Abstract
Can Escherichia coli be used as an indicator organism for transmission events in hospitals? Perineal and pharyngeal swabs were obtained from patients admitted to a medical or surgical intensive care unit within 24 h of admission and then twice per week. Escherichia coli isolates were typed by random amplification of polymorphic DNA (RAPD) and amplified fragment length polymorphism (AFLP) typing. Based on the typing results, transmission rates for RAPD and AFLP typing were 8.5 and 6.6 per 100 patient-days. Requiring in addition to similarity in genotype parity in time and place for a transmission event, the incidence dropped to 3.8 (RAPD) and 1.7 (AFLP) per 100 patient-days. The two typing methods not only differed with respect to numbers of transmissions identified, but also to individuals involved in transmissions. This study identified a number of problems regarding the use of Escherichia coli as indicator organism for transmission events. The use of Escherichia coli for this purpose cannot be recommended at the moment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infection control measures such as those formulated in the Standard Precautions are aimed at preventing transmission of micro-organisms and by doing so exogenous healthcare-associated infections (HAI) [1]. To assess the validity of this type of precaution the number of HAI is the ultimate endpoint. This measure has several drawbacks: discrimination between endogenous and exogenous infections is often difficult, and on standard wards the number of HAI is rather low, making comparisons statistically cumbersome. The alternative should be to measure transmission events. By carrying out surveillance cultures of all patients admitted to a ward and by typing the bacteria isolated from these cultures, theoretically it must be possible to assess the number of transmissions that have occurred. This approach will only be feasible if one or two frequently occurring micro-organisms, e.g. Escherichia coli (E. coli) or Enterococcus faecalis, can be used as indicator organisms for transmission.
As a first step in the development of this approach of measuring transmission events for the evaluation of hospital hygiene, we performed a study on two intensive care units. The questions were:
-
1.
Is it possible to detect transmission of E. coli in a reliable way so that the organism can be used as an indicator for transmission?
-
2.
What is the frequency of transmission of E. coli in an intensive care unit (ICU) under endemic conditions?
To answer these questions, we sampled patients on two ICUs prospectively and typed the cultured E. coli isolates from the patients by genomic fingerprinting. In addition, the type diversity of E. coli strains from different populations outside the ICUs was investigated to provide a framework for interpretation of the ICU results.
Materials and methods
ICU patients and samples
All patients admitted to the medical or surgical ICU of the Leiden University Medical Centre (LUMC) between 30 October and 7 December 2000 were prospectively included in the study. Within 24 h of admission and from then on each Monday and Thursday as long as the patient stayed in the ICU, perineal and pharyngeal swabs were taken. Clinical specimens were taken when indicated by the physician in charge.
Swabs were inoculated onto blood agar plates (CM271; Oxoid, Haarlem, The Netherlands) and CLED plates (Cystein Lactose Electrolyte Deficiency plates, CM225; Oxoid, Haarlem, The Netherlands). After 24 and 48 h of incubation at 35°C under aerobic conditions, the plates were screened for the presence of Gram-negative bacteria on the basis of colony morphology. Species identification and sensitivity testing were performed by the use of the VITEK2 system (Biomerieux, ‘s- Hertogenbosch, The Netherlands). E. coli isolates with different colony morphology or sensitivity pattern from one patient were included as separate isolates for typing.
Samples from outside the ICUs
To investigate the diversity of E. coli outside the ICUs under study, isolates were collected from three groups of patients supposed to be unrelated to each other. Group 1 were patients visiting outpatient departments of the LUMC, a sample of whose faeces was sent to the microbiological laboratory for culture, or patients from the general population whose general practitioner had ordered a faeces culture. Group 2 were patients admitted to different departments of the LUMC, a sample of whose faeces was sent to the microbiological laboratory. Group 3 were patients admitted to the LUMC in whom E. coli had been found in clinical samples. Isolates were collected between February and July 2002. From Group 1 and 2 patients faeces samples were cultured on CLED and colonies resembling E. coli were presumptively identified as E. coli by use of the PGUA/indol test (Rosco, Taastrup, Denmark). Final identification was obtained with the VITEK2 system (Biomerieux).
Random amplification of polymorphic DNA typing
Standardized PCR amplification with primers DAF4 and M13-core and Ready-To-Go™ random amplification of polymorphic DNA (RAPD) Analysis beads (GE Healthcare, Roosendaal, Netherlands), and agarose electrophoresis were performed as described [2]. Digitized profiles generated with both primers were normalized, combined into a composite dataset from which similarities were calculated and cluster analysis was performed using Bionumerics™ software, version 3.5 (Applied Maths, Sint-Martens-Latem, Belgium). Pearson product moment correlation coefficient was used as a dissimilarity measure, and the unweighted pair group average linkage method (UPGMA) for clustering. Zones used for clustering were 40–86% for DAF4 and 36–66% for M13. Optimization and position tolerance for both primers were 0.25% and 1% respectively. Isolates linked at ≥90% were considered the same type, as deduced from clustering at this level of multiple isolates of the same patient (apart from clearly different isolates representing another strain), and repeated analysis of one control strain. Profiles clustering at ≥90% visually had a maximum of one band difference.
Amplified fragment length polymorphism typing
Selective amplification of genomic restriction fragments using AFLP was performed as described previously [3]. Briefly, purified DNA was digested using EcoRI and MseI, and amplification was carried out with a Cy5-labelled EcoRI + A primer and an MseI + C primer (A and C, selective bases). The ALF express II DNA analysis system (Amersham Biosciences, Roosendaal, The Netherlands) was used for fragment separation. Fragments of 50 to 500 bp were investigated by cluster analysis using the Bionumerics software package with the Pearson product moment correlation coefficient as a similarity measure and UPGMA for grouping. Isolates linked at 90% or above were considered the same type.
Diversity calculation
Simpson’s diversity index (DI) was calculated for the ICU and the three groups of non-ICU patients according to the formula:
where ni was the number of isolates assigned to the RAPD types and N was the total number of isolates studied in the actual population of strains [4]. Di measures the distribution of isolates between RAPD types, and should be close to 1.00 for random bacterial populations if a highly discriminatory typing method is used.
Results and discussion
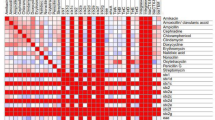
During the study period 136 patients were admitted to the intensive care units, 106 of whom were sampled. The number of patient days studied was 424. In total, 156 isolates of E. coli were found in 72 patients: 138 isolates from perineum, 16 from pharynx and 2 from clinical specimens. A total of 110 isolates remained after exclusion of multiple isolates with the same pattern in each patient as assessed by careful visual and computer-assisted analysis of RAPD profiles. By cluster analysis of the RAPD profiles of these isolates 17 clusters and 57 single isolates were distinguished at a cutting level of 90%, thus representing a total of 74 genotypes (Table 1). A subset of RAPD profiles is shown in Fig. 1a. To validate the results of the RAPD typing the 110 isolates were also typed by AFLP analysis. An example of a subset of profiles is given in Fig. 1b. A total of 15 clusters and 64 single profiles were distinguished (Table 1). Depending on which typing method was used transmission rates of 8.5 or 6.6 per 100 patient-days were suggested. When parity in time and place was taken as an additional criterion for transmission, the rates were 3.8 or 1.7 per 100 patient-days. The results of the two typing methods overlapped for 6 clusters (5 of 2 patients and 1 of 4 patients). Requiring correspondence in time and place, 5 transmissions were confirmed by both methods.
Example of a random amplification of polymorphic DNA (RAPD) and b amplified fragment length polymorphism (AFLP) typing. Thirty-two strains that occurred in at least 2 patients based on AFLP (16 couples) were selected and compared with RAPD typing. Eight AFLP couples were identified as couples by RAPD (linked and numbered). The other eight AFLP couples were not identified as such by RAPD. Vertical dotted lines mark the strain delineation level (90%). Similarities among RAPD profiles are based on combined M13 and DAF profiles
Regarding the use of E. coli as an indicator organism for transmission events in hospital wards, our study identified a number of problems. Only two-thirds of the ICU patients included in the study had cultures yielding E. coli. Much less than the expected 100% carriage rate. Usage of antibiotics while the cultures were taken is a likely explanation for this observation. It is a drawback of the use of E. coli as an indicator for transmission events because information about a substantial part of the population is lacking.
The two typing methods gave different results with respect to numbers of transmissions and individuals involved in transmission events. The poor correlation between the two methods raises severe doubts about the validity of the conclusions based on one of the methods. The discrepancy of the methods may be explained by the fact that RAPD is less robust than AFLP, despite the fact that the conditions and reagents of RAPD were rigorously standardized. Another source of bias may be that the heavy bands in RAPD outweigh the minor bands during computer-assisted analysis. For these reasons we have some preference for accepting the AFLP results as the most definitive.
Assuming that under endemic conditions transmission of E. coli occurs primarily from patient to patient without involvement of the environment or colonized personnel as long-term sources, approximately the same transmission rates are expected whether these rates are based on typing results alone or taking into account parity in time and place. The results of this study do not confirm this hypothesis.
We applied a strict norm for parity in time and place: patients should have been present in the same ward at the same moment. Allowance of a window period has been suggested to correct for a possible short-term persistence of bacteria in wards [5]. Allowing a window period of ≤3 days, ≤6 days, ≤9 days or an unlimited window results in 19, 21, 22, or 27 transmission events for RAPD, and 10, 14, 15, or 20 transmission events for AFLP, according to our data. A window period may be justified for micro-organisms known to be able to survive for some time in the environment. However, E. coli generally survives for only hours; therefore, in our opinion, allowing a window period for this organism leads to overestimation of transmission events.
Our finding that according to RAPD or AFLP typing identical strains often occur in patients who have not been admitted at the same time and to the same ward might be explained by the occurrence of a limited number of clones of E. coli in the population. To check this hypothesis the diversity index was calculated for three collections of E. coli from unrelated patients. The diversity index for RAPD profiles distinguished at 90% ranged from 0.9267 to 0.9873, and for AFLP profiles from 0.9800 to 0.9967. The lowest diversity was observed in isolates from sample Group 3, cultured from clinical specimens of non-ICU patients taken for clinical reasons. The diversity index calculated for clustering levels at 80% ranged from 0.9700 to 0.8433. The diversities at 80% were considerably lower than at 90%, emphasizing the occurrence of groups of highly similar but not identical isolates. Like at the 90% delineation level, the lowest diversity was found in sample Group 3, whereas the highest values were found in samples from Group 1, the outpatients. The high diversity index at the 90% clustering level that we calculated in the ICU patients and other groups of patients does not support the hypothesis that there is a limited number of clones of E. coli.
The question whether we have to reject the hypothesis that under endemic conditions environmental sources and possibly colonized personnel do not play a role in transmission remains unanswered.
A possible explanation, which we cannot completely exclude, is sampling error. By the swab method used we may not always have been able to pick up bacteria carried by the patient, and we missed 20 (15%) of the patients who had been admitted during the investigation period. When sample error is indeed the explanation for our results then this is a serious drawback for the approach of measuring transmission events as a measure of hospital hygiene. It will not be easy to overcome the problem of sampling error. In a further experiment, we compared perineal swabs and rectal swabs with regard to the yield of Gram-negative bacteria and did not find better results (unpublished observation).
In a recent study, Eckmanns et al. [6] found no or poor correlation between incidence rates of nosocomial infections, compliance with hand hygiene procedures and hand rub consumption, and transmission episodes of nosocomial pathogens as the “gold standard” for infection control. The results of our study question the use of transmission events identified by the typing of isolates as the gold standard for the quality of hospital hygiene and offer an alternative explanation for the poor correlation.
Our results also questions studies that tried to determine the proportion of exogenous versus endogenous nosocomial infections in intensive care patients by identifying transmission events by the typing of clinical isolates [7, 8]. In this way 13–35% of nosocomial infections are marked as exogenous. In the light of our data, there is doubt as to whether the transmission events identified in these studies, which mostly used one typing method for specific micro-organisms, are truly transmission events.
In conclusion, we feel that because too many questions about the use of E. coli as an indicator organism for transmission events in hospitals are unanswered, it cannot be used for this purpose at the moment. Likely, E. coli is not unique in this respect and, therefore, data on transmission events based on the typing of any micro-organism should be interpreted with caution.
References
Garner JS, The Hospital Infection Control Practices Advisory Committee (1996) Guidelines for isolation precautions in hospitals. I. Evolution of isolation practices. II. Recommendations for isolation precautions in hospitals. Am J Infect Control 24:24–52
Vogel L, van Oorschot E, Maas HME, Minderhoud B, Dijkshoorn L (2000) Epidemiologic typing of Escherichia coli using RAPD analysis, ribotyping and serotyping. Clin Microbiol Infect 6:82–87
Nemec A, De Baere T, Tjernberg I, Vaneechoutte M, van der Reijden TJ, Dijkshoorn L (2001) Acinetobacter ursingii sp. nov. and Acinetobacter schindleri sp. nov., isolated from human clinical specimens. Int J Syst Evol Microbiol 51:1891–1899
Hunter PR, Gaston MA (1988) Numerical index of the discriminatory ability of typing systems: an application of Simpson’s index of diversity. J Clin Microbiol 26:2465–2466
Grundmann H, Bärwolf S, Tami A et al (2005) How many infections are caused by patient-to-patient transmission in intensive care units? Crit Care Med 33:946–951
Eckmanns T, Schwab F, Bessert J et al (2006) Hand rub consumption and hand hygiene compliance are not indicators of pathogen transmission in intensive care units. J Hosp Infect 63:406–411
Chetchotisakd P, Phelps CL, Hartstein AI (1994) Assessment of bacterial cross-transmission as a cause of infections in patients in intensive care units. Clin Infect Dis 18:929–937
Weist K, Pollege K, Schulz I, Rüden H, Gastmeier P (2002) How many nosocomial infections are associated with cross-transmission? A prospective cohort study in a surgical intensive care unit. Infect Control Hosp Epidemiol 23:127–132
Acknowledgement
We thank K. van der Kouwe, P.J.C. van den Brink and L. Smit for their excellent technical assistance.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
van den Broek, P.J., Bernards, A.T., van der Reijden, T.J.K. et al. Can Escherichia coli be used as an indicator organism for transmission events in hospitals?. Eur J Clin Microbiol Infect Dis 28, 169–173 (2009). https://doi.org/10.1007/s10096-008-0597-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-008-0597-0