Abstract
During influenza epidemics, influenza-like illnesses (ILIs) viruses cocirculate with influenza strains. If positive, rapid influenza diagnostic tests (RIDTs) identify influenza A/B, but false-negative RIDTs require retesting by viral polymerase chain reaction (PCR). Patient volume limits testing during influenza epidemics, and non-specific laboratory findings have been used for presumptive diagnosis pending definitive viral testing. In adults, the most useful laboratory abnormalities in influenza include relative lymphopenia, monocytosis, and thrombocytopenia. Lymphocyte:monocyte (L:M) ratios may be even more useful. L:M ratios <2 have been used as a surrogate marker for influenza, but there are no longitudinal data on L:M ratios in hospitalized adults with viral ILIs. During the 2015 influenza A (H3N2) epidemic at our hospital, we reviewed our experience with L:M ratios in 37 hospitalized adults with non-influenza viral ILIs. In hospitalized adults with non-influenza A ILIs, the L:M ratios were >2 with human metapneumovirus (hMPV), rhinoviruses/enteroviruses (R/E), and respiratory syncytial virus (RSV), but not human parainfluenza virus type 3 (HPIV-3), which had L:M ratios <2. HPIV-3, like influenza, was accompanied by L:M ratios <2, mimicking influenza A (H3N2). In influenza A admitted adults, L:M ratios <2 did not continue for >3 days, whereas with HPIV-3, L:M ratios <2 persisted for >3 days of hospitalization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Influenza A community-acquired pneumonia (CAP) remains an important cause of mortality and morbidity in hospitalized adults [1, 2]. In winter months, other non-influenza viral influenza-like illnesses (ILIs) cocirculate with influenza strains [2]. In January 2015, influenza A (H3N2) cases reached epidemic proportions, as did non-influenza viral ILIs. In hospitalized adults, the clinical problem is to rapidly differentiate influenza A from ILI mimics of influenza A, e.g., human parainfluenza virus type 3 (HPIV-3) and Legionnaire’s disease (LD) [3–5]. Accurate diagnosis of influenza A is necessary to determine appropriate infection control (IC) precautions, as well as early initiation of anti-influenza therapy [1, 2]. The diagnosis of influenza A in hospitalized adults is usually either by rapid influenza diagnostic tests (RIDTs) or by viral polymerase chain reaction (PCR) of nasopharyngeal swab specimens. RIDTs are commonly used because of their rapidity, simplicity, and low cost, but false-negatives are problematic [6, 7]. There are few false-positives with RIDTs, but frequent false-negatives [6–9]. ILIs with negative RIDTs should be retested by viral PCR [10]. In adults, viral ILIs are most often due to human metapneumovirus (hMPV), coronaviruses (COR), rhinoviruses/enteroviruses (R/E), and respiratory syncytial virus (RSV) [10, 11]. To definitively diagnose non-influenza viral ILIs, viral respiratory PCR is ideal, but requires more time than RIDTs, is expensive, and not available everywhere [10]. When testing demands are exceeded during epidemics, non-specific laboratory findings have been used as surrogate influenza markers, pending definitive PCR diagnosis [12–15].
Excluding viruses, the infectious disease most likely to resemble influenza A is LD [3, 4]. Clinically, LD may be excluded in patients with ILIs with focal/segmental infiltrates on chest X-ray (CXR), particularly if accompanied by, otherwise unexplained, hypophosphatemia, high erythrocyte sedimentation rate (ESR; ≥90 mm/h), highly elevated ferritin (≥2 xn), or microscopic hematuria [16, 17].
For a presumptive influenza diagnosis, non-specific laboratory indicators have been used, e.g., relative lymphopenia, monocytosis, thrombocytopenia, and, depending upon the strain of influenza A (H1N1 vs. H3N2), leukocytosis or leukopenia. Influenza A (H3N2) strains were associated with leukopenia, particularly if, in contrast, severe during the 2009–2010 swine influenza A (H1N1) pandemic, leukocytosis, not leukopenia, was the rule [18–20]. The lymphocyte:monocyte (L:M) ratio has been used as a surrogate marker for influenza A [21, 22]. In admitted adults with ILIs, L:M ratios are readily available and useful pending influenza testing. A longitudinal study of L:M ratios has been reported in healthy/young human volunteers with induced infections [23]. However, there are no longitudinal data on L:M ratios in viral ILIs in hospitalized adults during influenza A (H3N2) epidemics.
Materials and methods
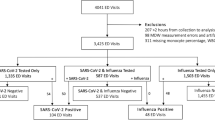
During January 2015 at Winthrop University Hospital, during the influenza A (H3N2) epidemic, 37 adults were admitted with non-influenza ILIs who had a specific viral diagnosis by viral PCR of nasopharyngeal swab specimens. Data on the 37 adult ILIs were reviewed for relative lymphopenia, monocytosis, thrombocytopenia, and L:M ratios. These non-specific test abnormalities were reviewed on admission, during hospital days 1–3, and after 3 days of hospitalization. Longitudinal L:M ratios were calculated during each patient’s hospitalization.
Results
Among 37 ILIs in hospitalized adults, there were four patients with hMPV, two patients with COR, ten patients with R/E, 16 patients with RSV, and five patients with HPIV-3. Relative lymphopenia and monocytosis, but not thrombocytopenia, was common in the non-influenza ILIs. L:M ratios were >2 with hMPV, R/E, and RSV. However, HPIV-3 patients were unique in having L:M ratios <2, mimicking influenza A (H3N2) (Table 1).
The HPIV-3 subset showed not only L:M ratios <2 on admission, but L:M ratios <2 were persistent during hospitalization. Since influenza is a “3 day illness”, the clinical usefulness of L:M ratios is in the early diagnosis of influenza A, i.e., during the first 3 days. With influenza A (H3N2), L:M ratios <2 were present on admission, but did not persist >3 days. In contrast, HPIV-3 L:M ratios <2 persisted for >3 days, and in one case (a 67-year-old male) of HPIV-3 pneumonia, L:M ratios <2 persisted during hospitalization (21 days) (Fig. 1).
Discussion
Specific viral diagnosis of influenza and non-influenza viral ILIs are diagnosed by viral PCR of nasopharyngeal swab specimens [10]. Unfortunately, viral PCR is not utilized/available everywhere. It is important in admitted adults from an IC perspective, to differentiate influenza from viral ILIs. Viral ILIs may be placed on droplet and contact precautions and cohorted, as with influenza [15, 17]. However, without specific testing, it is usually not possible to clinically differentiate viral ILIs [1, 2]. RIDTs are readily available, inexpensive, and useful when positive, but negative RIDTs do not rule out influenza and require specific PCR retesting for definitive diagnosis [6–9]. During influenza epidemics, when testing abilities are stressed and single beds limited, clinicians have used non-specific laboratory test abnormalities as surrogate influenza markers [8, 12].
The most commonly reported surrogate markers for influenza A in hospitalized adults include leukopenia or leukocytosis (depending upon the influenza A strain, i.e., H1N1 or H3N2 ), relative lymphopenia, monocytosis, and thrombocytopenia [13, 14, 18, 20, 21]. In addition, L:M ratios <2 have been used as an indicator of influenza A [21, 23]. L:M ratios have the advantage of being readily and rapidly available. There are no longitudinal data on L:M ratios in non-influenza viral ILIs in hospitalized adults during influenza A (H3N2) epidemics. Published data from young healthy volunteers after viral challenge indicated that R/E and RSV L:M ratios were expectedly >2 [23]. However, there are no data on L:M ratios on hospitalized adults with naturally acquired hMPV or HPIV-3 infections. In reviewing our experience with hospitalized adults during the 2015 influenza epidemic at our hospital, we were able to analyze 37 ILI patients diagnosed by PCR. The L:M ratios of non-influenza viral ILIs depended on viral type. L:M ratios >2 were present with ILIs due to R/E, RSV, and hMPV. In contrast, HPIV-3 patients had L:M ratios <2, mimicking influenza A (H3N2). Interestingly, L:M ratios in HPIV-3 patients were present on admission and persisted for >3 hospital days.
During the influenza A (H3N2) epidemic in hospitalized adults, we found that L:M ratios <2 was a surrogate marker for influenza A but did not persist for >3 days. In patients with non-influenza viral ILIs, with the exception of HPIV-3, L:M ratios <2 may be used to differentiate viral ILIs from influenza A (H3N2). Patients with HPIV-3 had L:M ratios <2 on admission and persisted for >3 days into hospitalization. L:M ratios may be useful not only in differentiating influenza from ILI viruses, but may also have important infection control and therapeutic implications, i.e., oseltamivir therapy for those ILIs with L:M ratios <2. We conclude that HPIV-3 mimics influenza A (H3N2) in hospitalized adults with relative lymphopenia, monocytosis, and L:M ratios <2 [14, 15]. Unlike influenza A (H3N2) or other respiratory viral ILIs, HPIV-3 L:M ratios persisted for >3 days into hospitalization. Clinicians should be aware that, in hospitalized adults, HPIV-3, among viral ILIs, is most likely to mimic influenza, with L:M ratios <2 [5, 11, 17, 24, 25]. Based on our experience, L:M ratios <2 should not be used to differentiate influenza A (H3N2) from HPIV-3 in hospitalized adults.
References
Ruuskanen O, Lahti E, Jennings LC, Murdoch DR (2011) Viral pneumonia. Lancet 377:1264–1275
Cesario TC (2012) Viruses associated with pneumonia in adults. Clin Infect Dis 55:107–113
Cunha BA, Mickail N, Thekkel V (2010) Unexplained increased incidence of Legionnaires disease during the “Herald Wave” of the H1N1 influenza pandemic. Infect Control Hosp Epidemiol 31:562–563
Cunha BA, Mickail N, Syed U, Strollo S, Laguerre M (2010) Rapid clinical diagnosis of Legionnaires’ disease during the “herald wave” of the swine influenza (H1N1) pandemic: the Legionnaires’ disease triad. Heart Lung 39:249–259
Cunha BA, Corbett M, Mickail N (2011) Human parainfluenza virus type 3 (HPIV 3) viral community-acquired pneumonia (CAP) mimicking swine influenza (H1N1) during the swine flu pandemic. Heart Lung 40:76–80
Uyeki T (2009) Diagnostic testing for 2009 pandemic influenza A (H1N1) virus infection in hospitalized patients. N Engl J Med 361:e114
Faix DJ, Sherman SS, Waterman SH (2009) Rapid-test sensitivity for novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med 361:728–729
Cunha BA, Syed U, Mickail N, Strollo S (2010) Rapid clinical diagnosis in fatal swine influenza (H1N1) pneumonia in an adult with negative rapid influenza diagnostic tests (RIDTs): diagnostic swine influenza triad. Heart Lung 39:78–86
Schofield R, Trent RJ (2010) Swine flu: false-positive rapid flu swab with resulting misdiagnosis of a case of Legionella pneumonia. BMJ Case Rep. pii: bcr1220092519
Marcone DN, Carballal G, Ricarte C, Echavarria M (2015) Respiratory viral diagnosis by using an automated system of multiplex PCR (FilmArray) compared to conventional methods. Rev Argent Microbiol 47:29–35
Pavia AT (2011) Viral infections of the lower respiratory tract: old viruses, new viruses, and the role of diagnosis. Clin Infect Dis 52:S284–S289
Cunha BA, Pherez FM, Schoch P (2009) Diagnostic Importance of relative lymphopenia as a marker of swine influenza (H1N1) in adults. Clin Infect Dis 49:1454–1456
Coşkun O, Avci IY, Sener K, Yaman H, Ogur R, Bodur H et al (2010) Relative lymphopenia and monocytosis may be considered as a surrogate marker of pandemic influenza a (H1N1). J Clin Virol 47:388–389
Cunha BA, Syed U, Strollo S (2010) Non-specific laboratory test indicators of severity in hospitalized adults with swine influenza (H1N1) pneumonia. Eur J Clin Microbiol Infect Dis 29:1583–1588
Hage JE, Petelin A, Cunha BA (2011) Before influenza tests results are available, can droplet precautions be instituted if influenza is suggested by leukopenia, relative lymphopenia, or thrombocytopenia? Am J Infect Control 39:619–621
Cunha BA (2008) Atypical pneumonias: current clinical concepts focusing on Legionnaires' disease. Curr Opin Pulm Med 14:183–194
Cunha BA (2010) Pneumonia essentials, 3rd edn. Jones & Bartlett, Sudbury
Cunha BA (2010) Swine influenza (H1N1) pneumonia: clinical considerations. Infect Dis Clin North Am 24:203–228
Kaji M, Watanabe A, Aizawa H (2003) Differences in clinical features between influenza A H1N1, A H3N2, and B in adult patients. Respirology 8:231–233
Cunha BA, Pherez FM, Strollo S, Syed U, Laguerre M (2011) Severe swine influenza A (H1N1) versus severe human seasonal influenza A (H3N2): clinical comparisons. Heart Lung 40:257–261
Merekoulias G, Alexopoulos EC, Belezos T, Panagiotopoulou E, Jelastopulu DM (2010) Lymphocyte to monocyte ratio as a screening tool for influenza. PLoS Curr 2:RRN1154
Huang Y, Zaas AK, Rao A, Dobigeon N, Woolf PJ, Veldman T et al (2011) Temporal dynamics of host molecular responses differentiate symptomatic and asymptomatic influenza A infection. PLoS Genet 7:e1002234
McClain MT, Park LP, Nicholson B, Veldman T, Zaas AK, Turner R et al (2013) Longitudinal analysis of leukocyte differentials in peripheral blood of patients with acute respiratory viral infections. J Clin Virol 58:689–695
Yamakoshi M, Suzuki K, Yamamoto T, Shinagawa N, Nakakita T, Goto N et al (1999) An outbreak of parainfluenza 3 virus infection in the elderly in a ward. Kansenshogaku Zasshi 73:298–304
Marx A, Gary HE Jr, Marston BJ, Erdman DD, Breiman RF, Török TJ et al (1999) Parainfluenza virus infection among adults hospitalized for lower respiratory tract infection. Clin Infect Dis 29:134–140
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare there is no conflict of interest in the publication of this article.
Rights and permissions
About this article
Cite this article
Cunha, B.A., Connolly, J.J. & Irshad, N. The clinical usefulness of lymphocyte:monocyte ratios in differentiating influenza from viral non-influenza-like illnesses in hospitalized adults during the 2015 influenza A (H3N2) epidemic: the uniqueness of HPIV-3 mimicking influenza A. Eur J Clin Microbiol Infect Dis 35, 155–158 (2016). https://doi.org/10.1007/s10096-015-2521-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-015-2521-8