Abstract
Four commercially available kits from (1) Focus Diagnostics, (2) SERION, (3) Zeus and (4) Vircell for detection of antibodies to Legionella pneumophila were evaluated with panels of sera from patients with proven Legionella infection (n = 81) and/or other bacterial infections (n = 75). An in-house indirect Legionella immunofluorescence antibody test (IF test) was used as reference. All sera from the laboratory-proven Legionella pneumophila cases [culture, urinary antigen test and/or polymerase chain reaction] of Legionella infection were found to be positive by the in-house IF test. The relative sensitivity for Focus Diagnostics, SERION, Zeus and Vircell kits was 81.5, 76.5, 68.8 and 62.5%, respectively, and the false-positive rate was 16.0, 5.6, 29.0 and 2.7%, respectively. The in-house IF test had a false-positive rate of 4.0%. It was found that none of the four commercial kits were as sensitive and specific as the in-house IF test.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Legionella (L.) pneumophila is responsible for at least two diseases in humans: Legionnaires’ disease, which is a severe form of pneumonia clinically indistinguishable from other types of bacterial pneumonia, and Pontiac fever, which is a flu-like illness. The common term for these diseases is legionellosis. L. pneumophila lives in freshwater and moist environments and multiplies especially at temperatures between 30 and 45°C [1]. Inhalation or aspiration of contaminated water can cause legionellosis.
The laboratory diagnosis of Legionnaires’ disease has traditionally been based on detection of antibodies and on isolation of the bacteria by culture. However, antibodies are generally not detected in the acute phase of the disease and culture is insensitive and time-consuming. An early diagnosis can be achieved by detection of L. pneumophila antigen in urine [2] or by detection of DNA from the organism by polymerase chain reaction (PCR) on lower respiratory samples [3]. However, kits for detection of urinary antigen have only reliable sensitivity for L. pneumophila serogroup (sg.) 1 [2] and not the other serogroups, which may also cause severe illness. Moreover, PCR is generally not used as a routine analysis, and it is to some degree hampered by the fact that pneumonia caused by L. pneumophila often is unproductive (dry cough) especially in the acute phase and in milder cases. Diagnosis of Pontiac fever is generally dependent on serology. Due to these circumstances, serology still remains an important tool in the diagnosis of legionellosis as well as for epidemiological and outbreak studies. Although serology rarely is helpful in the acute phase of the disease, it can be used to confirm a presumptive diagnosis of legionellosis by PCR or other non-confirmatory methods.
It is important to use specific, sensitive and validated methods for a reliable diagnosis. In this study, we compare an in-house reference method (IF test) with four commercially available kits for detection of antibodies to L. pneumophila: (1) Focus Diagnostics IFA kit for Legionella pneumophila sg. 1, 2, 3, 4, 5, 6 and 8 total immunoglobulin (Ig) (IgG/IgM/IgA), (2) SERION enzyme-linked immunosorbent assay (ELISA) classic Legionella pneumophila sg. 1-7 IgM kit and sg. 1-7 IgG kit, (3) Zeus Scientific, Inc. Legionella pneumophila sg. 1-6 ELISA IgG/IgM/IgA test system kit and (4) Vircell Legionella pneumophila sg. 1-6 ELISA IgG+IgM kit. It was decided to use seropositive sera in the study to be sure that the patients were able to produce antibodies, because up to 25% of patients with culture-verified legionellosis do not develop a significant antibody level [4], and to be sure that the serum was collected at a time when the patient had seroconverted. By testing the same panels of sera in all five assays, the performance of the methods was determined with respect to sensitivity and specificity (false-positive rate) relative to an in-house IF test. The kits have all previously been validated in different combinations but not all five at the same time [5–7].
Materials and methods
Sera
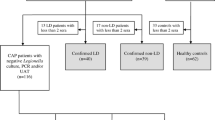
Sera used for sensitivity test
Eighty-one IF test-positive sera from 65 patients with L. pneumophila infection confirmed by one or more of the following methods; culture by standard method, Legionella urine antigen EIA (Biotest AG, Dreieich, Germany) and/or PCR by an in-house method [8]. All the sera were sent to Statens Serum Institut, Denmark for serodiagnosis. Of the 65 patients, 51 cases had only one serum sample analysed, 13 cases had two serum samples analysed, and 1 case had four serum samples analysed. Of the 65 cases, 33 were confirmed by culture either alone or combined with either Legionella urine antigen enzyme immunosorbent assay (EIA) or PCR or both methods, 27 cases were confirmed by Legionella urine antigen EIA either alone or combined with PCR and 5 cases were only positive by PCR.
The cases confirmed by culture could be grouped according to the L. pneumophila serogroup isolated from the patient: 25 were sg. 1 cases, 5 were sg. 3 cases, 1 was a sg. 5 case and 2 were sg. 6 cases. Most of the 27 cases confirmed by Legionella urine antigen EIA were probably sg. 1 cases. For the five PCR-positive cases, the causative serogroups are unknown.
Sera used for specificity test and cross-reactions
Seventy-five sera, which had been tested positive for antibodies against bacteria other than L. pneumophila, were used (10 sera of each positive for the following bacteria: Campylobacter jejuni/coli, Helicobacter pylori, Salmonella typhimurium/enteritidis, Proteus spp., Mycoplasma pneumoniae, Chlamydia group antigen, Coxiella burnetii and 5 sera positive for Pseudomonas aeruginosa). The Pseudomonas aeruginosa sera were supplied by Rigshospitalet, Copenhagen, Denmark, and were control sera from cystic fibrosis patients without pneumonia. All the other sera were sent to Statens Serum Institut, Denmark for serodiagnosis. Sera with antibodies to Campylobacter jejuni/coli, Proteus spp., Pseudomonas aeruginosa and Coxiella burnetii were chosen as these have previously been reported to be able to cross-react with Legionella [9–11]. Sera with antibodies to Mycoplasma pneumoniae (all cases confirmed as Mycoplasma pneumoniae infection by PCR) and Chlamydia group antigen (three cases confirmed as Chlamydia pneumoniae infection by PCR) were selected because these bacteria can give rise to respiratory symptoms similar to legionellosis [1, 12]. Helicobacter pylori and Salmonella typhimurium/enteritidis were chosen as representatives for antibodies to other gram-negative bacteria [13]. The sera used were all positive by validated serological tests and were a mixture of high and medium high results. None of the patients, from whom the sera were collected, have been notified as cases of Legionnaires’ disease within the last 15 years, so recent Legionnaires’ disease in the patients is very unlikely; a previous Legionella infection can however (symptomatic or non-symptomatic) of course not be ruled out.
Legionella pneumophila antibody detection kits
The following four commercial kits were used: Focus Diagnostics IFA kit for Legionella pneumophila sg. 1 (single antigen) and 2-6+8 (pool) IgG/IgM/IgA (Focus Diagnostics, Inc., Cypress, CA, USA), SERION ELISA classic Legionella pneumophila 1-7 IgM kit and 1-7 IgG kit (Serion Immundiagnostica GmbH, Würzburg, Germany), Zeus Scientific, Inc. Legionella pneumophila sg. 1-6 ELISA IgG/IgM/IgA test system kit (Zeus Scientific, Inc., Raritan, NJ, USA) and Vircell Legionella pneumophila sg. 1-6 ELISA IgG+IgM kit (Vircell S.L., Santa Fe, Spain).
All tests were performed according to the manufacturer’s instructions. The results for SERION ELISA IgG and IgM kits were combined; if a serum sample was positive in one of the kits the sample was considered positive. This was done in order to be able to compare this test with the results from the other kits which all detected total immunoglobulin (IgG, IgM and IgA).
In-house indirect Legionella immunofluorescence antibody test (IF test) [14, 15]
Serial dilutions of blood samples were analysed for antibodies against L. pneumophila by indirect immunofluorescence antibody test with plate-cultured and heat-inactivated L. pneumophila sg. 1 to 6 as single antigens. Antibodies to L. pneumophila were detected with a fluorescein isothiocyanate (FITC)-conjugated rabbit anti-human total immunoglobulin (IgM, IgA and IgG). The assay is essentially the same as the well-characterised assay reported by Wilkinson et al. [15], which follows the guidelines from the Centers for Disease Control and Prevention (CDC). An Escherichia coli blocking fluid [14] was used to block cross-reacting antibodies to other gram-negative bacteria. Titres of ≥1:256 were considered positive.
Results and discussion
Four commercially available kits were compared with an in-house IF test. The results which were found equivocal were repeated, and for those still equivocal the results were excluded from the calculations, since according to the manufacturers a new sample should be requested, if a sample repeatedly is equivocal.
The results are presented in Tables 1 and 2. The Focus Diagnostics, SERION ELISA classic, Zeus Scientific, Inc. ELISA and Vircell kits were all relatively sensitive (81.5, 76.5, 68.8 and 62.5%). But both Focus Diagnostics and Zeus Scientific, Inc. ELISA kits had high false-positive rates of 16 and 29%, respectively (Table 1), which are far too high to be acceptable in a routine laboratory. The combined SERION ELISA classic kits and the Vircell both showed very low false-positive rates (5.6 and 2.7%, Table 1). The false-positive rate for the Vircell kit is consistent with previously reported results [5]. When this is compared with the in-house IF test, the Vircell kits’ false-positive percent turns out to be lower, whereas it seems that the test lacks sensitivity as it only detects 62.5% of the seropositive samples. The sera which were positive for antibodies against Pseudomonas aeruginosa, Coxiella burnetii and Campylobacter jejuni/coli showed the highest level of false-positive/cross-reactivity in the kits (Tables 1 and 2), which is consistent with previously reported results [9–11].
It should be mentioned that in this evaluation of the commercial kits, the in-house IF test was chosen to be the gold standard, since all the tested samples were selected according to positivity in this assay. Due to this, the sensitivity of this in-house assay is 100%. To assure that the serum samples really are true positives, only samples from patients with legionellosis having been laboratory confirmed by at least one other test were used.
However, one should be aware that the selection of serum samples according to other criteria may change the obtained sensitivity.
The relative sensitivity of the kits was also calculated for the L. pneumophila serogroups identified by culture. The Focus Diagnostics and SERION ELISA classic kits both detected about 80% of the L. pneumophila sg. 1 positive patients, whereas the Zeus Scientific, Inc. and Vircell kits only found about 56% positive. For L. pneumophila non-sg. 1 (8 cases), the Focus Diagnostics and the SERION ELISA classic kits found 80%, the Vircell kit found 62.5% positive and Zeus Scientific, Inc. only found 33.3% positive. Taking all the tested serogroups together the Focus Diagnostics is the kit with the highest relative sensitivity (81.6%) to the different serogroups. The SERION ELISA classic kits have a total relative sensitivity of 78.9% for the four different serogroups tested. The Zeus Scientific, Inc. and Vircell ELISA kits both have low sensitivities (57.6 and 52.6%) for all of the tested serogroups, but the Zeus Scientific, Inc. especially lacks sensitivity to non-sg. 1.
This comparison of serological methods for the diagnosis of legionellosis confirms that the diagnosis cannot be based on one serum sample from the patient; a reliable diagnosis based on serology is still dependent on paired serum samples for detection of a significant change in the specific antibody level. This is due to a rather high false-positive rate in all the investigated methods. Positive antibody titres in sera from patients without legionellosis may be due to previous Legionella infections or cross-reacting antibodies. Although an assay with a false-positive rate of 2–5% (specificity of 95–98%) can be considered rather specific, the predictive value of a positive test for the assay will be as poor as approximately 50%, if the incidence of the disease among investigated patients is on the same level (2–5%), which is probably the true incidence of Legionnaires’ disease among pneumonia cases. One major disadvantage of the investigated commercial kits is that the antigens of the different serogroups are pooled; as only a significant change in the antibody level to L. pneumophila sg. 1 can be considered a verified diagnosis (WHO, EWGLI, ECDC),Footnote 1 these assays cannot be used to verify the diagnosis. As serology based on paired sera in most cases cannot be confirmed until rather late in the course of the disease it is advisable to use other diagnostic tests in combination with serology.
Notes
Homepage from 270207: http://www.ewgli.org/ewglinet/case_definitions.htm. Weekly epidemiological record, WHO, 1998,73,257–264, No 34.
References
Murray PR, Rosenthal KS, Kobayashi GS, Pfaller MA (2002) Medical microbiology, 4th edn. Mosby, St. Louis, MO
Helbig JH, Uldum SA, Lück PC, Harrison TG (2001) Detection of Legionella pneumophila antigen in urine samples by the BinaxNOW immunochromatographic assay and comparison with both Binax Legionella Urinary Enzyme Immunoassay (EIA) and Biotest Legionella Urine Antigen EIA. J Med Microbiol 50:509–516
Ginevra C, Barranger C, Ros A, Mory O, Stephan J-L, Freymuth F, Joannès M, Pozzetto B, Grattard F (2005) Development and evaluation of Chlamylege, a new commercial test allowing simultaneous detection and identification of Legionella, Chlamydophila pneumoniae, and Mycoplasma pneumoniae in clinical respiratory specimens by multiplex PCR. J Clin Microbiol 43:3247–3254
Edelstein PH (1987) Laboratory diagnosis of infections caused by legionellae. Eur J Clin Microbiol 6:4–10
Diederen BMW, Kluytmans JAJW, Peeters MF (2005) Evaluation of Vircell enzyme immunoassay and indirect immunofluorescent assay for the detection of antibodies against Legionella pneumophila. Clin Vaccine Immunol 13:361–364
Boshuizen HC, Den Boer JW, de Melker H, Schellekens JF, Peeters MF, van Vliet JA, Conyn-van Spaendonck MA (2003) Reference values for the SERION classic ELISA for detecting Legionella pneumophila antibodies. Eur J Clin Microbiol Infect Dis 22:706–708
Malan AK, Martins TB, Jaskowski TD, Hill HR, Litwin CM (2003) Comparison of two commercial enzyme-linked immunosorbent assays with an immunofluorescence assay for detection of Legionella pneumophila types 1 to 6. J Clin Microbiol 41:3060–3063
Uldum SA, Mølbak K (2002) PCR as a routine method for diagnosis of Legionnaires’ disease. In: Marre R, Kwaik YU (eds) Legionella. ASM Press, Washington, D.C., pp 213–215
Finidori JP, Raoult D, Bornstein N, Fleurette J (1992) Study of cross-reaction between Coxiella burnetii and Legionella pneumophila using immunofluorescence assay and immunoblotting. Acta Virol 5:459–465
Collins MT, Espersen F, Høiby N, Cho SN, Friis-Møller A, Reif JS (1983) Cross-reactions between Legionella pneumophila (serogroup 1) and twenty-eight other bacterial species, including other members of the family Legionellaceae. Infect Immun 3:1441–1456
Marshall LE, Boswell TCJ, Kudesia G (1994) False positive legionella serology in campylobacter infection: campylobacter serotypes, duration of antibody response and elimination of cross-reactions in the indirect fluorescent antibody test. Epidemiol Infect 112:347–357
McDonough EA, Barrozo CP, Russell KL, Metzgar D (2005) A multiplex PCR for detection of Mycoplasma pneumoniae, Chlamydophila pneumoniae, Legionella pneumophila, and Bordetella pertussis in clinical specimens. Mol Cell Probes 19:314–322
Edelstein P (1993) Laboratory diagnosis of Legionnaires’ disease: an update from 1984. In: Legionella: current status and emerging perspectives. Barbaree J, Breiman RF, Dufour AP (eds) American Society for Microbiology, Washington, D.C., pp 7–11
Bangsborg JM, Friis-Møller A, Rechnitzer C, Høiby N, Lind K (1988) The E. coli immunosorbent as used in serodiagnosis of Legionella infections studied by crossed immunoelectrophoresis. APMIS 96:177–184
Wilkinson HW, Fikes BJ, Cruce DD (1979) Indirect immunofluorescence test for serodiagnosis of Legionnaires’ disease: evidence for serogroup diversity of Legionnaires’ disease bacterial antigens and for multiple specificity of human antibodies. J Clin Microbiol 9:379–383
Acknowledgements
We thank Helle Krogh Johansen (Rigshospitalet, Denmark) for supplying the P. aeruginosa sera and Eva Rasmussen (Statens Serum Institut, Denmark) for supplying all the other sera and control sera.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elverdal, P., Jørgensen, C.S. & Uldum, S.A. Comparison and evaluation of four commercial kits relative to an in-house immunofluorescence test for detection of antibodies against Legionella pneumophila . Eur J Clin Microbiol Infect Dis 27, 149–152 (2008). https://doi.org/10.1007/s10096-007-0410-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-007-0410-5