Abstract
In the last two decades, an increasing trend in the incidence of pneumococcal disease in Europe has been reported. We investigated the effect of the use of the heptavalent pneumococcal conjugate vaccine (PCV7) in an area of northern Spain, where all recorded cases of invasive pneumococcal diseases (IPD) were included (n = 450; 91 between 1996–2007 in children aged <5 years and 359 between 1998–2007 in adults aged >64 years). All isolates were serotyped. In children, the overall IPD incidence did not significantly decrease after the introduction, in late 2001, of PCV7. However, the incidence of PCV7 serotypes significantly decreased by 137.2% from 31.59 cases/100,000 population in 1996–2001 to 13.42 in 2002–2007 (95% confidence interval [CI] −27.2 to −342.4%), as did the overall rates of penicillin resistance (from 45.6 to 18.6%) and multiresistance (from 30.3 to 11%). In older adults, the overall IPD incidence showed a non-significant increase due to non-PCV7 serotypes, which seemed to continue a previous trend in our region.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pneumococcal diseases are the first cause of death attributable to a vaccine-preventable disease worldwide [1, 2]. At present, two types of pneumococcal vaccines are used, each with a different number of capsular serotypes: the 23-valent pneumococcal polysaccharide vaccine (PPV23) and the newer heptavalent pneumococcal conjugate vaccine (PCV7). PPV23 is poorly active and is not recommended for routine vaccination in young children [3, 4]. The PCV7 has been shown to confer protection and to decrease the incidence of invasive pneumococcal disease (IPD) in young children, due to the serotypes included in this vaccine (serotypes 4, 6B, 9V, 14, 18C, 19F and 23F), as well as to decrease the rates of antibiotic-resistant invasive pneumococcal infections [5, 6].
In Europe, the use of PCV7 has been infrequent, with most countries having introduced this vaccine in 2005 and 2006 [7]. Consequently, few studies on the effect of PCV7 have been performed. This vaccine was introduced for the vaccination of young children in Spain in late 2001. Although PCV7 has not been included in the Basque Health System vaccination calendar (it is not subsidised), estimates indicate that approximately 50% of children aged <2 years in our autonomous community (Basque Country, Northern Spain) have been vaccinated [8]. PPV23 was introduced in the vaccination calendar in our region for people over 64 years of age in June 2007.
The incidence of IPD in the previous 12 years (1996–2007) in children aged <5 years and in the last 10 years (1998–2007) in adults aged >64 years in a specific region of northern Spain was studied. This study was performed in a region that provided population-based data and where the main changes produced in the diagnostic procedures could be controlled.
The aim of this study was to gain a greater understanding of the benefits and limitations of PCV7 use in a region of Europe. The association between temporal trends in IPD and changes in the prevalence of Streptococcus pneumoniae serotypes and PCV7 use were analysed.
Materials and methods
Population data and study periods
This study was performed in a region that included the areas of San Sebastián, Tolosa and most of the villages belonging to the area of the Urola Coast, all of which are in the province of Gipuzkoa, Basque Country, northern Spain. All registered cases of IPD in people living in these areas were included in this study.
The study was performed in children aged <5 years and in adults aged >64 years. To calculate the incidence rates of IPD by age groups, official data from the population living in the study areas (Eustat, Basque Institute office; http://www.eustat.es) were used. Census data were available for 1996, 2001 and 2006, while values estimated from a standard curve determined by linear regression were used for the remaining years.
The study was divided into two distinct periods. In children, the study period was 12 years, divided into two 6-year periods; a pre-vaccination period from 1996 to 2001, before the introduction of PCV7, and a post-vaccination period, from 2002 to 2007. In adults, the study period was 10 years; the pre-vaccination period was from 1998 to 2001 and the post-vaccination period was the same as that in children. Data on IPD from 1996 and 1997 from adults were excluded from the analysis due to differences in the diagnostic methods used in 1996 and 1997 compared with those in the following years.
Blood culture practice
Hospital Donostia is a 1,100-bed hospital, including a maternity unit, and is the referral hospital for the entire province. The hospital has 76 paediatric (<14 years old) beds and attends an annual mean of approximately 29,500 paediatric emergencies and approximately 4,000 deliveries. The hospital belongs to the public health system, which attends more than 97% of paediatric hospitalisations in Gipuzkoa. Although non-apparent changes were produced in the demand for diagnostic procedures, to coarsely estimate possible changes, the annual number of blood cultures collected from children and adults at the hospital was measured. Specific ages were available from 79 and 81% of the paediatric and adult patients with blood cultures, respectively. The unknown ages of the remaining 21 and 19% patients with blood cultures were then extrapolated and distributed accordingly into each age group.
Definition of IPD case
During the study periods, all children aged <5 years or adults aged >64 years living in the study areas diagnosed with pneumonia, meningitis, peritonitis or arthritis with an S. pneumoniae isolate from a sterile site (blood, cerebrospinal fluid [CSF], pleural, joint or peritoneal effusion) were considered to be eligible for inclusion. Patients with a S. pneumoniae isolated exclusively from a blood culture collected at the paediatric emergency department without signs of invasive disease, hospital admission or antibiotic treatment were not included.
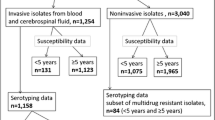
Isolates
S. pneumoniae isolates were identified to the species level by their colony morphology, optochin sensitivity and bile solubility tests. Isolates were serogrouped and serotyped by the Quellung reaction using antisera (Statens Serum Institut, Copenhagen, Denmark) and/or by a multiplex polymerase chain reaction (PCR) using previously described primers and conditions [9]. Isolates were grouped as PCV7 serotypes if they pertained to the serotypes included in PCV7 and as non-PCV7 serotypes if they were of any other serotype.
Pulsed-field gel electrophoresis (PFGE) and multilocus sequence typing (MLST) were performed on isolates of selected serotypes according to previously described protocols [10] in order to study their clonality.
Antimicrobial susceptibility
Antibiotic susceptibility was determined by the broth microdilution method and interpreted according to procedures and breakpoints reported by the Clinical and Laboratory Standards Institute [11]. Multiresistance was considered if an isolate showed resistance to penicillin (minimum inhibitory concentration [MIC] ≥0.12 μg/ml) and any two of the following antibiotics: cefotaxime (MIC ≥2 μg/ml), erythromycin (MIC ≥1 μg/ml), clindamycin (MIC ≥1 μg/ml), tetracycline (MIC ≥8 μg/ml), trimethoprim–sulfamethoxazole (MIC ≥4/76 μg/ml), chloramphenicol (MIC ≥8 μg/ml) and ciprofloxacin (MIC ≥4 μg/ml).
Statistical analysis
The chi-square test was used to compare qualitative variables with application of Yates’ or Fisher’s corrections (two-tailed) when required. Spearman’s rank correlation (r) was used to determine the strength of association or correlation between pairs of variables (IPD and diagnostic blood culture demand; IPD and population etc.) An r = 1 represents 100% correlation of ranking between two variables, an r = 0 represents no correlation and a negative correlation coefficient represents an inverse correlation. Statistical significance was determined with 95% confidence intervals (CI). Changes in incidence rates between the pre- and post-vaccination periods were assessed by calculating relative risks (RRs), reported as percentage changes in disease rates (percentage change in IPD = [1 − RR] × 100). A P-value of <0.05 was considered to be significant.
Results
A total of 450 IPD cases were included in this study (Tables 1 and 2), 91 for the period 1996–2007 in children aged <5 years [annual mean: 7.6 (95% CI: 6.0–9.2)] and 359 for the period 1998–2007 in adults aged >64 years [annual mean: 35.9 (95% CI: 31.7–40.1)].
Throughout the study period, the overall population of the region increased, especially the population of interest in this study. Based on the census for 1996, 2001 and 2006, the population aged <5 years grew from 13,622 to 17,128 and to 19,509 inhabitants, respectively, and that aged >64 years from 59,487 to 65,674 and to 70,684 inhabitants, respectively.
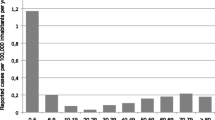
Invasive pneumococcal disease in children aged <5 years
During the 12 years of the study, S. pneumoniae caused 91 episodes of IPD in children <5 years, being isolated in blood on 79 occasions, in CSF in nine and one each in pleural fluid, peritoneal fluid (spontaneous peritonitis) and knee joint fluid. In children, pneumonia with bacteraemia was the most common manifestation of IPD (44/91, 48.4%), followed by bacteraemia without focus (33/91, 36.3%) and meningitis (11/91, 12.1%). No differences in the percentages of clinical presentations were found between both periods. Only one child died from meningitis caused by serotype 19A in the post-vaccination period. Of the 91 episodes, 46 episodes (50.5%) occurred in the pre-vaccination period (1996–2001; annual mean 7.7, 95% CI: 6.2–9.1) and the remaining 45 cases (49.5%) in the post-vaccination period (2002–2007; annual mean 7.5, 95% CI: 3.9–11.1). All 91 cases were serotyped. PCV7 serotypes caused 48.4% of IPD episodes, most of which occurred in the pre-vaccination period (29/44, 65.9%). Non-PCV7 serotypes were more frequent in the post-vaccination period (30/47; 63.8%).
Throughout the study period, the number of children <5 years of age living in the districts studied and the number of blood cultures performed increased (Table 1), with both increases showing a statistically significant correlation (r = 0.9161, 95% CI: 0.7120–0.9774, P < 0.0001). Between 1996 and 2007, no significant correlation was observed between the overall number of IPD episodes and the number of blood cultures drawn or the population size. No correlation was observed either with the number of IPD episodes caused by PCV7 or by non-PCV7 serotypes.
The annual incidence rates of IPD for the pre- and post-vaccination periods showed a non-significant decrease from 49.95 to 39.55 per 100,000 population (Table 3). When the two periods were compared, the decrease from 31.59 to 13.42 per 100,000 population in the annual incidence of IPD caused by PCV7 serotypes was statistically significant. In contrast, no statistically significant differences were observed in the incidence of IPD caused by non-PCV7 serotypes between the same two periods.
The most prevalent serotypes were the non-PCV7 serotypes 19A (n = 15) and 1 (n = 12) and the PCV7 serotypes 6B (n = 11) and 14 (n = 11). Serotypes 1 and 19A represented 29.7% of all episodes, while serotypes 6B and 14 represented an extra 24.2%. Except for serotype 1, which was isolated on three occasions in the pre-vaccination period and on nine in the post-vaccination period, serotypes 19A, 6B and 14 were isolated less frequently in the post-vaccination period. No association was observed between 19A isolates (12 different PFGE patterns were found), while 8 of the 12 isolates of serotype 1 had the same PFGE pattern and belonged to ST306.
Of the 45 children with IPD in the post-vaccination period, 18 had received at least one dose of PCV7 prior to infection. PCV7 serotypes infected 1/18 (5.6%) vaccinated and 14/27 (51.9%) non-vaccinated children (P = 0.0013). The episode due to a PCV7 serotype was an arthritis caused by serotype 19F in a 17-month boy who had received two doses of PCV7.
The other serotypes found in vaccinated children were serotype 1 (n = 7), 19A (n = 3), 7F (n = 2), 5 (n = 1), 10 (n = 1), 15 (n = 1), 22 (n = 1) and 24 (n = 1).
Penicillin resistance decreased during the post-vaccination period (Tables 1 and 3). Penicillin resistance (25/44, 56.8%) and multiresistance (15/44, 34.1%) were associated with PCV7 serotypes versus non-PCV7 serotypes (5/47, 10.6 and 4/47, 8.5%, respectively); P < 0.005 for both. Cefotaxime resistance (MIC ≥2 μg/ml) was only observed in PCV7 serotypes.
Invasive pneumococcal disease in adults aged >64 years
Overall, 359 episodes of IPD were detected between 1998 and 2007 in adults aged >64 years. Of these, 129 episodes occurred in the pre-vaccination period (1998–2001, annual mean 32.25, 95% CI: 28.27–36.23) and 230 in the post-vaccination period (2002–2007, annual mean 38.33, 95% CI: 31.64–45.03). All 359 isolates were serotyped; 121 (33.7%) were PCV7 serotypes and 238 (66.3%) were non-PCV7 serotypes. No statistically significant differences in the overall incidence of IPD, in the incidence due to PCV7 or in non-PCV7 serotypes were observed between pre- and post-vaccination periods (Table 3).
In adults, the increase in demand for blood cultures was correlated with the population increase (r = 0.7091, P = 0.027). No significant correlation was found between the increases in population and blood culture demand and the overall number of IPD cases or with the number of IPD cases due to PCV7 vaccine serotypes. However, the increase in the population or blood culture demand was significantly correlated with the increase in IPD cases due to non-PCV7 serotypes (r = 0.793, P = 0.009 for population size and r = 0.689, P = 0.031 for blood culture demand).
The most frequent serotypes and the number of episodes caused by each serotype in the pre- and post-vaccination periods were serotype 3 (51 cases, 24 and 27), serotype 14 (36 cases, 11 and 25), serotype 19A (30 cases, 5 and 25) and serotype 1 (21 cases, 3 and 18).
In adults, penicillin resistance was also associated with PCV7 serotypes (60/121, 49.6% versus 11/238, 4.6%; P < 0.0001), as well as with multiresistance (31/121, 25.6% versus 8/238, 3.4%; P < 0.0001).
Unlike the results in children <5 years of age, penicillin resistance did not statistically decrease in the post-vaccination period, although multiresistance did decrease (Table 3). Cefotaxime resistance (MIC ≥2 μg/ml) was only observed in PCV7 serotypes.
Prevalence of vaccine serotypes
The prevalence of PCV7 serotypes was 63% (29/46) for children <5 years and 39.5% (51/129) for adults >64 years of age in the pre-vaccination period, dropping to 33.3% (15/45) and 30.4% (70/230), respectively, in the post-vaccination period.
When the serotypes covered by Glaxo’s 10-valent conjugate investigational vaccine (PCV7 serotypes plus 1, 5 and 7F) (PCV10) and by Wyeth’s 13-valent conjugate investigational vaccine (PCV7 serotypes plus 1, 3, 5, 6A, 7F and 19A) (PCV13) were considered, the estimations of coverage in the period 2002–2007 would have been 31/45 (68.9%) and 39/45 (86.7%) for children <5 years and 106/230 (46.1%) and 163/230 (70.9%) for adults >64 years of age, respectively. The serotype 11 and 14 of the 18 isolates causing IPD in children who had received at least one PCV7 dose before infection were represented in the PCV10 and PCV13 vaccines, respectively.
Discussion
After 2001, the incidence of IPD caused by PCV7 serotypes in children <5 years of age sharply decreased, as did the percentages of penicillin resistance and multiresistance in the strains causing these IPD cases. Nevertheless, the overall incidence of IPD in children aged <5 years showed only a non-significant reduction of −10.4 (95% CI: −26.57–5.76). According to the published data, in the last decade, the incidence of pneumococcal disease in European countries has increased [12–17]. If these reports are an accurate reflection of reality, whether due to a true increase in disease occurrence or as a result of an improvement in surveillance methodology in the last few years [16], the effect of PCV7 may not have been as obvious as in other places where these circumstances have not occurred. In the USA, the introduction of the PCV7 vaccine has been accompanied by a striking decrease in the incidence of IPD [5, 18]. In contrast, most of the few studies performed in Europe have found no significant differences between the pre- and post-vaccination periods. In Portugal [15], France [19] and in several studies from Spain, the changes in the incidence of IPD were not significant [20–22] or were very slight [17]; a recent study even showed increases in the incidence of IPD after the introduction of PCV7 [23]. In the present study, all isolates were available for serotyping, and despite the yearly population increase, a high IPD incidence rate was found in comparison with the rates described in similar areas [7, 20, 23].
The reported incidence of IPD and its interpretation may have been influenced by methodological issues. Changes in the size of the population studied, as well as modifications in medical practice, especially in the practice of drawing blood cultures, are highly important [24].
The overall population in our region rose yearly and this increase was more noticeable in the population of interest (small children and older adults), the age groups most susceptible to pneumococcal infection.
The non-significant increase in the incidence of IPD in children caused by non-PCV7 serotypes found in this study could not be explained by more frequent blood culturing, since, throughout the study period, the number of children living in the districts studied and the number of blood cultures performed increased in a similar fashion. The trend of non-PCV7 IPD in the last few years in our region will continue or even increase as the spread of specific epidemic clones not covered by PCV7 increases.
The epidemiology of pneumococcal infection is complex, and the reason why a certain clone disappears from a region or spreads epidemically is not well known. The non-significant increase in the rate of IPD in children caused by non-PCV7 between 1996–2001 and 2002–2007 was partly due to serotypes 1 and 19A. As in this study, the rest of Europe and North America, serotype 1 has been associated with ST306 and its related sequence types [22, 25–28] and can, therefore, be considered as a clone whose current behaviour is nearly pandemic. Serotype 19A isolates in this study belonged to 12 different clones (different PFGE patterns), indicating polyclonal spread of this serotype. Infections caused by serotypes 1 and 19A were increasing in Europe before the introduction of PCV7 [16, 27–30].
Apart from preventing IPD, PCV7 affects both pneumococcal carriage and the transmission of PCV7 serotypes [31], and some authors have indicated the beneficial effect that the use of PCV7 in children may have in adults [31, 32]. The higher the vaccine coverage and the longer the vaccination programme has been implemented, the higher the herd effect or protection among the non-vaccinated population. A vaccine coverage of about 50% in the population aged <5 years would be unlikely to significantly change the trend of pneumococcal infection in older people in such a short space of time, prompting us to speculate that our findings in older people, including the decrease in multiresistant isolates, was mainly a consequence of the natural evolution of pneumococcal infection in our region.
In conclusion, our findings in older adults seem to reproduce the overall trends of pneumococcal infection in the last few years in our region. In contrast, in children, despite modest PCV7 coverage, both antimicrobial resistance and the incidence of IPD caused by vaccine serotypes decreased. The beneficial effect of PCV7 was probably greater than that which would have been estimated by comparing the overall IPD incidences between pre- and post-vaccination periods and could be increased by using new PCVs that cover more serotypes when they become available.
References
Centers for Disease Control and Prevention (CDC) (2006) Vaccine preventable deaths and the Global Immunization Vision and Strategy, 2006–2015. MMWR Morb Mortal Wkly Rep 55:511–515
World Health Organization (WHO) (2004) 2004 global immunization data. Available online at: http://www.who.int/immunization_monitoring/data/GlobalImmunizationData.pdf
Jackson LA, Neuzil KM, Yu O et al (2003) Effectiveness of pneumococcal polysaccharide vaccine in older adults. N Engl J Med 348:1747–1755. doi:10.1056/NEJMoa022678
Centers for Disease Control and Prevention (CDC) (1997) Prevention of pneumococcal disease: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep 46:1–24
Whitney CG, Farley MM, Hadler J et al (2003) Decline in invasive pneumococcal disease after the introduction of protein–polysaccharide conjugate vaccine. N Engl J Med 348:1737–1746. doi:10.1056/NEJMoa022823
Kyaw MH, Lynfield R, Schaffner W et al (2006) Effect of introduction of the pneumococcal conjugate vaccine on drug-resistant Streptococcus pneumoniae. N Engl J Med 354:1455–1463. doi:10.1056/NEJMoa051642
Lopalco PL; Editorial team (2006) Use of 7-valent pneumococcal conjugate vaccine in EU. Euro Surveill 11:E061207.3
Mintegi S, Benito J, González M et al (2006) Impact of the pneumococcal conjugate vaccine in the management of highly febrile children aged 6 to 24 months in an emergency department. Pediatr Emerg Care 22:566–569. doi:10.1097/01.pec.0000230550.79046.68
Brito DA, Ramirez M, de Lencastre H (2003) Serotyping Streptococcus pneumoniae by multiplex PCR. J Clin Microbiol 41:2378–2384. doi:10.1128/JCM.41.6.2378-2384.2003
Pérez-Trallero E, Marimón JM, Gonzalez A et al (2003) Spain14-5 international multiresistant Streptococcus pneumoniae clone resistant to fluoroquinolones and other families of antibiotics. J Antimicrob Chemother 51:715–719. doi:10.1093/jac/dkg106
Clinical and Laboratory Standards Institute (CLSI) (2007) Performance standards for antimicrobial susceptibility testing: 17th informational supplement. M100-S17. CLSI, Wayne, PA
Harboe ZB, Valentiner-Branth P, Benfield TL et al (2008) Estimated effect of pneumococcal conjugate vaccination on invasive pneumococcal disease and associated mortality, Denmark 2000–2005. Vaccine 26:3765–3771. doi:10.1016/j.vaccine.2008.04.040
Johnson AP, Waight P, Andrews N et al (2007) Morbidity and mortality of pneumococcal meningitis and serotypes of causative strains prior to introduction of the 7-valent conjugant pneumococcal vaccine in England. J Infect 55:394–399. doi:10.1016/j.jinf.2007.07.009
Rückinger S, von Kries R, Reinert RR et al (2008) Childhood invasive pneumococcal disease in Germany between 1997 and 2003: Variability in incidence and serotype distribution in absence of general pneumococcal conjugate vaccination. Vaccine 26:3984–3986. doi:10.1016/j.vaccine.2008.04.031
Dias R, Caniça M (2007) Invasive pneumococcal disease in Portugal prior to and after the introduction of pneumococcal heptavalent conjugate vaccine. FEMS Immunol Med Microbiol 51:35–42. doi:10.1111/j.1574-695X.2007.00283.x
Ihekweazu CA, Dance DA, Pebody R et al (2008) Trends in incidence of pneumococcal disease before introduction of conjugate vaccine: South West England, 1996–2005. Epidemiol Infect 136:1096–1102. doi:10.1017/S0950268807009715
Aristegui J, Bernaola E, Pocheville I et al (2007) Reduction in pediatric invasive pneumococcal disease in the Basque Country and Navarre, Spain, after introduction of the heptavalent pneumococcal conjugate vaccine. Eur J Clin Microbiol Infect Dis 26:303–310. doi:10.1007/s10096-007-0294-4
Kaplan SL, Mason EO Jr, Wald ER et al (2004) Decrease of invasive pneumococcal infections in children among 8 children’s hospitals in the United States after the introduction of the 7-valent pneumococcal conjugate vaccine. Pediatrics 113:443–449. doi:10.1542/peds.113.3.443
Bingen E, Levy C, Varon E et al (2008) Pneumococcal meningitis in the era of pneumococcal conjugate vaccine implementation. Eur J Clin Microbiol Infect Dis 27:191–199. doi:10.1007/s10096-007-0417-y
Barricarte A, Castilla J, Gil-Setas A et al (2007) Effectiveness of the 7-valent pneumococcal conjugate vaccine: a population-based case-control study. Clin Infect Dis 44:1436–1441. doi:10.1086/516779
Calbo E, Díaz A, Cañadell E et al (2006) Invasive pneumococcal disease among children in a health district of Barcelona: early impact of pneumococcal conjugate vaccine. Clin Microbiol Infect 12:867–872. doi:10.1111/j.1469-0691.2006.1502_1.x
Obando I, Arroyo LA, Sánchez-Tatay D et al (2007) Molecular epidemiology of paediatric invasive pneumococcal disease in southern Spain after the introduction of heptavalent pneumococcal conjugate vaccine. Clin Microbiol Infect 13:347–348. doi:10.1111/j.1469-0691.2006.01646.x
Muñoz-Almagro C, Jordan I, Gene A et al (2008) Emergence of invasive pneumococcal disease caused by nonvaccine serotypes in the era of 7-valent conjugate vaccine. Clin Infect Dis 46:174–182. doi:10.1086/524660
Pérez A, Herranz M, Segura M et al (2008) Epidemiologic impact of blood culture practices and antibiotic consumption on pneumococcal bacteraemia in children. Eur J Clin Microbiol Infect Dis 27:717–724. doi:10.1007/s10096-008-0498-2
Hausdorff WP, Feikin DR, Klugman KP (2005) Epidemiological differences among pneumococcal serotypes. Lancet Infect Dis 5:83–93
Brueggemann AB, Spratt BG (2003) Geographic distribution and clonal diversity of Streptococcus pneumoniae serotype 1 isolates. J Clin Microbiol 41:4966–4970. doi:10.1128/JCM.41.11.4966-4970.2003
McChlery SM, Scott KJ, Clarke SC (2005) Clonal analysis of invasive pneumococcal isolates in Scotland and coverage of serotypes by the licensed conjugate polysaccharide pneumococcal vaccine: possible implications for UK vaccine policy. Eur J Clin Microbiol Infect Dis 24:262–267. doi:10.1007/s10096-005-1313-y
Serrano I, Melo-Cristino J, Carriço JA et al (2005) Characterization of the genetic lineages responsible for pneumococcal invasive disease in Portugal. J Clin Microbiol 43:1706–1715. doi:10.1128/JCM.43.4.1706-1715.2005
Kirkham LA, Jefferies JM, Kerr AR et al (2006) Identification of invasive serotype 1 pneumococcal isolates that express nonhemolytic pneumolysin. J Clin Microbiol 44:151–159. doi:10.1128/JCM.44.1.151-159.2006
Flamaing J, Verhaegen J, Vandeven J et al (2008) Pneumococcal bacteraemia in Belgium (1994–2004): the pre-conjugate vaccine era. J Antimicrob Chemother 61:143–149. doi:10.1093/jac/dkm435
Hammitt LL, Bruden DL, Butler JC et al (2006) Indirect effect of conjugate vaccine on adult carriage of Streptococcus pneumoniae: an explanation of trends in invasive pneumococcal disease. J Infect Dis 193:1487–1494. doi:10.1086/503805
Lexau CA, Lynfield R, Danila R et al (2005) Changing epidemiology of invasive pneumococcal disease among older adults in the era of pediatric pneumococcal conjugate vaccine. JAMA 294:2043–2051. doi:10.1001/jama.294.16.2043
Financial support
This work was supported, in part, by the CIBERES and by a grant from the University of the Basque Country/Euskal Herriko Unibertsitatea (Subvención General a Grupos de Investigación).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pérez-Trallero, E., Marimon, J.M., Ercibengoa, M. et al. Invasive Streptococcus pneumoniae infections in children and older adults in the north of Spain before and after the introduction of the heptavalent pneumococcal conjugate vaccine. Eur J Clin Microbiol Infect Dis 28, 731–738 (2009). https://doi.org/10.1007/s10096-008-0693-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-008-0693-1