Abstract
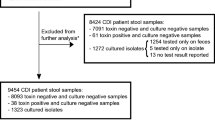
Clostridium difficile, methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (VRE) are worldwide prevalent healthcare-associated pathogens. We have evaluated three Qiagen artus QS-RGQ assays for the detection of these pathogens. We examined 200 stool samples previously tested for C. difficile infection (CDI), 94 rectal swabs previously screened for VRE and 200 MRSA screening nasal swabs. With the routine diagnostic laboratory results being adopted as the gold standard, the sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of the artus C. difficile assay were 100%, for the artus VanR QS-RGQ assay, 95, 68, 44 and 98%, and for the artus MRSA/SA assay, 80, 94, 93 and 83%, respectively. The artus VanR assay detected the vanA and/or vanB genes in 32% of culture-negative VRE screens; in 71% of these cases, only vanB was detected. An over-estimation of the rate of faecal VRE colonisation could be due to a patient population with high rates of faecal carriage of non-enterococcal species carrying vanB. Based on our findings, we conclude that all three artus QS-RGQ assays could be a useful addition to a diagnostic laboratory, and that the optimal choice of assay should be determined according to user needs.
Similar content being viewed by others
References
Kara A, Devrim İ, Bayram N, Katipoğlu N, Kıran E, Oruç Y, Demiray N, Apa H, Gülfidan G (2015) Risk of vancomycin-resistant enterococci bloodstream infection among patients colonized with vancomycin-resistant enterococci. Braz J Infect Dis 19:58–61
Khanna S, Pardi DS (2010) The growing incidence and severity of Clostridium difficile infection in inpatient and outpatient settings. Expert Rev Gastroenterol Hepatol 4:409–416
Köck R, Becker K, Cookson B, van Gemert-Pijnen JE, Harbarth S, Kluytmans J, Mielke M, Peters G, Skov RL, Struelens MJ, Tacconelli E, Navarro Torné A, Witte W, Friedrich AW (2010) Methicillin-resistant Staphylococcus aureus (MRSA): burden of disease and control challenges in Europe. Euro Surveill 15:19688
World Health Organization (WHO) (2011) Report on the burden of endemic health care-associated infection worldwide. A systematic review of the literature. Available online at: http://www.who.int/en/. Accessed 11 April 2016
Walters PR, Zuckerbraun BS (2014) Clostridium difficile infection: clinical challenges and management strategies. Crit Care Nurse 34:24–35
Office for National Statistics (ONS) (2013) Deaths involving Clostridium difficile, England and Wales: 2012. Statistical Bulletin. 22 August 2013
White A (2015) Weekly digest: CDC study reports 29,000 annual US deaths related to C. difficile. Available online at: http://www.cddep.org/blog/posts/weekly_digest_cdc_study_reports_29000_annual_us_deaths_related_c_difficile. Accessed 13 July 16
Planche TD, Davies KA, Coen PG, Finney JM, Monahan IM, Morris KA, O’Connor L, Oakley SJ, Pope CF, Wren MW, Shetty NP, Crook DW, Wilcox MH (2013) Differences in outcome according to Clostridium difficile testing method: a prospective multicentre diagnostic validation study of C difficile infection. Lancet Infect Dis 13:936–945
Arias CA, Murray BE (2012) The rise of the Enterococcus: beyond vancomycin resistance. Nat Rev Microbiol 10:266–278
Sreeja S, Sreenivasa Babu PR, Prathab AG (2012) The prevalence and the characterization of the enterococcus species from various clinical samples in a tertiary care hospital. J Clin Diagn Res 6:1486–1488
Zirakzadeh A, Patel R (2006) Vancomycin-resistant enterococci: colonization, infection, detection, and treatment. Mayo Clin Proc 81:529–536
Werner G, Coque TM, Hammerum AM, Hope R, Hryniewicz W, Johnson A, Klare I, Kristinsson KG, Leclercq R, Lester CH, Lillie M, Novais C, Olsson-Liljequist B, Peixe LV, Sadowy E, Simonsen GS, Top J, Vuopio-Varkila J, Willems RJ, Witte W, Woodford N (2008) Emergence and spread of vancomycin resistance among enterococci in Europe. Euro Surveill 13:19046
Werner G, Klare I, Fleige C, Geringer U, Witte W, Just HM, Ziegler R (2012) Vancomycin-resistant vanB-type Enterococcus faecium isolates expressing varying levels of vancomycin resistance and being highly prevalent among neonatal patients in a single ICU. Antimicrob Resist Infect Control 1:21
Li S, Li J, Qiao Y, Ning X, Zeng T, Shen X (2014) Prevalence and invasiveness of community-acquired methicillin-resistant Staphylococcus aureus: a meta-analysis. Indian J Pathol Microbiol 57:418–422
Sastre A, Roberts PF, Presutti RJ (2013) A practical guide to community-acquired MRSA. J Fam Pract 62:624–629
Leclercq R (2009) Epidemiological and resistance issues in multidrug-resistant staphylococci and enterococci. Clin Microbiol Infect 15:224–231
Rohr U, Kaminski A, Wilhelm M, Jurzik L, Gatermann S, Muhr G (2009) Colonization of patients and contamination of the patients’ environment by MRSA under conditions of single-room isolation. Int J Hyg Environ Health 212:209–215
Polisena J, Chen S, Cimon K, McGill S, Forward K, Gardam M (2011) Clinical effectiveness of rapid tests for methicillin resistant Staphylococcus aureus (MRSA) in hospitalized patients: a systematic review. BMC Infect Dis 11:336
Roisin S, Laurent C, Denis O, Dramaix M, Nonhoff C, Hallin M, Byl B, Struelens MJ (2014) Impact of rapid molecular screening at hospital admission on nosocomial transmission of methicillin-resistant Staphylococcus aureus: cluster randomised trial. PLoS One 9, e96310
Burnham CA, Carroll KC (2013) Diagnosis of Clostridium difficile infection: an ongoing conundrum for clinicians and for clinical laboratories. Clin Microbiol Rev 26:604–630
Hart J, Putsathit P, Knight DR, Sammels L, Riley TV, Keil A (2014) Clostridium difficile infection diagnosis in a paediatric population: comparison of methodologies. Eur J Clin Microbiol Infect Dis 33:1555–1564
Orellana-Miguel MA, Alcolea-Medina A, Barrado-Blanco L, Rodriguez-Otero J, Chaves-Sánchez F (2013) Algorithm proposal based on the C. Diff Quik Chek Complete ICT device for detecting Clostridium difficile infection. Enferm Infecc Microbiol Clin 31:97–99
Surawicz CM, Brandt LJ, Binion DG, Ananthakrishnan AN, Curry SR, Gilligan PH, McFarland LV, Mellow M, Zuckerbraun BS (2013) Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol 108:478–498
Crobach MJ, Planche T, Eckert C, Barbut F, Terveer EM, Dekkers OM, Wilcox MH, Kuijper EJ (2016) European Society of Clinical Microbiology and Infectious Diseases: update of the diagnostic guidance document for Clostridium difficile infection. Clin Microbiol Infect 22(Suppl 4):S63–S81
Jazmati N, Wiegel P, Ličanin B, Plum G (2015) Evaluation of the Qiagen artus C. difficile QS-RGQ Kit for detection of Clostridium difficile toxins A and B in clinical stool specimens. J Clin Microbiol 53:1942–1944
Moon HW, Kim HN, Kim JY, Hur M, Kim H, Yun YM (2016) Performance of the artus C. difficile QS-RGQ kit for the detection of toxigenic Clostridium difficile. Clin Biochem. doi:10.1016/j.clinbiochem.2016.08.013
Alcalá L, Reigadas E, Marín M, Fernández-Chico A, Catalán P, Bouza E (2015) Comparison of GenomEra C. difficile and Xpert C. difficile as confirmatory tests in a multistep algorithm for diagnosis of Clostridium difficile infection. J Clin Microbiol 53:332–335
Beneš J, Husa P, Nyč O, Polívková S (2014) Diagnosis and therapy of Clostridium difficile infection: Czech national guidelines. Klin Mikrobiol Infekc Lek 20:56–66
Bagdasarian N, Rao K, Malani PN (2015) Diagnosis and treatment of Clostridium difficile in adults: a systematic review. JAMA 313:398–408
Peterson LR, Manson RU, Paule SM, Hacek DM, Robicsek A, Thomson RB Jr, Kaul KL (2007) Detection of toxigenic Clostridium difficile in stool samples by real-time polymerase chain reaction for the diagnosis of C. difficile-associated diarrhea. Clin Infect Dis 45:1152–1160
Arends JP, Zhou X, Kampinga GA, Meessen NEL, Friedrich AW (2012) Prevalence of phenotypically vancomycin susceptible, but vanB-PCR positive, Enterococcus faecium: do we overlook VRE vanB carrying strains in our hospital? In: Proceedings of the 22nd European Congress of Clinical Microbiology Infectious Diseases (ECCMID), London, UK, March/April 2012, poster P1289
Mak A, Miller MA, Chong G, Monczak Y (2009) Comparison of PCR and culture for screening of vancomycin-resistant enterococci: highly disparate results for vanA and vanB. J Clin Microbiol 47:4136–4137
Hegstad K, Giske CG, Haldorsen B, Matuschek E, Schønning K, Leegaard TM, Kahlmeter G, Sundsfjord A; NordicAST VRE Detection Study Group (2014) Performance of the EUCAST disk diffusion method, the CLSI agar screen method, and the Vitek 2 automated antimicrobial susceptibility testing system for detection of clinical isolates of enterococci with low- and medium-level VanB-type vancomycin resistance: a multicenter study. J Clin Microbiol 52:1582–1589
Wijesuriya TM, Perry P, Pryce T, Boehm J, Kay I, Flexman J, Coombs GW, Ingram PR (2014) Low vancomycin MICs and fecal densities reduce the sensitivity of screening methods for vancomycin resistance in Enterococci. J Clin Microbiol 52:2829–2833
Ballard SA, Grabsch EA, Johnson PD, Grayson ML (2005) Comparison of three PCR primer sets for identification of vanB gene carriage in feces and correlation with carriage of vancomycin-resistant enterococci: interference by vanB-containing anaerobic bacilli. Antimicrob Agents Chemother 49:77–81
Domingo MC, Huletsky A, Giroux R, Boissinot K, Picard FJ, Lebel P, Ferraro MJ, Bergeron MG (2005) High prevalence of glycopeptide resistance genes vanB, vanD, and vanG not associated with enterococci in human fecal flora. Antimicrob Agents Chemother 49:4784–4786
Graham M, Ballard SA, Grabsch EA, Johnson PDR, Grayson ML (2008) High rates of fecal carriage of nonenterococcal vanB in both children and adults. Antimicrob Agents Chemother 52:1195–1197
Huh HJ, Kim ES, Chae SL (2012) Methicillin-resistant Staphylococcus aureus in nasal surveillance swabs at an intensive care unit: an evaluation of the LightCycler MRSA advanced test. Ann Lab Med 32:407–412
Hos NJ, Wiegel P, Fischer J, Plum G (2016) Comparative evaluation of two fully-automated real-time PCR methods for MRSA admission screening in a tertiary-care hospital. Eur J Clin Microbiol Infect Dis 35:1475–1478
Lee S, Park YJ, Park KG, Jekarl DW, Chae H, Yoo JK, Seo SW, Choi JE, Lim JH, Heo SM, Seo JH (2013) Comparative evaluation of three chromogenic media combined with broth enrichment and the real-time PCR-based Xpert MRSA assay for screening of methicillin-resistant Staphylococcus aureus in nasal swabs. Ann Lab Med 33:255–260
Patel PA, Schora DM, Peterson KE, Grayes A, Boehm S, Peterson LR (2014) Performance of the Cepheid Xpert® SA Nasal Complete PCR assay compared to culture for detection of methicillin-sensitive and methicillin-resistant Staphylococcus aureus colonization. Diagn Microbiol Infect Dis 80:32–34
Yam WC, Siu GK, Ho PL, Ng TK, Que TL, Yip KT, Fok CP, Chen JH, Cheng VC, Yuen KY (2013) Evaluation of the LightCycler methicillin-resistant Staphylococcus aureus (MRSA) advanced test for detection of MRSA nasal colonization. J Clin Microbiol 51:2869–2874
Acknowledgements
We thank QIAGEN for supplying the QIAsymphony RGQ MDx system, artus assays, related reagents and consumables, as well as for their technical expertise. We also thank Cepheid for supplying the Xpert SA Nasal Complete assays and technical advice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Qiagen (grant number 403774_Qiagen_2014).
Conflict of interest
MHW declares that he has the following conflict of interests: I have received consulting fees from Qiagen and grant funding from Cepheid. In addition, QIAGEN supplied the QIAsymphony RGQ MDx system, artus assays, related reagents and consumables, as well as technical expertise. Cepheid supplied the Xpert SA Nasal Complete assays and technical advice.
Ethical approval
No ethical approval was required for this study.
Informed consent
No informed consent was required for this study.
Rights and permissions
About this article
Cite this article
Morris, K.A., Macfarlane-Smith, L.R. & Wilcox, M.H. Evaluation of the novel artus C. difficile QS-RGQ, VanR QS-RGQ and MRSA/SA QS-RGQ assays for the laboratory diagnosis of Clostridium difficile infection (CDI), and for vancomycin-resistant enterococci (VRE) and methicillin-resistant Staphylococcus aureus (MRSA) screening. Eur J Clin Microbiol Infect Dis 36, 823–829 (2017). https://doi.org/10.1007/s10096-016-2867-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-016-2867-6