Abstract
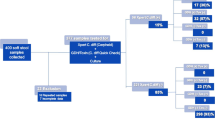
The increasing incidence of Clostridium difficile infection (CDI) in paediatric hospitalised populations, combined with the emergence of hypervirulent strains, community-acquired CDI and the need for prompt treatment and infection control, makes the rapid, accurate diagnosis of CDI crucial. We validated commonly used C. difficile diagnostic tests in a paediatric hospital population. From October 2011 to January 2012, 150 consecutive stools were collected from 75 patients at a tertiary paediatric hospital in Perth, Western Australia. Stools were tested using: C. Diff Quik Chek Complete, Illumigene C. difficile, GeneOhm Cdiff, cycloserine cefoxitin fructose agar (CCFA) culture, and cell culture cytotoxin neutralisation assay (CCNA). The reference standard was growth on CCFA or Cdiff Chromagar and PCR on isolates to detect tcdA, tcdB, cdtA, and cdtB. Isolates were PCR ribotyped. The prevalence of CDI was high (43 % of patients). Quik Chek Complete glutamate dehydrogenase (GDH) demonstrated a low negative predictive value (NPV) (93 %). Both CCNA and Quik Chek Complete toxin A/B had poor sensitivity (33 % and 29 % respectively). Molecular methods both had 89 % sensitivity. Algorithms using GDH + Illumigene or GeneOhm reduced the sensitivity to 85 % and 83 % respectively. Ribotype UK014/20 predominated. GDH NPV and GeneOhm and Illumigene sensitivities were reduced compared with adult studies. Quik Chek Complete and CCNA cannot reliably detect toxigenic CDI. A GDH first algorithm showed reduced sensitivity. In a high prevalence paediatric population, molecular methods alone are recommended over the use of GDH algorithm or culture and CCNA, as they demonstrate the best test performance characteristics.


Similar content being viewed by others
References
Enoch DA, Butler MJ, Pai S, Aliyu SH, Karas JA (2011) Clostridium difficile in children: Colonisation and disease. J Infect 63(2):105–113
Kim J, Smathers SA, Prasad P, Leckerman KH, Coffin S, Zaoutis T (2008) Epidemiological features of Clostridium difficile-associated disease among inpatients at children’s hospitals in the United States, 2001-2006. Pediatrics 122(6):1266–1270
Nylund CM, Goudie A, Garza JM, Fairbrother G, Cohen MB (2011) Clostridium difficile infection in hospitalized children in the United States. Arch Pediatr Adolesc Med 165(5):451–457
Zilberberg M, Tillotson G, McDonald L (2010) Clostridium difficile infections among hospitalized children, United States, 1997–2006. Emerg Infect Dis 16(4):604–609
Sammons JS, Localio R, Xiao R, Coffin SE, Zaoutis T (2013) Clostridium difficile infection is associated with increased risk of death and prolonged hospitalization in children. Clin Infect Dis 57(1):1–8
Freeman J, Bauer MP, Baines SD, Corver J, Fawley WN, Goorhuis B, Kuijper EJ, Wilcox MH (2010) The changing epidemiology of Clostridium difficile infection. Clin Microbiol Rev 23(3):529–549
Toltzis P, Kim J, Dul M, Zoltanski J, Smathers S, Zaoutis T (2009) Presence of the epidemic North American Pulsed Field type 1 Clostridium difficile strain in hospitalized children. J Pediatr 154(4):607–608
Benson L, Song X, Campos J, Singh N (2007) Changing epidemiology of Clostridium difficile-associated disease in children. Infect Control Hosp Epidemiol 28(11):1233–1235
Richards M, Knox J, Elliott B, Mackin K, Lyras D, Waring LJ, Riley TV (2011) Severe infection with Clostridium difficile PCR ribotype 027 acquired in Melbourne, Australia. Med J Aust 194(7):369–371
Crobach MJ, Dekkers OM, Wilcox MH, Kuijper EJ (2009) European Society of Clinical Microbiology and Infectious Diseases (ESCMID): data review and recommendations for diagnosing Clostridium difficile-infection (CDI). Clin Microbiol Infect 15(12):1053–1066
Shetty N, Wren MW, Coen PG (2011) The role of glutamate dehydrogenase for the detection of Clostridium difficile in faecal samples: a meta-analysis. J Hosp Infect 77(1):1–6
O’Horo JC, Jones A, Sternke M, Harper C, Safdar N (2012) Molecular techniques for diagnosis of Clostridium difficile infection: systematic review and meta-analysis. Mayo Clin Proc 87(7):643–651
Kato N, Ou C, Kato H, Bartley S, Brown V, Dowell VD Jr, Ueno K (1991) Identification of toxigenic Clostridium difficile by the polymerase chain reaction. J Clin Microbiol 29(1):33–37
Stubbs S, Rupnik M, Gibert M, Brazier J, Duerden B, Popoff M (2000) Production of actin-specific ADP-ribosyltransferase (binary toxin) by strains of Clostridium difficile. FEMS Microbiol Lett 186:307–312
Kato H, Kato N, Watanabe K, Iwai N, Nakamura H, Yamamoto T, Suzuki K, Kim SM, Chong Y, Wasito EB (1998) Identification of toxin A-negative, toxin B-positive Clostridium difficile by PCR. J Clin Microbiol 36(8):2178–2182
Stubbs S, Brazier J, O’Neill G, Duerden B (1999) PCR targeted to the 16S-23S rRNA gene intergenic spacer region of Clostridium difficile and construction of a library consisting of 116 different PCR ribotypes. J Clin Microbiol 37(2):461–463
Ota KV, McGowan KL (2012) Clostridium difficile testing algorithms using glutamate dehydrogenase antigen and C. difficile toxin enzyme immunoassays with C. difficile nucleic acid amplification testing increase diagnostic yield in a tertiary pediatric population. J Clin Microbiol 50(4):1185–1188
Selvaraju SB, Gripka M, Estes K, Nguyen A, Jackson MA, Selvarangan R (2011) Detection of toxigenic Clostridium difficile in pediatric stool samples: an evaluation of Quik Chek Complete antigen assay, BD GeneOhm Cdiff PCR and ProGastro Cd PCR assays. Diagn Microbiol Infect Dis 71(3):224–229
Luna RA, Boyanton BL Jr, Mehta S, Courtney EM, Webb CR, Revell PA, Versalovic J (2011) Rapid stool based diagnosis of Clostridium difficile infection by real time PCR in a children’s hospital. J Clin Microbiol 49(3):851–857
Toltzis P, Nerandzic MM, Saade E, O’Riordan MA, Smathers S, Zaoutis T, Kim J, Donskey CJ (2012) High proportion of false-positive Clostridium difficile enzyme immunoassays for toxin A and B in paediatric patients. Infect Control Hosp Epidemiol 33(2):175–179
Sharp SE, Ruden LO, Pohl JC, Patricia A, Hatcher PA, Linda M, Jayne LM, Ivie WM (2010) Evaluation of the C.Diff Quik Chek Complete assay, a new glutamate dehydrogenase and A/B toxin combination lateral flow assay for use in rapid, simple diagnosis of Clostridium difficile disease. J Clin Microbiol 48(6):2082–2086
Swindells J, Brenwald N, Reading N, Oppenheim B (2010) Evaluation of diagnostic tests for Clostridium difficile infection. J Clin Microbiol 48(2):606–608
Reyes RC, John MA, Ayotte DL, Covacich A, Milburn S, Hussain Z (2007) Performance of TechLab C. Diff Quik Chek and TechLab C. Difficile Tox A/B II for the detection of Clostridium difficile in stool samples. Diagn Microbiol Infect Dis 59(1):33–37
Kawada M, Annaka M, Kato H, Shibasaki S, Hikosaka K, Mizuno H, Masuda Y, Inamatsu T (2011) Evaluation of a simultaneous detection kit for the glutamate dehydrogenase antigen and toxin A/B in feces for diagnosis of Clostridium difficile infection. J Infect Chemother 17(6):807–811
Dubberke ER, Han Z, Bobo L, Hink T, Lawrence B, Copper S, Hoppe-Bauer J, Burnham CD, Dunne WM (2011) Impact of clinical symptoms on interpretation of diagnostic assays for Clostridium difficile infections. J Clin Microbiol 49(8):2887–2893
Planche TD, Davies KA, Coen PG, Finney JM, Monahan IM, Morris KA, O’Connor L, Oakley SJ, Pope CF, Wren MW, Shetty NP, Crook DW, Wilcox MH (2013) Differences in outcome according to Clostridium difficile testing method: a prospective multicentre diagnostic validation study of C difficile infection. Lancet Infect Dis 13(11):936–945
Norén T, Alriksson I, Andersson J, Akerlund T, Unemo M (2011) Rapid and sensitive loop-mediated isothermal amplification test for Clostridium difficile detection challenges cytotoxin B cell test and culture as gold standard. J Clin Microbiol 49(2):710–711
Drudy D, Fanning S, Kyne L (2007) Toxin A-negative, toxin B-positive Clostridium difficile. Int J Infect Dis 11(1):5–10
Bauer MP, Notermans DW, van Benthem BH, Brazier JS, Wilcox MH, Rupnik M, Monnet DL, van Dissel JT, Kuijper EJ, ECDIS Study Group (2011) Clostridium difficile infection in Europe: a hospital-based survey. Lancet 377(9759):63–73
Acknowledgements
We would like to thank the laboratory staff of the PathWest Laboratory Medicine Princess Margaret Hospital branch and the Queen Elizabeth II Medical Centre branch enteric laboratory.
Ethical standards
As a laboratory-based, non-interventional study ethics committee review was not required.
Conflicts of interest
JH, PP, DK, LS and AK have no conflicts of interest to declare. TVR has received speaker fees, educational grants and travel assistance to attend scientific meetings from Bayer, bioMérieux, GlaxoSmithKine, Genenzyme, Becton Dickinson, Meridian Bioscience, Sanofi and Merck.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hart, J., Putsathit, P., Knight, D.R. et al. Clostridium difficile infection diagnosis in a paediatric population: comparison of methodologies. Eur J Clin Microbiol Infect Dis 33, 1555–1564 (2014). https://doi.org/10.1007/s10096-014-2108-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-014-2108-9