HCMV IgG ELISA developed in our previous study [10]. The results demonstrated that the baseline anti-HCMV pp150 titre was negatively correlated with the risk of HCMV infection and an excellent indicator for the prediction of recurrent HCMV infection episodes.
Materials and methods
Serum samples
An initial follow-up seroepidemiological study of hepatitis E virus infection was conducted in 2003 and 2004 among eight rural communities in Guangxi Province, China [11]. Serum samples were taken in 2003 from 7,284 participants. A second sample was taken 12 months later from a subpopulation of 3,431 of these individuals. After the initial study, the residual serum samples were sealed and kept at −20 °C. Among them, 1,659 pairs of well-stored serum samples were collected from five communities, including Binyang (BY), Guilin (GL), Lingshan (LS), Tiandeng (TD) and Xing’an (XA), and were used for this study. The characteristics of the participant population are summarized in Table 1. Additional ethical approval for the study was obtained from the Institutional Review Board of School of Public Health, Xiamen University.
Serological measurements
IgG detection
The anti-pp150 IgG was detected using a home-made indirect enzyme-linked immunosorbant assay (ELISA), as previously described [10]. The cutoff value was calculated as 0.15 + mean OD value of the negative control, and an OD value above the cutoff indicated a positive result. For positive samples, the serum was two-fold serially diluted from 1:10 and then retested. The reciprocal of the highest dilution of the serum higher than or equal to the cutoff was defined as the titre of the serum. The anti-pp150 antibody titre of the negative serum samples was defined as 1:5.
IgM detection
The anti-HCMV IgM was detected using a commercially available ELISA kit, ETI-CYTOK-M reverse PLUS (DiaSorin, Saluggia, Italy), and based on an antibody capture technique according to the user’s manual. Briefly, the microplates were coated with human IgM-specific IgG antibody, and the presence of specific IgM was detected by HRP-conjugated monoclonal anti-CMV IgG, which can bind to the solid-phase HCMV antigen. The optical density (OD) was read at a wavelength of 450 nm with a reference filter of 630 nm. The results are calculated as index values using two replicates of the cut-off control, and samples with index values above 1.1 indicated a positive result.
Microneutralization assay
The neutralizing activity of the serum samples were detected by a microneutralization assay based on an ELISPOT technique previously described [12]. Different from the previously described method, ARPE cells were used for the HCMV neutralization assay, and the serum samples were serially two-fold diluted from 1:20 and mixed with HCMV AD169. The expression of HCMV IE1 protein was immunostained by mouse monoclonal antibody L14 (ATCC, Manassas, VA, USA) and detected with Vectastain® ABC kits (Vector Labs, Burlingame, CA, USA) according to the manufacturer’s protocol for better sensitivity.
The neutralization curves were then automatically plotted by 4-PL curve fitting using GraphPad Prism® V5.00 (GraphPad Software, Inc., La Jolla, CA, USA), and the reciprocal of the serum dilution with 50% neutralization was determined to be the NT50 titre of each serum sample.
Definition of HCMV infection episodes
A primary HCMV infection episode is defined as that the IgG antibody titer conversed from negative to at least 1:20 in seronegative participants. A recurrent HCMV infection episode is defined as that the IgG antibody titre increased at least 4-fold in seropositive participants [13].
Statistical methods
Statistical analyses were performed using SPSS 18.0 (SPSS Inc, Chicago, IL, USA). Pearson chi-square analysis was used to determine the differences in IgG seroprevalence, IgM seroprevalence and recurrent HCMV infection based on gender, age, and community. Mann–Whitney analysis was used to compare the anti-HCMV IgG titre in different groups. MedCalc Statistical Software version 16.2.1 (MedCalc Software bvba, Ostend, Belgium; https://www.medcalc.org; 2016) was used to plot the receiver operating characteristic curve (ROC) to calculate the area under the curve (AUC) and to determine the cutoff value of the baseline anti-pp150 titre to distinguish participants with or without HCMV infection. The Youden index was defined as sensitivity + specificity − 1.
Results
HCMV serological profiles at baseline
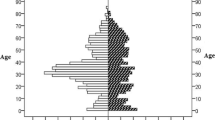
The median age of the participants was 38 years old (range: 0.5–87 years), and the male to female ratio was 0.85 (762/897). All participants were tested for HCMV IgG and IgM. The baseline seroprevalence of anti-HCMV IgG and IgM of the population in 2003 are 98.6% (95% CI, 97.9–99.1) and 2.1% (95% CI 1.5–2.9) respectively (Table 1). There was no significant difference in seroprevalence based on age, gender, or community. The geometric mean of the titre (GMT) of anti-HCMV IgG was 285.0 (95% CI, 269.2–301.9) (Table 1), and the distribution of anti-HCMV IgG titres is plotted in Fig. 1. Approximately 65% of the participants had anti-HCMV IgG titres between 1:160 and 1:640.
Changes in anti-HCMV IgG titres during follow-up
The second serum samples were collected 12 months later and tested for antibodies against HCMV. The anti-HCMV IgG level of the whole population remained stable (Table 2). However, changes in the mean antibody levels are negatively related to the baseline titre (p < 0.0001). As the baseline antibody titre increased, the faster the antibody titres dropped. In subgroups with baseline antibody titres of no more than 1:80, the mean titre increased significantly (Table 2).
The 100 pairs of serum samples with different IgG titre changing ratios were selected for testing the relation of the IgG titre changing ratio with the neutralizing antibody titre changing ratio (Supplementary Figure 2). The results showed that the changing ratio of IgG titres is strongly correlated with that of the neutralizing antibody titres (R 2 = 0.69). In addition, the antibody specific for other HCMV antigens was also elevated in the group of participants with above 4-fold elevation in anti-pp150 IgG titre during follow-up (Supplementary Table 1). These results indicated that the anti-pp150 IgG titre was closely associated with HCMV infection episodes.
Correlation between baseline IgG antibody titre and HCMV infection episodes
Of the 1,659 participants, 171 (10.3%, 95% CI 8.8–11.9) encountered HCMV infection episodes, as indicated by seroconversion or with an increase greater than 4-fold in anti-HCMV IgG titres. Among them, 19 infection episodes occurred in 23 seronegative participants (82.6%, 95% CI 55.5%–95.3%) (primary infection), and 152 occurred in 1,636 seropositive participants (9.3%, 95% CI 7.9%–10.9%) (recurrent infection). The baseline anti-pp150 IgG titre of the infection episodes was significantly lower than that of the participants without HCMV infection (Supplementary Figure 1), and the infection risk is negatively related to the baseline antibody titre (p < 0.0001) (Table 2 and Supplementary Figure 3). Participants with antibody titres no less than 1:2,560 had the lowest infection risk (i.e., an infection risk of zero), and seronegative participants had the highest infection risk, 82.6%. However, neither the IgM status in 2003/2004 nor the changing of anti-HCMV IgM status was correlated with the HCMV episodes during follow-up (Supplementary Table 3).
Performance of the baseline IgG titre in predicting HCMV infections
The baseline anti-pp150 IgG titre was negatively correlated with risk of HCMV infection, and it was an excellent predictor of HCMV infection, as indicated by an AUC of 0.881 obtained from the ROC analysis (95% CI: 0.864-0.896) (Fig. 2 and Table 3). The suggested optimal cutoff value of IgG titre by ROC is 1:80 for the entire population, with a Youden index of 0.59, and the sensitivity and specificity were 73.1% (95% CI: 65.8%–79.6%) and 85.7% (95% CI: 83.8%–87.4%), respectively. According to the cutoff, the number of individuals with a higher risk (baseline anti-pp150 IgG titre ≤1:80) was 338 (20.4%), and the number of individuals with a lower risk (baseline anti-pp150 IgG titre >1:80) was 1321 (79.6%) (Table 3). Among the high-risk group, 125 participants were infected by HCMV (36.9%), which is significantly higher than that of the low-risk group (3.5%, 46/1,321) (relative risk = 10.6, 95% CI: 7.7-–4.6) (Table 3).
The ROC analysis was also conducted for child-bearing female participants (aged from 15 to 49), and similar results have been observed (Fig. 2 and Table 3). When the cutoff was set as 1:160, the optimal cutoff suggested by ROC analysis, the sensitivity and specificity among child-bearing female participants was 93.6% (95% CI: 82.5%–98.7%) and 72.6% (95% CI 68.5%–76.4%), respectively (Table 3). The relative risk in the high-risk group compared to the low-risk group was 29.7 (95% CI: 9.4–94.5) (Table 3).
Discussion
In pregnant women, both primary and recurrent HCMV infection can lead to congenital HCMV infection with similar clinical hazards. In high prevalence areas, such as China, the seroprevalence of HCMV could reach 90% or more, and the majority of congenitally infected children were born to seropositive pregnant mothers harbouring recurrent infection [2]. For decreasing congenital HCMV-related morbidity and mortality, it was valuable to find a way to identify child-bearing females with a high risk of recurrent HCMV infection.
HCMV vaccines have been developed for decreasing HCMV-related diseases and proved to be effective in the HCMV seronegative population [14]. Identification of a high-risk recurrent HCMV infection population may help promote the study of the effectiveness of existing HCMV vaccines and development of new HCMV vaccines to prevent recurrent HCMV infection or congenital infection. In the seropositive population, when a pregnant woman was identified with a high risk of HCMV infection, intervention with hyperimmune globulin during pregnancy could help decrease the risk of congenital HCMV infection in the infant [15]. In addition, in countries where congenital HCMV infection screening is not performed for all infants, once the mother was identified with a high risk of HCMV infection during pregnancy, congenital HCMV screening of the infants should be conducted after birth. Intervention could be started once the infant is identified as congenitally infected to decrease the consequences of congenital HCMV infection [15, 16].
The seroprevalence of HCMV was extremely high in Guangxi (98.6%), and most individuals in this region have been infected with HCMV at an early age, as the seroprevalence in the group that was 0–14 years old was already 97.5% (Table 1). The seroprevalence observed in this study was consistent with previous studies in other areas of China [17, 18]. As indicated by an increase greater than 4-fold and by seroconversion in anti-pp150 IgG, the HCMV infection rate was approximately 10% among the participants (9% for seropositive participants). Such characteristics made this an excellent population for the study of recurrent HCMV infection, and we found that the baseline serum anti-pp150 IgG titre was negatively correlated with the risk of HCMV infection. The highest HCMV infection rate was observed in the seronegative participants. In the seropositive population, the lower the baseline of the anti-pp150 level, the higher the risk of infection (Table 2 and Supplementary Figure 3). In addition, the ROC analysis results indicated that the conclusion (the baseline antibody titre could be an excellent indicator of HCMV infection) was also applicable in the child-bearing female population (Table 3 and Fig. 2).
Although we found that the baseline anti-pp150 IgG level can be used to predict the risk of recurrent HCMV infection in this study, many more studies must be conducted before this finding becomes more clinically significant. Most importantly, the correlation between baseline antibody level at an early stage of pregnancy and HCMV infection in mothers with congenitally infected infants must be investigated. In addition, a standard curve using international standards should be included to make the results from different laboratories comparable.
References
Grosse SD, Ross DS, Dollard SC (2008) Congenital cytomegalovirus (CMV) infection as a cause of permanent bilateral hearing loss: A quantitative assessment. J Clin Virol 41(2):57–62
Manicklal S, Emery VC, Lazzarotto T, Boppana SB, Gupta RK (2013) The “silent” global burden of congenital cytomegalovirus. Clin Microbiol Rev 26(1):86–102
Yamamoto AY, Mussi-Pinhata MM, Isaac MD, Amaral FR, Carvalheiro CG, Aragon DC, Manfredi AKD, Boppana SB, Britt WJ (2011) Congenital cytomegalovirus infection as a cause of sensorineural hearing loss in a highly immune population. Pediatr Infect Dis J 30(12):1043–1046
Boppana SB, Fowler KB, Britt WJ, Stagno S, Pass RF (1999) Symptomatic congenital cytomegalovirus infection in infants born to mothers with preexisting immunity to cytomegalovirus. Pediatrics 104(1 Pt 1):55–60
Ross SA, Fowler KB, Ashrith G, Stagno S, Britt WJ, Pass RF, Boppana SB (2006) Hearing loss in children with congenital cytomegalovirus infection born to mothers with preexisting immunity. J Pediatr 148(3):332–336
Zalel Y, Gilboa Y, Berkenshtat M, Yoeli R, Auslander R, Achiron R, Goldberg Y (2008) Secondary cytomegalovirus infection can cause severe fetal sequelae despite maternal preconceptional immunity. Ultrasound Obstet Gynecol 31(4):417–420
Yamamoto AY, Mussi-Pinhata MM, Boppana SB, Novak Z, Wagatsuma VM, Oliveira PD, Duarte G, Britt WJ (2010) Human cytomegalovirus reinfection is associated with intrauterine transmission in a highly cytomegalovirus-immune maternal population. Am J Obstet Gynecol 202(3):297.e1–297.e8
Boppana SB, Rivera LB, Fowler KB, Mach M, Britt WJ (2001) Intrauterine transmission of cytomegalovirus to infants of women with preconceptional immunity. NEngl J Med 344(18):1366–1371
Greijer AE, van de Crommert JM, Stevens SJ, Middeldorp JM (1999) Molecular fine-specificity analysis of antibody responses to human cytomegalovirus and design of novel synthetic-peptide-based serodiagnostic assays. J Clin Microbiol 37(1):179–188
Xi Huang JL, Shengxiang G, Tingdong L, Tongming F, Jun Z (2017) Establishment and validation of an enzyme-linked immunosorbent assay for IgG antibody against cytomegalovirus based on pp 150 antigen. J Virol Methods 240(C):21–25
Li RC, Ge SX, Li YP, Zheng YJ, Nong Y, Guo QS, Zhang J, Ng MH, Xia NS (2006) Seroprevalence of hepatitis E virus infection, rural southern People’s Republic of China. Emerg Infect Dis 12(11):1682–1688
Li T, Lin H, Yu L, Xue M, Ge S, Zhao Q, Zhang J, Xia N (2014) Development of an enzyme-linked immunospot assay for determination of rotavirus infectivity. J Virol Methods 209:7–14
Gouma S, Schurink-Van’t Klooster TM, de Melker HE, Kerkhof J, Smits GP, Hahne SJ, van Els CA, Boland GJ, Vossen AC, Goswami PR, Koopmans MP, van Binnendijk RS (2014) Mumps serum antibody levels before and after an outbreak to assess infection and immunity in vaccinated students. Open forum Infect Dis 1(3):ofu101
Griffiths P, Baraniak I, Reeves M (2015) The pathogenesis of human cytomegalovirus. J Pathol 235(2):288–297
Nigro G, Adler SP, La Torre R, Best AM, Congenital Cytomegalovirus Collaborating Group (2005) Passive immunization during pregnancy for congenital cytomegalovirus infection. N Engl J Med 353(13):1350–1362
Yinon Y, Farine D, Yudin MH (2010) Screening, diagnosis, and management of cytomegalovirus infection in pregnancy. Obstet Gynecol Surv 65(11):736–743
Zhao P, Ma D, Xue F, Ji C, Wang S, Zhang X, Zhou Y, Yu X (2009) Seroprevalence and risk factors of human cytomegalovirus infection in the eastern Chinese population. Arch Virol 154(4):561–564
Zhang Q, Gao Y, Peng Y, Fu M, Liu YQ, Zhou QJ, Yu J, Zheng XQ (2014) Epidemiological survey of human cytomegalovirus antibody levels in children from Southeastern China. Virol J 11:123
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding information
This study was supported by the National Natural Science Foundation of China (81472015) and (31670927).
Conflicts of interest
The authors declare that they have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 297 kb)
Rights and permissions
About this article
Cite this article
Li, Td., Li, Jj., Huang, X. et al. Baseline antibody level may help predict the risk of active human cytomegalovirus infection in a HCMV seropositive population. Eur J Clin Microbiol Infect Dis 36, 863–868 (2017). https://doi.org/10.1007/s10096-016-2873-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-016-2873-8