Abstract
Introduction
Cognitive symptoms are reported commonly throughout all phases of a migraine; however, there is a paucity of objective cognitive profiling. Previous studies have been limited by practice effect, and variable populations.
Methods
Participants completed 1 month of daily testing with a computerised cognitive battery involving a simple reaction (SRT), choice reaction (CRT) and a working memory test (WM). Results were correlated with their diary to identify interictal scores, and scores during each phase of a migraine, and non-migraine headache days.
Results
A total of 16 patients with episodic migraine participated. During the headache phase of a migraine, responses to SRT, CRT and WM tasks were significantly slower and less accurate than interictally. During the postdrome, WM task performance was slower and less accurate. Non-migraine headache days were not associated with significant change.
Conclusion
The headache and postdromal phase of a migraine day was associated with objective evidence of cognitive dysfunction in patients with episodic migraine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cognitive dysfunction is the second most disabling symptom of a migraine attack, and is likely to be responsible for some of the significant economic burden of migraine [1]. Cognitive dysfunction is the most frequent symptom complex in the prodromal phase [2]. It persists throughout the headache phase, during which up to 90% of patients report the inability to concentrate, and the postdromal phase, in which 40% of patients report impaired concentration [2, 3].
Use of neuropsychological tests to assess cognitive effects of migraine is limited by variance in healthy adults with higher cognitive baselines, practice effects of repeat testing, and the burden of repeat testing for clinicians and patients [4,5,6]. Several previous studies have attempted to assess cognition during a migraine attack, and have variably found transient declines in processing speed and working memory [7,8,9]. The goal of this study is to use a previously validated and very short set of computerised cognitive tests that patients can complete at home to assess the impact of cognitive dysfunction during each phase of a migraine, and a non-migrainous headache day in comparison to the interictal baseline.
Methodology
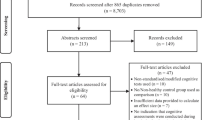
We undertook a single-centre prospective cohort study in patients who met the International Classification of Headache Disorders, third edition (ICHD-3) criteria for episodic migraine. Participants who were on stable preventative treatment for their migraine, did not take opiates for acute treatment and had no confounding medical or psychiatric comorbidity were eligible for the study.
Participants were educated on identifying migraine days and non-migraine headache days by a headache specialist, and then, following a practice session, asked to complete 1 month of daily home testing while keeping a headache diary. Participants had a computerised cognitive battery (“MSReactor”), and were asked to perform a test at the same time daily for the study duration. Participants were allowed to continue a stable dose of their usual acute and preventative migraine treatment throughout the study period.
The MSReactor test battery is accessible to participants via the internet, and consists of three simple graphical game-like tests including a psychomotor/simple reaction test (SRT), a visual attention choice reaction test (CRT) and a working memory one-back test (WM) [10]. The test battery that has previously been utilised in several neurological disorders, including migraine, has demonstrated correlation with more extensive cognitive tests, and demonstrates limited practice effects, reaching a stable baseline within three repetitions [10,11,12].
Practise, or learning effect, is a significant consideration in the concurrent application of test batteries. The learning effect and test–retest reliability of the MSReactor battery has been determined previously [10]. The learning effect of this battery stabilises within three repetitions. To account for the impact of learning effect on the study, the first five repetitions for each participant were considered practices, and not included in the analysis.
The impact of migraine state on test results was measured by reaction speed (milliseconds) and test accuracy (percentage of correct responses in each trial). The first 5 days were not included in the analysis to allow stabilisation of practice effect. Interictal tests were defined as tests that were completed on days at least 2 days separate from a recorded migraine or headache, and these results were averaged to provide a patient’s interictal baseline.
Where a patient had more than one qualifying event, the first qualifying migraine or non-migraine headache day was chosen for analysis. The prodrome and postdrome phase in the study was defined as the day of testing preceding or following the headache phase on a migraine day, as marked in the patient diary.
Statistical analysis was performed using SPSS v28.0. Population characteristics were summarised with descriptive statistics. A Wilcoxon signed rank test was used to analyse non-normally distributed paired samples. Test results were considered significant when p < 0.05. This study received institutional review board approval (HREC 153/21).
Results
A total of 16 patients with episodic migraine were enrolled in the study, with population demographics described in Table 1. All the participants recorded a migraine day, and 14 of 16 participants recorded a non-migraine headache day. All participants had stable medications throughout the study period, and 50% were receiving botulinum toxin, 12.5% CGRP monoclonal antibodies and 25% oral preventative therapies in treatment of their migraines. 87.5% (14/16) of the cohort used triptans as an acute abortive agent, and the remainder non-steroidal anti-inflammatories.
During the headache phase of a migraine day, response in the SRT task was 8.2% slower than baseline (z = − 2.923, p = 0.003), the average response time in the CRT was 10.2% slower (z = − 3.206, p < 0.001), and response time in the WM was 5.6% slower (z = − 2.172, p = 0.030). The accuracy of response for SRT (z = − 2.219, p = 0.026), CRT (z = − 2.097, p = 0.036) and WM tasks (z = − 2.371, p = 0.018) were all significantly lower than baseline. A summary of test results is provided in Table 2.
On the postdromal test day, the WM test was 8.9% slower than baseline (z = − 2.198, p = 0.028), and significantly less accurate (z = − 2.456, p = 0.014). Response speed for the WM test is summarised in Fig. 1. SRT on postdromal days was less accurate than baseline (z = − 2.067, p = 0.039); however, response times for SRT and CRT were not significantly different. Neither the prodromal test day nor non-migraine headache test day were associated with a change in SRT, CRT or WM response time or accuracy compared to interictal baseline. There was no significant difference in severity of pain on migraine and non-migraine headache days (z = − 0.051, p = 0.959).
Discussion
We showed that performance on validated tests of WM, SRT and CRT worsens during the headache and postdromal phase of a migraine, but not on a non-migraine headache day, in comparison to a patients interictal baseline. This is the first study to utilise home-based computerised cognitive tests to examine the effect of cognition during the phases of a migraine, and a non-migrainous headache day.
These findings are broadly in keeping with several previous studies that have variably reported transient declines in processing speed, working memory and immediate and sustained attention during the headache phase of a migraine [7, 9]. It provides further validation of patient reports of cognitive symptoms during the migraine postdromal phase [2, 3].
Possible explanations for altered cognition in migraine have been summarised previously [13]. Previous observations include increased functional connectivity and fMRI activation in the temporal lobe in patients with migraine, and deficits in task-related suppression during acute pain, irrespective of pain catastrophizing or pain intensity [14,15,16]. Variations in grey matter density have also been reported in patients with migraine [17].
Our study provides several insights into contributory mechanisms to cognitive symptoms in migraine. Firstly, our observation of an impact on test scores on a migraine, but not on a non-migraine headache day, is significant. One hypothesis and possible confounder is that cognitive symptoms and test results relate to ‘distraction by pain’, our observation that there was no significant difference in pain severity between migraine and headache days, but that only migraine days were associated with significant deviations on testing, suggests that distraction by pain is not an adequate explanation for cognitive symptoms. Given deficits in task-related suppression during acute pain seen in fMRI studies however [15], pain remains a significant possible confounder in the design of cognitive study.
Secondly, the findings of our study describe a dynamic process impacting markers of cognition in migraine, that is not completely explained by static changes in grey matter density. In Mathur et al.’s fMRI study, patients with migraine underwent cognitive testing during and in the absence of painful stimuli [16]. Evidence of abnormally blunted cognitive task-related deactivation of the left dorsolateral prefrontal cortex and left dorsal anterior midcingulate cortex suggested alterations of cognitive processing in migraine, which were further modulated by migraine frequency [16]. Furthermore, functional studies have also shown increased activation of cortical areas related to executive function during a migraine attack [18]. Taken together, this suggests maladaptive functional connectivity of altered pain-cognition networks in migraine that are associated with attack frequency, which may explain the association of migraine with cognitive symptoms.
There are several limitations to this study. The lack of observed change during the defined prodromal period may relate to the timing of the test, which was defined retrospectively from the headache phase rather than prospectively from reported symptoms. Secondly, due to the study design and sample size, the generalisability to chronic migraine, and association with disease frequency and duration were not investigated, however the study design, utilising paired samples, controls for variation in education and background. The study population included patients who were on a preventative agent for migraine. As they were all on a stable regimen, this was felt to not be responsible for the observed variation in cognition, and an accurate representation of the lived experience of a patient with migraine. Finally, the effect of other variables such as altered sleep during a migraine was not examined. Given the observation that poor sleep quality may precede a migraine attack [19, 20] and the impact of sleep on cognitive performance [21], this is a significant confounder that requires further study.
Conclusion
Cognitive test performance in terms of working memory, simple reaction and choice reaction time is lower on a migraine and postdromal day compared to interictally in patients with episodic migraine. Further study is required to assess the interaction between migraine frequency, severity, disease duration and sleep on cognitive function. Sensitive cognitive testing may allow migraineurs to determine when they should return to work duties that depend on their normal cognitive function.
Data availability
Primary data is available on reasonable request to the corresponding author.
References
Gil-Gouveia R, Oliveira AG, Martins IP (2016) The impact of cognitive symptoms on migraine attack-related disability. Cephalalgia [Internet] 36(5):422–30. Available from: http://journals.sagepub.com/doi/10.1177/0333102415604471. Accessed 26 Jun 2023
Gil-Gouveia R, Martins IP (2018) Clinical description of attack-related cognitive symptoms in migraine: a systematic review. Cephalalgia [Internet] 38(7):1335–50. Available from: http://journals.sagepub.com/doi/10.1177/0333102417728250. Accessed 26 Jun 2023
Gil-Gouveia R, Oliveira AG, Martins IP (2016) Subjective cognitive symptoms during a migraine attack: a prospective study of a clinic-based sample. Pain Phys 19(1):E137–E150
Alenius M, Koskinen S, Hallikainen I et al (2019) Cognitive performance among cognitively healthy adults aged 30–100 years. Dement Geriatr Cogn Dis Extra [Internet] 9(1):11–23. Available from: https://www.karger.com/Article/FullText/495657. Accessed 26 Jun 2023
McCaffrey RJ, Ortega A, Orsillo SM et al (1992) Practice effects in repeated neuropsychological assessments. Clin Neuropsychol [Internet] 6(1):32–42. Available from: http://www.tandfonline.com/doi/abs/10.1080/13854049208404115. Accessed 26 Jun 2023
Bartels C, Wegrzyn M, Wiedl A et al (2010) Practice effects in healthy adults: a longitudinal study on frequent repetitive cognitive testing. BMC Neurosci [Internet] 11(1):118. Available from: https://bmcneurosci.biomedcentral.com/articles/10.1186/1471-2202-11-118. Accessed 26 Jun 2023
Gil-Gouveia R, Oliveira AG, Martins IP (2015) Cognitive dysfunction during migraine attacks: a study on migraine without aura. Cephalalgia [Internet] 35(8):662–74. Available from: http://journals.sagepub.com/doi/10.1177/0333102414553823. Accessed 26 Jun 2023
Mulder E, Linssen W, Passchier J et al (1999) Interictal and postictal cognitive changes in migraine. Cephalalgia [Internet] 19(6):557–65. Available from: http://journals.sagepub.com/doi/10.1046/j.1468-2982.1999.019006557.x. Accessed 26 Jun 2023
Meyer JS, Thornby J, Crawford K et al (2000) Reversible cognitive decline accompanies migraine and cluster headaches. Headache J Head Face Pain [Internet] 40(8):638–46. Available from: http://doi.wiley.com/10.1046/j.1526-4610.2000.040008638.x. Accessed 26 Jun 2023
Merlo D, Darby D, Kalincik T et al (2019) The feasibility, reliability and concurrent validity of the MSReactor computerized cognitive screening tool in multiple sclerosis. Ther Adv Neurol Disord [Internet] 12:175628641985918. Available from: http://journals.sagepub.com/doi/10.1177/1756286419859183. Accessed 26 Jun 2023
Ho S, Darby D, Bear N (2020) Cognitive effects of onabotulinumtoxinA in chronic migraine. BMJ Neurol Open [Internet] 2(1):e000014. Available from: https://neurologyopen.bmj.com/lookup/doi/10.1136/bmjno-2019-000014. Accessed 26 Jun 2023
Yam C, Merlo D, Stankovich J et al (2020) The MSReactor computerized cognitive battery correlates with the processing speed test in relapsing-remitting multiple sclerosis. Mult Scler Relat Disord [Internet] 43:102212. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2211034820302881. Accessed 26 Jun 2023
Gil-Gouveia R, Martins IP (2019) Cognition and cognitive impairment in migraine. Curr Pain Headache Rep 23(11)
Moulton EA, Becerra L, Maleki N et al (2011) Painful heat reveals hyperexcitability of the temporal pole in interictal and ictal migraine states. Cereb Cortex [Internet] 21(2):435–48. Available from: https://academic.oup.com/cercor/article-lookup/doi/10.1093/cercor/bhq109. Accessed 26 Jun 2023
de Tommaso M, Valeriani M, Guido M et al (2003) Abnormal brain processing of cutaneous pain in patients with chronic migraine. Pain [Internet] 101(1):25–32. Available from: https://journals.lww.com/00006396-200301000-00004. Accessed 26 Jun 2023
Mathur VA, Khan SA, Keaser ML et al (2015) Altered cognition-related brain activity and interactions with acute pain in migraine. NeuroImage Clin [Internet] 7:347–58. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2213158215000042. Accessed 26 Jun 2023
Tortorella P, Rocca MA, Colombo B et al (2006) Assessment of MRI abnormalities of the brainstem from patients with migraine and multiple sclerosis. J Neurol Sci [Internet] 244(1–2):137–41. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0022510X06000372. Accessed 26 Jun 2023
Tolner EA, Chen S-P, Eikermann-Haerter K (2019) Current understanding of cortical structure and function in migraine. Cephalalgia [Internet] 39(13):1683–99. Available from: http://journals.sagepub.com/doi/10.1177/0333102419840643. Accessed 26 Jun 2023
Proserpio P, Agostoni EC (2020) Sleep and migraine. Neurol Sci [Internet] 41(S2):437–8. Available from: https://link.springer.com/10.1007/s10072-020-04644-7. Accessed 26 Jun 2023
Duan S, Ren Z, Xia H et al (2022) Association between sleep quality, migraine and migraine burden. Front Neurol [Internet] 13. Available from: https://www.frontiersin.org/articles/10.3389/fneur.2022.955298/full. Accessed 26 Jun 2023
Gildner TE, Liebert MA, Kowal P et al (2014) Associations between sleep duration, sleep quality, and cognitive test performance among older adults from six middle income countries: results from the Study on Global Ageing and Adult Health (SAGE). J Clin Sleep Med [Internet] 10(06):613–21. Available from: http://jcsm.aasm.org/doi/10.5664/jcsm.3782. Accessed 26 Jun 2023
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Contributions
JCR conceptualised the study with input from EH, MM, HB and DD. JCR was responsible for project administration and data analysis. JCR drafted the original draft and all authors contributed extensively to the interpretation of data, review and editing. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study received institutional review board approval (Alfred Health HREC 153/21). Patients provided informed consent to participate in this study.
Competing interests
Dr. Ray has received funding for educational activity from Abbvie, Novartis and Viatris. He has served on medical advisory boards for Pfizer, Viatris, and Lilly. Professor Butzkueven’s institution (Monash University) received compensation for consulting, talks, and advisory/steering board activities from Alfred Health, Biogen, Merck, Novartis, Roche and UCB; research support from Biogen, Merck, MS Research Australia, National Health and Medical Research (Australia), Medical Research Future Funds (Australia) Novartis, the Oxford Health Policy Forum, and Roche. He has received personal compensation for steering group activities from Oxford Health Policy Forum. Prof. Matharu serves on the advisory board for Allergan, Novartis, Eli Lilly, Autonomic Technologies Inc and TEVA and has received payment for the development of educational presentations from Allergan, electroCore, Eli Lilly, Novartis and TEVA. Dr. Hutton has served on advisory boards for Sanofi-Genzyme, Novartis, Teva, Eli Lilly, Allergan, Lundbeck, been involved in clinical trials sponsored by Novartis, Teva, Xalud, Cerecin, and has received payment for educational presentations from Allergan, Teva, Eli Lilly and Novartis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ray, J.C., Darby, D., Butzkueven, H. et al. Cognitive assessment during the phases of a spontaneous migraine: a prospective cohort study. Neurol Sci (2024). https://doi.org/10.1007/s10072-024-07520-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10072-024-07520-w