Abstract
The purpose of this investigation was to determine the proportion of influenza-like illness (ILI) attributable to specific viruses during the influenza A(H1N1)2009 pandemic and to describe the demographic and clinical characteristics of ILI due to respiratory viruses in Belgium. Nasopharyngeal swabs were collected from ILI patients by general practitioners (GPs) and paediatricians (PediSurv) and analysed for viruses. Of 139 samples collected from children <5 years of age by PediSurv, 86 were positive, including 28 influenza (20%), 27 respiratory syncytial virus (RSV) (19%), 21 rhinovirus (17%), 12 human metapneumovirus (hMPV) (9%) and ten parainfluenza virus (PIV) (7%). Of 810 samples received from GPs, 426 were influenza (53%). Of 312 influenza-negative samples, 41 were rhinovirus (13%), 13 RSV (4%), 11 PIV (4%) and three hMPV (1%). Influenza mostly affected the 6–15 years old age group. Other respiratory viruses were commonly detected in the youngest patients. Similar clinical symptoms were associated with different respiratory viruses. Influenza A(H1N1)2009 was the most detected virus in ILI patients during the 2009–2010 winter, suggesting a good correlation between ILI case definition and influenza diagnosis. However, in children under 5 years of age, other respiratory viruses such as RSV were frequently diagnosed. Furthermore, our findings do not suggest that the early occurrence of the influenza A(H1N1)2009 epidemic impacted the RSV epidemic in Belgium.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The rapid global spread of influenza A(H1N1)2009 surprised the world and triggered a series of surveillance actions to monitor and characterise the influenza epidemic in each country. In Belgium, several surveillance actions were taken, including the virological surveillance of patients presenting with influenza-like illness (ILI) to primary healthcare providers. Few manuscripts reported on the occurrence of respiratory viruses other than influenza A(H1N1)2009 during the pandemic wave. We collected information on the viral cause of ILI during the A(H1N1)2009 epidemic in Belgium. We used real-time polymerase chain reaction (PCR) to detect nine respiratory viruses in samples from patients presenting with ILI to paediatricians and general practitioners (GPs). Our objective was to determine the proportion of ILI attributable to influenza and other viral pathogens in Belgium during the A(H1N1)2009 pandemic, and to describe the demographic and clinical characteristics of ILI due to different respiratory viruses in Belgium.
Materials and methods
Sample collection
Nasopharyngeal samples were collected from patients presenting with ILI through two surveillance networks.
The PediSurv network was implemented in 2002 and comprises 440 paediatricians and GPs spread throughout Belgium. Based on geographical location, 69 paediatricians were selected to collect two nasopharyngeal and two throat swabs from the first two patients under 5 years of age presenting with ILI each month during the weeks from week 43 in 2009 to week 17 in 2010 [1]. Already hospitalised patients were excluded. The case definition for ILI in children was the sudden onset of fever in the presence of at least one respiratory symptom (cough, rhinitis, sore throat etc.).
In addition, the sentinel surveillance network of general practitioners (GPs), participating since 2007 in the virological surveillance of seasonal flu, was enlarged to 139 GPs during the influenza A(H1N1)2009 epidemic [2]. GPs were asked to collect two nasopharyngeal and two throat swabs from the first two patients presenting with ILI each week during the weeks from week 40 in 2009 to week 20 in 2010. The ILI case definition was the sudden onset of fever in the presence of systemic and respiratory symptoms.
For each patient, information on gender, age, symptoms, influenza vaccination status, hospitalisation status, antiviral treatment and risk factors was collected. Verbal informed consent was obtained from all participants. All four swabs were collected in one tube of transport medium (Tube Copan M10125, MLS, Belgium) and sent to the laboratory by post.
Virus identification
Samples collected by PediSurv were analysed for the detection of influenza A(H1N1)2009 by the CEMOL Laboratory of the University Hospital Gasthuisberg, Leuven, using Nuclisens easyMAG extraction (bioMérieux, Boxtel, The Netherlands) for viral RNA extraction, followed by real time reverse transcription (RT)-PCR on an ABI 7900 (Applied Biosystems, Foster City, CA, USA) using the EXPRESS One-Step Superscript qRT-PCR kit (Invitrogen, Carlsbad, CA) and primers and probe targeting the influenza A(H1N1)2009 hemagglutinin gene.
All other tests were performed at the laboratory of the Scientific Institute of Public Health. Viral RNA was extracted using the QIAamp® Viral RNA kit (QIAGEN, Hilden, Germany) and submitted to a series of real-time RT-PCRs on a Stratagene Mx3000P™ using the SuperScript® III Platinum® One-Step qRT-PCR System (Invitrogen, Carlsbad, CA, USA) or the Brilliant QRT-PCR Core Reagent kit (Stratagene, Amsterdam, The Netherlands). Primers and probes for the identification of influenza A(H1N1)2009 virus were provided by the Centers for Disease Control and Prevention (CDC) [3]. Primers and probes for the identification of human metapneumoviruses [4] and parainfluenza viruses (1,3) [5] were described previously. Other respiratory viruses were detected using primers and probes targeting conserved regions within the genes: (i) PIV-2 hemagglutinin-neuraminidase, (ii) respiratory syncytial virus (RSV)-A and RSV-B nucleocapsid genes, and (iii) rhinovirus 5′ untranslated region. The amplification protocols, primers and probes used are available from the authors upon request. All primers and probes were ordered from Integrated DNA Technologies (Leuven, Belgium).
Statistical analysis
The distribution of clinical symptoms by viral aetiology was determined independently for both data sets (GPs and PediSurv), as were additional statistical analyses. Of note, influenza-positive samples collected by GPs were not tested for other respiratory viruses, and, therefore, influenza co-infections could have biased statistical analyses. Also, the limited battery of respiratory viruses/bacteria tested for might have impacted the statistical analysis.
2 × 2 contingency tables were created to analyse the relation between a virus and a single symptom. For example, the number of influenza-infected individuals (co-infections excluded) and the number of all influenza-negative individuals were stratified according to the appearance of cough. Odds ratios and their confidence intervals (95% CI) and crude p-values were calculated using Fisher’s exact test to evaluate the association between viruses and symptoms. To correct for multiple comparisons in a series of multiple hypothesis tests, we calculated the false discovery rate (FDR) adjusted p-values [6]. Only variables that were found to be statistically associated are reported. The positive predictive value (PPV) of associated viruses and symptoms were calculated as well. All analyses were done using Stata 10 or R (version 2.11.1).
Results
PediSurv network
From PediSurv, we received 139 samples from children younger than 5 years of age, of which 79 were male and 60 were female. Seven patients required hospitalisation and eight patients belonged to one of eight predefined risk groups (chronic respiratory or cardiac disease, moderate to severe kidney or liver insufficiency, diabetes, immunodeficiency, neuromuscular problems or chronic neurological disease, congenital metabolic disease). Of the 139 patients, three were vaccinated for seasonal flu and two for the pandemic variant.
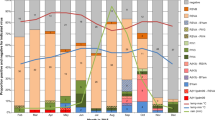
The number of positive samples by virus and sampling week is shown in Table 1. The corresponding percentage is calculated from the weekly received number of samples. Eighty-six of the 139 samples were positive for at least one virus (62%), including 28 influenza (20%), 27 RSV (19%), 21 rhinovirus (17%), 12 human metapneumovirus (hMPV) (9%) and ten parainfluenza virus (PIV) (7%). Twelve co-infections were detected. Of the influenza isolates, 27 were influenza A(H1N1)2009 and one influenza B. Influenza was the most common virus during weeks 42–49 of 2009, whereas RSV was the most frequently detected during weeks 50–52 of 2009 and hMPV during weeks 5–7 of 2010. PIV was infrequently detected and rhinoviruses could be identified throughout the whole study period. During the co-circulation of rhinovirus and influenza A(H1N1)2009 (weeks 42–49), two rhinovirus infections were identified in 22 children infected with influenza A(H1N1)2009 compared to nine rhinovirus detections in 44 influenza-negative cases. During the co-circulation of RSV and influenza A(H1N1)2009 (weeks 46–49), one RSV was detected in 11 children infected with influenza A(H1N1)2009 in comparison to eight RSV detections in 23 influenza-negative cases. The odds ratio for rhinovirus detection in influenza A(H1N1)2009-positive samples was estimated to be 0.39 (95% CI 0.04–2.18), p = 0.31 (Fisher’s exact test) and the odds ratio for RSV detection in influenza A(H1N1)2009-positive samples was estimated to be 0.20 (95% CI 0.01–1.87), p = 0.21 (Fisher’s exact test).
The number of samples by virus and symptom is shown in Table 2. The most common clinical findings (besides symptoms included in the ILI case definition) in children under 5 years of age infected with influenza (n = 25) were cough (n = 21), rhinitis (n = 20) and pharyngitis (n = 15). These symptoms were also commonly associated with other respiratory viruses. All RSV-infected children (n = 19) coughed and 18 had rhinitis. Moreover, 11 of 12 rhinovirus-infected children coughed and had rhinitis and eight had pharyngitis. Also, all hMPV-infected children (n = 10) coughed and had rhinitis, and seven had pharyngitis. PIV-infected children (n = 9) had pharyngitis (n = 8), rhinitis (n = 7) and coughed (n = 8). Odds ratios were calculated to identify associations between symptoms and specific viruses. To control for false-positive associations in this setting of multiple hypothesis testing, FDR adjusted p-values were calculated. Only associations with FDR adjusted p-values < 0.05 were regarded as true associations. Analysis revealed that rhonchi/wheezing was more likely to be reported in children infected with RSV (odds ratio 8.25 [2.51–28.10], FDR adjusted p = 0.0095); however, this symptom had a low PPV (43%) for identifying RSV infection in children. On the other hand, grouping RSV and hMPV resulted in a PPV of 61% for rhonchi/wheezing to identify RSV/hMPV infection in children.
Network of general practitioners
Samples received weekly from the GP network were first analysed for influenza. A subset of samples which remained undiagnosed were submitted to real-time RT-PCRs, which detect RSV (A, B), hMPV, PIV (1, 2, 3) and rhinoviruses. To allow the tracking of virus epidemic trends, all samples of each one out of four weeks were analysed. When the sample number was low, samples from adjacent weeks were analysed. In total, 810 samples (of which 18 were from influenza A(H1N1)2009-vaccinated patients) from nine different weeks during the winter season of 2009–2010 were analysed for influenza, and 312 influenza-negative samples were analysed for other respiratory viruses.
The number of samples by virus and sampling week is shown in Table 3. For influenza, the corresponding percentage is calculated from the number of weekly received samples. For other respiratory viruses, the corresponding percentage is calculated from the number of influenza-negative samples analysed for a specific week. Of 810 samples, 426 were influenza-positive (53%), with 423 influenza A(H1N1)2009 and three influenza B. Of 312 influenza-negative samples, 41 were rhinovirus (13%), 13 RSV (4%), 11 PIV (4%) and three hMPV (1%). Three co-infections were detected. Overall, we were able to detect respiratory viruses (including influenza) in 491/738 samples (67%). Influenza was the most common virus detected in weeks 43 of 2009 and 47 of 2009, whereas RSV was the most frequently detected during week 51 of 2009. hMPV was only infrequently detected, and PIV and rhinoviruses could be identified throughout the whole study period.
The distribution of analysed samples by virus and patient age class is shown in Table 4. The proportion of influenza-positive samples was highest in the 6–15 years old age group, and only 3 out of 18 patients ≥65 years of age tested influenza-positive. The proportion of RSV-positive and hMPV-positive samples was highest in the youngest age group. PIV infections were mostly detected in the youngest patients and the elderly, and rhinoviruses were most commonly detected in the elderly. Overall, respiratory viruses other than influenza accounted for 28% of ILI cases in both children under 5 years of age and the elderly.
The number of positive samples, by virus and by symptom, is shown in Table 5. Fever was not included in the table because it was often inadequately recorded. The most common symptoms (besides symptoms included in the ILI case definition) in ILI patients with influenza (n = 426) were shivers (n = 334), asthaenia (n = 316), headache (n = 349) and cough (n = 374). RSV-infected patients (n = 10) most commonly coughed (n = 10), had asthaenia (n = 9), coryza (n = 8) and loss of appetite (n = 8). Of 41 rhinovirus-infected patients, 34 coughed and 31 had shivers. All hMPV-infected patients (n = 3) coughed and had asthaenia, myalgia and coryza. PIV-infected patients (n = 10) most commonly had headache (n = 7), myalgia (n = 7) and coryza (n = 7). Odds ratios were calculated in order to identify associations between symptoms and specific viruses. Only associations with FDR adjusted p-values < 0.05 are regarded as true associations. Analysis revealed that cough (odds ratio 3.39 [2.30–5.04], FDR adjusted p = 4.11 × 10−9) and ocular symptoms (odds ratio 1.72 [1.21–2.47], FDR adjusted p = 0.043) were more likely to be reported in influenza-infected patients. Of note, cough and ocular symptoms had a PPV of 64 and 67%, respectively, for identifying influenza and the PPV of the combination of these two symptoms was 73%. The odds ratio of the combination of cough and ocular symptoms was estimated to be 2.36 (1.59–3.55) (FDR adjusted p = 2.09 × 10−4).
Discussion
In the two surveillance studies performed during the 2009–2010 winter in Belgium, 62 or 67% of all ILI samples collected were positive for at least one respiratory virus. These results are in line with previous reports on the viral causes of ILI during the influenza A(H1N1)2009 pandemic, with detection frequencies ranging from 37% [7] to 61% [8] to 89% [9], depending on when the samples were collected, which and how many viruses were tested, and which population groups were studied. In Belgium, influenza was the most common viral cause of ILI in both study groups, with 20% (PediSurv) and 53% of influenza-positive samples (GP group). Even moreso, during the influenza epidemic period in Belgium (weeks 40–49 of 2009), 33% (22/66) of ILI samples collected by PediSurv and 62% (400/644) of samples collected by GPs were influenza-positive, suggesting a good correlation between ILI case definition and influenza diagnosis in the GP study.
On the other hand, when breaking down the data into age groups, two particular observations can be made. First, in the elderly (≥65 years of age), other respiratory viruses than influenza were more commonly detected (28% vs. 17%, respectively), although it should be mentioned that the sample number was low (n = 18) and four patients were vaccinated for seasonal influenza, of which two of these patients also received one dose of the monovalent Pandemrix vaccine six weeks before sampling. Lower attack rates among persons ≥65 years of age were reported by several studies investigating respiratory infection outbreaks in long-term care facilities for the elderly during the early stages of the 2009 pandemic [9, 10]. The sparing of the elderly by influenza A(H1N1)2009 could be due to cross-reactive antibodies from previous exposure to A(H1N1) strains. Early data from the influenza A(H1N1)2009 outbreak indicated anti-influenza A antibodies that cross-react with 2009 H1N1 could be detected in up to one-third of healthy adults >60 years of age [10].
Secondly, although the results showed influenza to be the most commonly detected virus among children under the age of 5 years, this population group was frequently infected by other respiratory viruses as well, with the most commonly detected viruses being RSV (19% and 13% in either study) and rhinoviruses (15% and 6% in either study). hMPV and PIV were found in smaller percentages, ranging from 9 to 2% of ILI cases in either study. By adding up all of the positive detections for respiratory viruses other than influenza, we evaluated the specificity of the ILI case definition for influenza diagnosis in children under the age of 5 years; 67/139 (50%) other respiratory viruses infections compared to 28/139 (20%) influenza infections in the PediSurv group and 13/47 (28%) other respiratory viruses to 21/44 (45%) influenza infections in the GP study group were detected during the whole period. The results differ to some extent between both study groups, which might be due to the low number of children under the age of 5 years included in the GP study, the years of experience of the GPs in ILI surveillance compared to the paediatricians of the PediSurv group and the different test protocols used (no detection of influenza co-infections in the GP study). Still, our findings confirm the aspecificity of ILI criteria for influenza diagnosis in children; the clinical presentation of A(H1N1)2009 infection is largely indistinguishable from that of other respiratory viral infections, but it should still be used as a guide for whom needs testing.
Identifying respiratory virus infection on the basis of clinical symptoms is a widely known difficulty. Previous studies reporting on symptoms associated with influenza showed cough and fever as the best predictors for influenza infection in adults [11–14], or muscle/joint pain and nasal congestion to be associated with influenza in all age groups [15]. In children, fever, headache, cough and absence of abnormal breathing sounds [14] or cough, headache and pharyngitis [16] or myalgia (among 1–5-year-olds) [17] were reported to be associated with influenza. Recent reports on the clinical features associated with A(H1N1)2009 influenza in children showed that headache and myalgia were positively associated [18] or fever, rhinorrhoea, a normal chest radiograph and the absence of leukocytosis or significant gastrointestinal symptoms were positively associated [19]. As for RSV, cough, wheezing and retractions were previously reported to be independent variables predictive of RSV infection in children [20]. In this study, the statistical analysis of clinical symptoms demonstrated few positive associations with specific viral agents, probably due to the limited number of samples. However, cough and ocular symptoms were statistically significant positively associated with influenza in the GP study group, whereas rhonchi/wheezing were positively associated with RSV in children under 5 years of age (PediSurv). Our findings are in concordance with previous results and may help clinicians to perform diagnosis.
It has been suggested that the influenza A(H1N1)2009 wave might have been impacted or might have had an impact on the pattern of other respiratory viruses (viral interference) commonly observed during the winter months, such as rhinoviruses and RSV [21, 22]. It is not clear from our data whether rhinoviruses might have impacted the emergence of the influenza A(H1N1)2009 pandemic in Belgium, since rhinoviruses typically peak soon after the start of school term and this period was not included in our study. However, during the study period, rhinoviruses, RSV and influenza co-circulated but had different temporal distributions. Still, the statistical analysis of co-detection data from the PediSurv study could not corroborate negative associations between the detection of rhinovirus or RSV and influenza A(H1N1)2009 in Belgium. RSV circulating patterns during the influenza A(H1N1)2009 wave in Belgium compared to previous years showed great regularity, with a peak around weeks 49–50. These data do not suggest that the early occurrence of the influenza A(H1N1)2009 epidemic had an impact on the RSV epidemic in Belgium.
As mentioned throughout the manuscript, there were several limitations to this study. Firstly, some relevant respiratory viruses and bacteria were not studied. Nevertheless, the viral detection frequency in this study (62–67%) did not differ extensively from those in other studies [7–9]. Secondly, only a limited number of samples were analysed, and, thirdly, not all samples were analysed similarly for both surveillance studies, which could have biased the statistical analysis and limits the conclusions to be drawn.
Still, both surveillance networks provided high-quality information during the pandemic, which permitted to monitor the influenza A(H1N1)2009 epidemic in Belgium with confidence. Despite the relatively small size of the PediSurv network, this study collected important additional data on respiratory infections in paediatric patients, a population group which is rather underrepresented in the GP network involved in the yearly surveillance of influenza. The future continuation of paediatric surveillance in addition to the initiation of surveillance networks focused on the elderly in Belgium are warranted. Overall, ILI surveillance is a powerful tool to signal and interpret the relevant microbiological and epidemiological dynamics of respiratory infections.
References
Sabbe M, Hue D, Antoine J, Dupont Y, van Eldere J, Van Ranst M, Thomas I (2010) Influenza surveillance in children: first experiences with the Belgian Paediatric Surveillance system ‘PediSurv’. Available online at: http://www.wiv-isp.be/aph/pdf/aph68_94-99.pdf
Van Casteren V, Mertens K, Antoine J, Wanyama S, Thomas I, Bossuyt N (2010) Clinical surveillance of the Influenza A(H1N1)2009 pandemic through the network of Sentinel General Practitioners. Available online at: http://www.wiv-isp.be/aph/pdf/aph68_62-67.pdf
Centers for Disease Control and Prevention (CDC) (2009) CDC protocol of realtime RTPCR for influenza A(H1N1). Available online at: http://www.who.int/csr/resources/publications/swineflu/CDCRealtimeRTPCR_SwineH1Assay-2009_20090430.pdf
Maertzdorf J, Wang CK, Brown JB, Quinto JD, Chu M, de Graaf M et al (2004) Real-time reverse transcriptase PCR assay for detection of human metapneumoviruses from all known genetic lineages. J Clin Microbiol 42(3):981–986
Cordey S, Thomas Y, Cherpillod P, van Belle S, Tapparel C, Kaiser L (2009) Simultaneous detection of parainfluenza viruses 1 and 3 by real-time reverse transcription-polymerase chain reaction. J Virol Methods 156(1–2):166–168
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Statist Soc B 57(1):289–300
Nisii C, Meschi S, Selleri M, Bordi L, Castilletti C, Valli MB et al (2010) Frequency of detection of upper respiratory tract viruses in patients tested for pandemic H1N1/09 viral infection. J Clin Microbiol 48(9):3383–3385
Follin P, Lindqvist A, Nyström K, Lindh M (2009) A variety of respiratory viruses found in symptomatic travellers returning from countries with ongoing spread of the new influenza A(H1N1)v virus strain. Euro Surveill 14(24):pii.19242
Marchand-Austin A, Farrell DJ, Jamieson FB, Lombardi N, Lombos E, Narang S et al (2009) Respiratory infection in institutions during early stages of pandemic (H1N1) 2009, Canada. Emerg Infect Dis 15(12):2001–2003
Echevarría-Zuno S, Mejía-Aranguré JM, Mar-Obeso AJ, Grajales-Muñiz C, Robles-Pérez E, González-León M et al (2009) Infection and death from influenza A H1N1 virus in Mexico: a retrospective analysis. Lancet 374(9707):2072–2079
Boivin G, Hardy I, Tellier G, Maziade J (2000) Predicting influenza infections during epidemics with use of a clinical case definition. Clin Infect Dis 31(5):1166–1169
Govaert TM, Dinant GJ, Aretz K, Knottnerus JA (1998) The predictive value of influenza symptomatology in elderly people. Fam Pract 15(1):16–22
Monto AS, Gravenstein S, Elliott M, Colopy M, Schweinle J (2000) Clinical signs and symptoms predicting influenza infection. Arch Intern Med 160(21):3243–3247
Sočan M, Prosenc K, Nagode M (2010) Differences in clinical predictors of influenza in adults and children with influenza-like illness. Central Eur J Med 5(1):41–48. doi:10.2478/s11536-009-0089-3
Puzelli S, Valdarchi C, Ciotti M, Dorrucci M, Farchi F, Babakir-Mina M et al (2009) Viral causes of influenza-like illness: insight from a study during the winters 2004–2007. J Med Virol 81(12):2066–2071
Friedman MJ, Attia MW (2004) Clinical predictors of influenza in children. Arch Pediatr Adolesc Med 158(4):391–394
Ohmit SE, Monto AS (2006) Symptomatic predictors of influenza virus positivity in children during the influenza season. Clin Infect Dis 43(5):564–568
Bryant PA, Tebruegge M, Papadakis G, Clarke C, Barnett P, Daley AJ et al (2010) Clinical and microbiologic features associated with novel swine-origin influenza A pandemic 2009 (H1N1) virus in children: a prospective cohort study. Pediatr Infect Dis J 29(8):694–698
Ong AK, Chen MI, Lin L, Tan AS, Nwe NW, Barkham T et al (2009) Improving the clinical diagnosis of influenza—a comparative analysis of new influenza A (H1N1) cases. PLoS One 4(12):e8453
Durani Y, Friedman MJ, Attia MW (2008) Clinical predictors of respiratory syncytial virus infection in children. Pediatr Int 50(3):352–355
Linde A, Rotzén-Ostlund M, Zweygberg-Wirgart B, Rubinova S, Brytting M (2009) Does viral interference affect spread of influenza? Euro Surveill 14(40):pii.19354
Casalegno JS, Bouscambert-Duchamp M, Morfin F, Lina B, Escuret V (2009) Rhinoviruses, A(H1N1)v, RVS: the race for hivernal pandemics, France 2009–2010. Euro Surveill 14(44):pii.19390
Acknowledgements
Special thanks go to all of the general practitioners and paediatricians who participated in the surveillance. Both surveillance networks were financially supported by the Directorate-General for Primary Health Care and Crisis Management (DG2) from the Federal Public Service Health, Food Chain Safety and Environment, and by the French and Flemish Communities. The study was co-funded by the EPIWORK project (Seventh Framework Programme of the European Commission) and by the Institute for the Promotion of Innovation by Science and Technology (IWT) in Flanders (strategic basic research project SIMID). Many thanks go to Christophe Van den Poel, Ilham Fdillate, Mona Abady, Regine De Bruyn, Jeanine Weyckmans, Yvonne Ronflette and Kurt Beuselinck for their excellent technical assistance.
Competing interests
The authors declare that there are no conflicts of interest.
Ethical approval
Verbal informed consent was obtained from all participants.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hombrouck, A., Sabbe, M., Van Casteren, V. et al. Viral aetiology of influenza-like illness in Belgium during the influenza A(H1N1)2009 pandemic. Eur J Clin Microbiol Infect Dis 31, 999–1007 (2012). https://doi.org/10.1007/s10096-011-1398-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-011-1398-4