Abstract
This study investigated the correlation between antibiotic consumption and resistance among Staphylococcus aureus and enterococci causing healthcare-associated infections at a university hospital in Taiwan from 2000 to 2009. Overall, the trend of total consumption (defined daily dose [DDD] per 1,000 patient-days) of glycopeptides, including vancomycin and teicoplanin, significantly increased during 2000 to 2003 and remained stable during 2004–2009. Vancomycin consumption significantly increased during 2003 and decreased after 2004. A significant decrease in the resistance rate with time was found for oxacillin- and gentamicin-resistant S. aureus. In contrast, the rates of vancomycin- and teicoplanin-resistant enterocci increased significantly. A significant correlation was found between the increased use of extended-spectrum cephalosporins, β-lactam-β-lactamase inhibitor combinations, carbapenems and the decreased prevalence of methicillin-resistant S. aureus (MRSA). In contrast, the increased use of teicoplanin, extended-spectrum cephalosporins, β-lactam-β-lactamase inhibitor combinations, and carbapenems was correlated with the increased prevalence of vancomycin-resistant enterococci (VRE). In conclusion, this 10-year study in a single institution identified different correlations between the prescription of antibiotics and the resistance rates of MRSA and VRE. Strict implementation of infection control policy based on these correlates would be helpful in decreasing the presence of these multidrug-resistant pathogens in hospitals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In this era of aged populations and increasing numbers of immunocompromised patients the incidence of healthcare-associated infection (HAI) has risen dramatically and is most often caused by multidrug-resistant bacteria [1, 2]. For Gram-positive bacteria in the US, Staphylococcus aureus is the most common pathogen causing HAI, followed by enterococci [3]. Among these pathogens, methicillin (oxacillin)-resistant S. aureus (MRSA) and vancomycin-resistant enterococci (VRE) are of greatest concern because the resistant pathogens are associated with extended length of hospital stay, higher cost and greater mortality [1, 4].
Although antibiotic use is the most important risk factor for the emergence of bacterial resistance, the nature of this relationship is complicated. Previous studies which examined the relationship between antimicrobial consumption and antibiotic resistance have had inconsistent findings, which may be due to differences in the resistance profiles and antibiotic prescribing practices in different countries [5–10]. The prevalence of MRSA and VRE was shown to be associated with the use of glycopetides, extended-spectrum cephalosporins, and fluoroquinolones [11–18]. This study investigated the correlation between antibiotic consumption and antimicrobial resistance of MRSA and VRE causing healthcare-associated infection from 2000 to 2009 at a medical center in Taiwan.
Materials and methods
Setting and patients
National Taiwan University Hospital (NTUH) is a 2,500-bed, academically affiliated medical center providing both primary and tertiary care in northern Taiwan. The number of annual patient-days at the hospital increased from 624,675 in 2000 to 751,026 in 2009. Linezolid and fusidic acid were introduced in the hospital formulary in 2002. Some of the data analyzed in this study were included in a previous study [5, 6]. Prior to 2004, no specific and well-established antibiotic control polices were implemented at the hospital. All attending physicians at the hospital can prescribe nearly all antimicrobial agents (except for liposomal amphotericin B, voriconazole, caspofungin, linezolid, and ganciclovir) without the permission of the infection disease specialists.
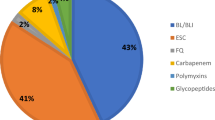
Antimicrobial agents and consumption
Data on annual consumption (defined daily dose [DDD] per 1,000 patient-days) of glycopetides (vancomycin and teicoplanin), linezolid, fusidic acid, extended-spectrum cephalosporins (cefotaxime, ceftriaxone, flumoxef, ceftazidime, cefempime and cefpirome), β-lactam-β-lactamase inhibitor combinations (ticarcillin-clavulanic acid and piperacillin-tazobactam), carbapenems (imipenem, meropenem and ertapenem), aminoglycosides (amikacin and gentamicin), and fluoroquinolones (ciprofloxacin and levofloxacin) from 2000 to 2009 were obtained from the pharmacy department of the hospital.
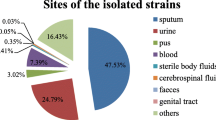
Bacterial isolates
To determine the temporal trend of MRSA and VRE causing health-associated infections at NTUH, data on the disk diffusion susceptibilities of S. aureus to oxacillin and of enterococci to vancomycin among isolates recovered from 2000 to 2009 were retrieved from annual summary documents as previously reported [1, 2]. Definitions for health-associated infections followed the National Nosocomial Infection Surveillance guidelines [19]. These isolates were non-duplicate samples, as several isolates of each species from each patient recovered within 7 days were considered as a single isolate. Susceptibility testing for S. aureus and enterococci followed Clinical and Laboratory Standards Institute (CLSI) guidelines [20]. S. aureus ATCC 25923 and E. faecalis ATCC 29212 were used as control strains for routine disk susceptibility testing [20]. Methicillin resistance in S. aureus was routinely screened for by growth of the isolate on a trypticase soy agar plate containing oxacillin 6 mg/L plus 2% NaCl and incubation in ambient air at 35°C for 24 h [20, 21]. Vancomycin resistance in enterococci was further confirmed by growth of the isolate on a brain heart infusion (BHI) agar with vancomycin 6 mg/L and incubation in ambient air at 35°C for 24 h [20]. S. aureus ATCC 29213, S. aureus ATCC 43300, E. faecalis ATCC 29212 and E. faecalis ATCC 51299 were used as control strains.
Statistical analysis
Linear regression analysis was used to analyze the trends of annual consumption of antimicrobial agents and the trends in the nonsusceptible (including intermediate and resistant) rate of S. aureus and enterococci causing all healthcare-associated infections with time. Because of the emergence of severe acute respiratory syndrome (SARS) in 2003, the trends of annual consumption of antimicrobial agents were analyzed with three time periods: 2000–2003, 2004–2009, and 2000–2009, with linear regression analysis. Pearson’s correlation coefficient was used to determine the relationship between annual antibiotic consumption and trends in resistance. In order to study the lag-time effect, the relationship of the annual consumption of antimicrobial agents and the next year antimicrobial resistance was further explored in pairs using linear regression and Pearson’s correlation analysis. A p value <0.05 was considered statistically significant.
Results
Annual antibiotic consumption
In general, the use of each individual antimicrobial agent varied with time period (Table 1 and Fig. 1). During 2000 to 2003, a significant increase in consumption of glycopetides, extended-spectrum cephalosporins, and fluoroquinolones was found while a decrease in consumption was found for aminoglycosides. From 2004 to 2009, only the prescription of carbapenems and aminoglycosides significantly increased and decreased, respectively. Overall, the consumption of extended-spectrum cephalosporins, β-lactam-β-lactamase inhibitor combinations, carbapenems, and fluoroquinolones significantly increased while the consumption of aminoglycosides decreased during the study period. Vancomycin consumption significantly increased during 2003 (r = 0.96, p = 0.03, b = 2.28) and decreased after 2004 (r = 0.84, p = 0.036, b = −1.00). In contrast, the teicoplanin use remained stable during the study period (r = 0.47, p = 0.18, b = 0.28). In addition, the trend in consumption of linezolid insignificantly increased from 2.2 DDD per 1,000 patient-days in 2002 to 66.5 DDD per 1,000 in 2009, while the trend for fusidic acid use remained stable from 2002 to 2009.
Trend of antimicrobial resistance among S. aureus and enterococci isolates
A total of 4,352 non-duplicate S. aureus and 3,673 enterococci isolates were identified and tested for susceptibility. Table 2 shows the trends in the resistance rate of S. aureus and enterococci isolates. A significant decrease in the resistant rate with time was found for oxacillin- and gentamicin-resistant S. aureus. In contrast, a significant increase in resistance rates was found for vancomycin- and teicoplanin-resistant enterococci.
Correlation between antibiotic consumption and rate of resistance
The correlation between the rates of resistant MRSA and VRE causing healthcare-associated infections and the annual consumption of the specific antibiotics are shown in Tables 3 and 4. A significant correlation was found between the increased use of extended-spectrum cephalosporins, β-lactam-β-lactamase inhibitor combinations, carbapenems and the decreased prevalence of MRSA. In contrast, a significant positive correlation was found between the increased use of teicoplanin, extended-spectrum cephalosporins, β-lactam-β-lactamase inhibitor combinations, carbapenems and the increased prevalence of VRE. Decreased prescription of aminoglycosides was correlated with the decreased prevalence of MRSA and the increased prevalence of VRE.
Discussion
This study evaluated the association between antibiotic consumption and the antimicrobial resistance of MRSA and VRE causing healthcare-associated infection in a medical center in Taiwan during a 10-year period. The first noteworthy finding of this study was that the trend in the consumption of extended-spectrum cephalosporins, β-lactam-β-lactamase inhibitor combinations, carbapenems, and fluoroquinolones significantly increased during the study period; however, the trend for consumption of glycopeptides, with significant increases only during 2000 to 2003, was followed by stable consumption during the next six years. As has been previously documented, the emergence of SARS led to acknowledgement of the need for more stringent infection control measures by physicians and in healthcare-associated infection policy. The revised policies reflected the need for more cautious intervention but not misuse of antibiotics. The slow-down in the increasing use of antibiotics documented in this work thus appears to have resulted from the implementation of infection control intervention measures after the emergence of SARS. In addition, the consumption of aminoglycosides significantly decreased during this period, which is probably attributable to changes in prescription practices due to the notable side effects of these agents.
A second noteworthy finding of this study is that the prevalence of MRSA significantly increased from 71.8% in 2000 to 78.2% in 2002 (peak) and finally decreased to 54.9% in 2009. A similar trend was noted for gentamicin-resistant S. aureus. As stated above, stricter infection control policy after the emergence of SARS and another simple measure—hand washing—have been intensively carried out since 2003. Therefore, the declining prevalence of MRSA could be partly explained by the aggressive policy of infection control and the resulting decreased risk of hand transmission. However, the prevalence VRE and teicoplanin-resistant enterococci significantly increased up to more than 20% during the study period. These differences most likely resulted from the character of the bacteria itself as enterococci colonized the gastrointestinal tract of hospitalized patients. Therefore, more effective infection control interventions continue to be needed to prevent the spread of VRE.
In addition to infection control, we were also interested in the relationship between antibiotic use and the prevalence of MRSA related healthcare-associated infection. In contrast to previous studies [5, 11, 14, 22] we found a negative correlation between the use of extended-spectrum cephalosporins, β-lactam-β-lactamase inhibitor combinations, and carbapenems and the prevalence of MRSA. We demonstrated that the consumption of extended-spectrum cephalosporins and carbapenems reduced the rate of MRSA with a 1-year lag. On the contrary, the prescription of aminoglycosides was positively correlated with the prevalence of MRSA with and without a time lag. Most importantly, all of the MRSA were susceptible to vancomycin and most MRSA remained susceptible to teicoplanin during the 10-year period.
Besides MRSA, the epidemiology of VRE could be affected by the use of antibiotics including third-generation cephalosporins and vancomycin [16]. In this work, we further confirmed that the consumption of teicoplanin, β-lactam-β-lactamase inhibitor combinations, and carbapenems were positively correlated with an increased rate of VRE. In addition, aminoglycosides exerted a protective effect against this resistance, which lasted as long as one year.
This study had one major limitation. Although we found a relationship between antibiotic use and the resistance rate among MRSA and VRE, these results must be interpreted with care. The cause of emergence of drug resistant bacteria in the hospital is complex and selective pressure from widespread use of antimicrobials might only partly explain investigational results. In fact, the prevalence of MRSA and VRE are susceptible to several factors such as infection control measures and hand hygiene, or operational changes in the hospital (such as shorter length of stay because of the shift of procedures or rehabilitation to an outpatient setting, etc.), or even the epidemiology of patients (i.e. shifts towards an ageing population with more chronic diseases over a decade-long period). Their effect was not measured in this study, hence their impact on MRSA and VRE trends remains unknown. Besides, because this was an ecological surveillance, we could not analyze the impact of individual level, duration of exposure to antibiotics or possibility of clonal spreads of resistant bacteria to determine their further correlation with the identified associations.
In conclusion, this 10-year study in an institution provided a profile of the different correlations between the prescription of antibiotics and the resistant rate of MRSA and VRE. Strict implementation of infection control policy including appropriate antimicrobial prescription and simple infection control measures including hand washing are positively correlated with a decreased presence of MRSA in the hospital.
References
Buke C, Armand-Lefevre L, Lolom I, Guerinot W, Deblangy C, Ruimy R, Andremont A, Lucet JC (2007) Epidemiology of multidrug-resistant bacteria in patients with long hospital stays. Infect Control Hosp Epidemiol 28:1255–1260
Gales AC, Jones RN, Andrade SS, Sader HS (2005) Antimicrobial susceptibility patterns of unusual nonfermentative gram-negative bacilli isolated from Latin America: report from the SENTRY Antimicrobial Surveillance Program (1997–2002). Mem Inst Oswaldo Cruz 100:571–577
Hidron AI, Edwards JR, Patel J, Horan TC, Sievert DM, Pollock DA, Fridkin SK, National Healthcare Safety Network Team, Participating National Healthcare Safety Network Facilities (2008) NHSN annual update: antimicrobial-resistant pathogens associated with healthcare-associated infections: annual summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2006-2007. Infect Control Hosp Epidemiol 29:996–1011
Ruttimanns Keck B, Hartmeier C, Maetzel A, Bucher HC (2004) Long-term antibiotic cost saving from a comprehensive intervention program in a medical department of a university-affiliated teaching hospital. Clin Infect Dis 38:348–356
Hsueh PR, Chen WH, Teng LJ, Luh KT (2005) Nosocomial infections due to methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci at a university hospital in Taiwan from 1991 to 2003: resistance trends, antibiotic usage and in vitro activities of newer antimicrobial agents. Int J Antimicrob Agents 26:43–49
Hsueh PR, Chen WH, Luh KT (2005) Relationships between antimicrobial use and antimicrobial resistance in Gram-negative bacteria causing nosocomial infection from 1991–2003 at a university hospital in Taiwan. Int J Antimicrob Agent 26:463–472
Metz-Gercek S, Maieron A, Straub R, Wieninger P, Apfalter P, Mittermayer H (2009) Ten years of antibiotic consumption in ambulatory care: trends in prescribing practice and antibiotic resistance in Austria. BMC Infect Dis 9:61
Cook PP, Catrou PG, Christie JD, Young PD, Polk RE (2004) Reduction in broad-spectrum antimicrobial use associated with no improvement in hospital antibiogram. J Antimicrob Chemother 53:853–859
Meyer E, Schwab F, Gastmeier P, Rueden H, Daschner FD (2006) Surveillance of antimicrobial use and antimicrobial resistance in German intensive care units (SARI): a summary of the data from 2001 through 2004. Infect 34:303–309
Mutnick AH, Rhomberg PR, Sader HS, Jones RN (2004) Antimicrobial usage and resistance trend relationship from MYSTIC programme in North America. J Antimicrob Chemother 53:290–296
Crowcroft NS, Ronveaux O, Monnet DL, Mertens R (1999) Methicillin-resistant Staphylococcus aureus and antimicrobial use in Belgian hospitals. Infect Control Hosp Epidemiol 20:31–36
Graffunder EM, Venezia RA (2002) Risk factors associated with nosocomial methicillin-resistant Staphylococcus aureus (MRSA) infection including previous use of antimicrobials. J Antimicrob Chemother 49:999–1005
Monnet DL (1998) Methicillin-resistant Staphylococcus aureus and its relationship to antimicrobial use: possible implications for control. Infect Control Hosp Epidemiol 19:552–559
Muller AA, Mauny F, Bertin M, Cornette C, Lopez-Lozano JM, Viel JF, Talon DR, Bertrand X (2003) Relationship between spread of methicillin-resistant Staphylococcus aureus and antimicrobial use in a French university hospital. Clin Infect Dis 36:971–978
Dahms RA, Johnson EM, Statz CL, Lee JT, Dunn DL, Beilman GJ (1998) Third-generation cephalosporins and vancomycin as risk factors for post operative vancomycin-resistant Enterococcus infection. Arch Surg 133:1343–1346
Harbarth H, Cosgrove S, Carmeli Y (2002) Effects of antibiotics on nosocomial epidemiology of vancomycin-resistant enterococci. Antimicrob Agents Chemother 46:1619–1628
Rice LB, Hutton-Thomas R, Lakticova V, Helfand MS, Donskey CJ (2004) β-Lactam antibiotics and gastrointestinal colonization with vancomycin-resistant enterococci. Clin Infect Dis 189:1113–1118
Venezia RA, Domaracki BE, Evans AM, Preston KE, Graffunder EM (2001) Selection of high-level oxacillin resistance in heteroresistant Staphylococcus aureus by fluoroquinolone exposure. J Antimicrob Chemother 48:375–381
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM (1988) CDC definitions for nosocomial infections, 1988. Am J Infect Control 16:128–40
Clinical and Laboratory Standards Institute (2009) Performance standards for antimicrobial susceptibility testing; Nineteenth informational supplement (M100-S19). CLSI, Wayne
Clinical and Laboratory Standards Institute (2006) Performance standards for antimicrobial disk susceptibility tests: approved standard. Document M2-A9, 9th edn. CLSI, Wayne
Liebowitz LD, Blunt MC (2008) Modification in prescribing practices for third-generation cephalosporins and ciprofloxacin is associated with a reduction in methicillin-resistant Staphylococcus aureus bacteraemia rate. J Hosp Infect 69:328–36
Conflict of interest statement
None declared.
Funding sources
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lai, C.C., Wang, C.Y., Chu, C.C. et al. Correlation between antimicrobial consumption and resistance among Staphylococcus aureus and enterococci causing healthcare-associated infections at a university hospital in Taiwan from 2000 to 2009. Eur J Clin Microbiol Infect Dis 30, 265–271 (2011). https://doi.org/10.1007/s10096-010-1081-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-010-1081-1