Abstract
Alzheimer’s disease, prevalent in individuals aged 60 and above, constitutes most dementia cases and significantly impairs memory and cognitive functions. With global Alzheimer’s cases projected to triple by 2050, there is a pressing need for effective interventions. Lecanemab, a monoclonal antibody targeting amyloid-beta plaques, shows promise in slowing Alzheimer’s progression. Positive clinical trial results have instilled hope in patients, prompting ongoing research to advance understanding and intervention possibilities. To contribute to this knowledge base, we conducted a systematic review and meta-analysis, focusing on lecanemab’s efficacy and safety at a dosage of 10 mg/kg. This comprehensive approach aimed to address gaps in the current literature, scrutinize research disparities, and guide future investigations. Applying strict inclusion/exclusion criteria, we assessed study details, participant information, and intervention specifics, using the Cochrane risk of bias tool for quality evaluation. Statistical analyses, conducted with R software, included risk ratios and mean differences, assessing heterogeneity and publication bias. The meta-analysis reveals a significant positive effect of lecanemab (10 mg/kg biweekly) on cognitive outcomes in Alzheimer’s disease. Consistent reductions in ADCOMS, CDR-SB, and ADAS-cog14 scores across studies indicate drug efficacy with narrow confidence intervals and no significant heterogeneity. While TEAE shows no significant difference, heightened risks of ARIA-E and ARIA-H associated with lecanemab underscore the need for vigilant safety monitoring in clinical practice. Despite the drug efficacy, the study emphasizes a balanced assessment of benefits and potential risks associated with lecanemab, providing critical insights for clinicians evaluating its use in addressing cognitive impairment in individuals with Alzheimer’s disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is a neurodegenerative disorder causing memory and cognitive decline, significantly impacting the quality of life, especially in individuals aged 60 and older, constituting approximately 70% of dementia cases [1, 2]. According to the Alzheimer’s Association, approximately a third of elderly people die with AD or similar dementia. The global prevalence of AD is expected to triple by 2050, reaching over 100 million cases, with variations attributed to demographics, age, and diagnostic criteria [2]. Notably, AD incidence increased by 40% in Umea, Sweden, from 2001 to 2006, underscoring the need for effective interventions [3].
Lecanemab, a monoclonal antibody, aims to slow AD progression and improve cognitive function by targeting Aβ plaques, a hallmark feature of AD pathology. Its mechanism involves binding to aggregated forms of the protein, promoting clearance from the brain, and reducing amyloid-beta burden [4, 5]. By targeting the toxic protofibrils of amyloid-β, lecanemab may have a disease-modifying effect that slows down the progression of cognitive and functional deficits in AD patients. This can help improve the quality of life for patients with mild AD and their families. However, it is not yet known whether the medicine helps in other ways such as slowing the development of AD in people without symptoms of memory loss [6,7,8].
Several clinical trials have produced positive findings about lecanemab, also known by its generic name BAN2401, regarding its safety and possible efficacy [4, 5]. There is ongoing research for the development of lecanemab to target the roots of AD, which may offer new hope for AD patients [9]. Use of lecanemab in older, less healthy, less well-educated, and more diverse populations, who are not included in previous clinical trials, may result in efficacy and safety outcomes that differ from those observed in trials [10].
The Food and Drug Administration (FDA) accelerated approval for lecanemab was granted in January 2023, acknowledging its potential in a population not included in previous clinical trials Despite promising phase III data indicating a 27% reduction in cognitive decline over 18 months, the FDA decision was based on phase II results, emphasizing the need for further research and caution in its use, currently restricted to individuals with mild cognitive impairment consistent with the clinical trial group [11].
In a study on lecanemab use compared to placebo in early Alzheimer’s, 1795 participants were enrolled, half of them received lecanemab. Results showed reduced amyloid markers and a slower cognitive decline over 18 months, but adverse events necessitate more extensive trials [12]. In the lecanemab Study 201 Core, a double-blind trial with 856 patients, 10 mg/kg of lecanemab biweekly significantly reduced amyloid plaques, slowed clinical decline over 12–18 months, and highlighted potential disease-modifying effects [6].
Our systemic review attempted to reduce bias with the use of explicit methods to perform a comprehensive literature search and critical appraisal of individual studies. Meta-analyses were aimed to assess the strength of evidence present on the lecanemab 10 mg/kg efficacy and safety. For efficacy, one aim was to determine whether an effect exists; another aim was to determine whether the effect is positive or negative and, ideally, to obtain a single summary estimate of the effect. For safety, the goal was to determine the presence of potential harm and quantify their risk, ideally providing a single summary estimate of safety concerns.
Material and methods
Search strategy
We conducted a comprehensive search across electronic databases, including PubMed, Scopus, Web of Science, Cochrane Library, and Clinical Trials.gov for publication period ranging from 2010 to 2023. The initial clinical trial on lecanemab (NCT01230853) took place in 2010 [13]. The search strategy used was “lecanemab OR leqembi OR BAN2401 OR BAN 2401 OR BAN-2401 AND Alzheimer’s disease OR Acute Confusional Senile Dementia OR Presenile Dementia OR Senile Dementia OR Alzheimer dementia (AD) OR Alzheimer sclerosis OR Alzheimer syndrome OR Alzheimer-type dementia OR ATD OR DAT OR Familial Alzheimer disease OR FAD” and their association with various Alzheimer’s disease-related terms, with a language constraint of English. This limitation was imposed due to language restrictions.
Our systematic review and meta-analysis specifically focused on peer-reviewed randomized controlled trials (RCTs) for several reasons. RCTs are widely acknowledged as the gold standard for establishing causality in research due to their randomized nature, which effectively controls for confounding variables and allows us to confidently attribute observed outcomes to the intervention being studied. The inherent design of RCTs also contributes to high internal validity by minimizing biases and ensuring that baseline characteristics are evenly distributed among intervention and control groups. Given that our primary objective is to assess the comparative effectiveness of interventions, RCTs facilitate a rigorous comparison between different interventions or between intervention and control groups. Moreover, RCTs hold a prominent position in the evidence hierarchy, providing robust and reliable evidence for clinical decision-making. While we recognize the potential value of other study designs, our deliberate choice to focus on RCTs aligns with our commitment to ensure the highest methodological rigor and internal validity in this systematic review.
Study selection
We included peer-reviewed RCTs conducted in English that compare lecanemab at a dosage of 10 mg/kg biweekly against a placebo in AD patients. Included studies reported outcomes related to Alzheimer’s Disease Composite Score (ADCOMS), Alzheimer’s Disease Assessment Scale-Cognitive Subscale 14-item version (ADAS-Cog14), and Clinical Dementia Rating Scale-Sum of Boxes (CDR-SB).
In this study, the inclusion criteria encompass patients diagnosed with Alzheimer’s disease, with a specific focus on assessing the efficacy and safety of lecanemab in comparison to a placebo through peer-reviewed RCTs. There are no restrictions on age, gender, location, or ethnicity, allowing for a comprehensive examination across diverse patient groups. To maintain precision and reliability, the exclusion criteria involve the exclusion of animal studies, in vitro investigations, observational or laboratory studies, and research with redundant findings. Additionally, abstract-only presentations, reviews, books, posters, theses, editorials, notes, letters, case reports, case series, and conference papers are excluded, ensuring a stringent focus on peer-reviewed RCTs in this thorough analysis (Table 1). Studies were selected based on the inclusion and exclusion criteria by two independent authors (K.A., B.A) and cross-checked by K.A. and A.A.A. Any disagreement was settled by consensus among all authors.
Data extraction
The data extraction was conducted by two investigators (K.A. and A.A.A.) and cross-checked by K.A. and B.A. The extracted information encompasses study characteristics, participant details, intervention specifics, outcome measures, and funding sources. For quantitative data, (mean differences [standard error (SE)]) used for ADCOMS, ADAS-Cog14, and CDR-SB. In addition, we extract data for treatment-emergent adverse events (TEAE), amyloid-related imaging abnormalities hemorrhage (ARIA-H), and amyloid-related imaging abnormalities edema (ARIA-E) to evaluate the safety of lecanemab 10 mg/kg biweekly.
Regarding missing data, we made efforts to obtain it and calculate mean differences [SE] from the original studies. If this is not feasible, imputation techniques such as mean imputation, utilized to estimate missing values, recognize the potential introduction of bias into the analysis.
Quality assessment
The quality of the studies was appraised independently by K.A. and A.A.A. and cross-checked by B.A. and H.A. We assessed the risk of bias in included studies using the Cochrane risk of bias tool for RCTs. This tool is transparent, reproducible, and facilitates evidence-based decision-making by identifying potential biases in study design and reporting [14].
Data synthesis
Statistical analyses were conducted using R software 4.2.2. For binary variables, risk ratios (RR) with 95% confidence intervals (CI) were calculated. Continuous outcomes were analyzed using the mean differences [SE] with a 95% CI. Heterogeneity among studies was assessed using the Cochrane Q p-value and I2 statistic, with a random effects model and common effect model. Publication bias was evaluated using funnel plots and Egger’s regression test.
We would like to highlight that this systematic review and meta-analysis has been diligently registered on Prospero, an international prospective register of systematic reviews. The registration number for this study is CRD42023430184.
Results
Study selection and characteristics
The literature search yielded 380 records, of which 55 were duplicates. The remaining 325 articles were then evaluated based on title and abstract, with 292 deemed irrelevant and removed. The remaining 33 articles were evaluated using full text for eligibility, and 29 were excluded. The overall count of incorporated studies is 4.
Figure 1 outlines the schematic flow of the studies’ identification and inclusion processes. The characteristics of the studies included are shown in Table 2. Four articles comprising 2176 patients who received the treatment, and 1407 controls were included in this study.
McDade et al.’s study is an extension of the work presented in Swanson et al. Both studies are intricately connected, with McDade et al. building upon the findings and insights reported in Swanson et al. The term “extension” in this context indicates a sequential or follow-up study that delves deeper into specific aspects or expands upon the initial investigation presented in the earlier work.
The funding landscape for the discussed studies on lecanemab highlights the substantial support provided by pharmaceutical entities for advancing Alzheimer’s research and therapeutic development. Eisai Inc., a prominent pharmaceutical company, emerges as a key contributor, backing the trials conducted by Logovinsky et al., McDade et al., Swanson et al., and Van Dyck et al. These multinational, multicenter studies, published in esteemed journals such as Alzheimer’s Research & Therapy and The New England Journal of Medicine, collectively involved thousands of participants across various regions. The financial backing from Eisai Inc. demonstrates a strategic commitment to advancing the understanding and treatment of Alzheimer’s disease. The collaboration between academia and industry, evident in these studies, underscores the collaborative effort required to address the complex challenges posed by neurodegenerative diseases, with funding playing a pivotal role in driving such groundbreaking research endeavors.
Interpreting gender differences in included studies
In comparing gender ratios between case and control groups across four studies, a notable variation emerges in the observed associations. Swanson et al.’s study reveals a significant disparity, with individuals in the study group having substantially lower odds of being in the case group compared to controls (p < 0.0001). Conversely, Van Dyck et al., McDade et al., and Logovinsky et al. report less pronounced differences, with p-values of 0.179, 0.688, and 0.488, respectively, failing to reach statistical significance (Table 3).
Treatment effect
Lecanemab 10 mg/kg vs. placebo effect on ADCOMS change
The findings from our meta-analysis revealed a statistically significant decrease (p-value < 0.0001) in ADCOMS scores when lecanemab is administered at a 10 mg/kg dosage compared to a placebo. Both the common effect model and the random effects model estimate a mean difference of − 0.0508, and the narrow 95% confidence intervals suggest a consistent effect size across the studies.
Furthermore, the absence of significant heterogeneity (I2 = 0.0%) among the studies implies a consensus regarding the impact of lecanemab on ADCOMS scores. The test of heterogeneity (Q statistic) yields a p-value of 0.9545, indicating a lack of significant heterogeneity, and suggesting a high degree of consistency in the findings across the studies (Fig. 2A). For further details, please refer to Sect. 1 in the supplementary file.
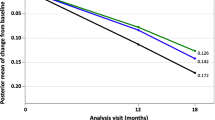
Lecanemab 10 mg/kg vs. placebo effect on CDR-SB change
The results of the meta-analysis suggest that the administration of lecanemab at a dosage of 10 mg/kg biweekly is linked to a statistically significant reduction (p < 0.0001) in CDR-SB scores compared to a placebo. Both the common effect model and the random effects model estimate a mean difference of approximately − 0.4264, with narrow 95% confidence intervals, indicating consistency in the effect size across the studies.
The absence of significant heterogeneity (I2 = 0.0%) among the studies indicates a consensus in their findings, further supporting the strength of the results. The test of heterogeneity (Q statistic) yields a p-value of 0.9339, signifying a lack of significant heterogeneity among the studies and suggesting relative consistency in their findings (Fig. 2B). For further details, please refer to Sect. 2 in the supplementary file.
Lecanemab 10 mg/kg vs. placebo effect on ADAS-cog14 change
The results of the meta-analysis indicate that administering lecanemab at a 10 mg/kg dosage biweekly leads to a statistically significant reduction (p < 0.0001) in ADAS-cog14 scores compared to a placebo in patients diagnosed with Alzheimer’s disease. Both the common effect model and the random effects model estimate a mean difference of approximately − 1.3416, with narrow 95% confidence intervals, highlighting a consistent effect size across studies.
The absence of significant heterogeneity (I2 = 0.0%) among the studies suggests agreement in their findings, further supporting the reliability of the results. The heterogeneity test (Q statistic) yields a p-value of 0.4550, indicating a lack of significant heterogeneity among the studies and suggesting a relatively consistent pattern in their findings (Fig. 2C). For further details, please refer to Sect. 3 in the supplementary file.
Safety concerns
Lecanemab 10 mg/kg vs. placebo effect on any TEAE outcome
The meta-analysis results concerning the occurrence of TEAE when comparing lecanemab at a dosage of 10 mg/kg administered biweekly to placebo shows that the random effects model estimates a pooled relative risk (RR) of 0.6647. However, the 95% CI is wide indicating no effect, and the p-value is 0.3034, signifying a lack of statistical significance.
Additionally, there is significant heterogeneity among the studies, with an I2 of 96.8%. This suggests diverse findings regarding TEAE outcomes across the studies (Fig. 3A). For further details, please refer to Sect. 4 in the supplementary file.
Lecanemab 10 mg/kg vs. placebo effect on ARIA-E outcome
The meta-analysis findings for the occurrence of ARIA-E when comparing lecanemab at a dosage of 10 mg/kg administered biweekly to placebo are outlined as shows that the random effects model estimates a pooled RR of 7.9613, with a 95% CI of [4.8358; 13.1068], and a very low p-value (< 0.0001), indicating a statistically significant increased risk of ARIA-E associated with lecanemab treatment.
Furthermore, there is no significant heterogeneity among the studies, as indicated by the p-value of 0.5430 and an I2 of 0.0%. This implies that the studies are consistent in their findings regarding the risk of ARIA-E (Fig. 3B). For further details, please refer to Sect. 5 in the supplementary file.
Lecanemab 10 mg/kg vs. placebo effect on ARIA-H outcome
The meta-analysis results for the occurrence of ARIA-H when comparing lecanemab at a dosage of 10 mg/kg administered biweekly to placebo reveal that the pooled RR estimated by the random effects model is 1.7533, with a 95% CI of [1.3488; 2.2790], and a very low p-value (< 0.0001). This indicates a statistically significant increased risk of ARIA-H associated with lecanemab treatment.
Moreover, there is no significant heterogeneity among the studies, as indicated by the p-value of 0.4088 and an I2 of 0.0%. This suggests that the studies are consistent in their findings regarding the risk of ARIA-H (Fig. 3C). Retrieved data related to adverse events are depicted in Table 4. For further details, please refer to Sect. 6 in the supplementary file.
Publication bias testing and sensitivity analyses
Funnel plots and Egger’s tests were carried out to evaluate the publication bias (Fig. 4A, B, C). The results indicated no evidence of significant publication bias, as demonstrated by the Egger’s test with a p-value greater than 0.05.
The results of the regression test for funnel plot asymmetry for ADCOMS
The results of the regression test for funnel plot asymmetry suggest that there is no statistically significant evidence of publication bias or funnel plot asymmetry in the meta-analysis. The p-value of 0.9564 indicates that the relationship between study precision SE and effect size is not significantly different from what would be expected by chance. In other words, the distribution of studies in the funnel plot appears to be symmetric and not skewed due to publication bias.
The limit estimate as SE approaches zero gives an estimate of the effect size under ideal conditions, if the studies had perfect precision. The point estimate of − 0.0491 suggests that, under these ideal conditions, the mean difference or effect size is approximately − 0.0491. However, the wide confidence interval (− 0.1117 to 0.0136) indicates substantial uncertainty in this estimate.
The results of the regression test for funnel plot asymmetry for CDR-SB
The results of the regression test for funnel plot asymmetry suggest that there is no statistically significant evidence of publication bias or funnel plot asymmetry in the meta-analysis. The p-value of 0.7808 indicates that the relationship between study precision SE and effect size is not significantly different from what would be expected by chance. In other words, the distribution of studies in the funnel plot appears to be symmetric and not skewed due to publication bias.
The limit estimate as SE approaches zero gives an estimate of the effect size under ideal conditions, assuming that the studies had perfect precision. The point estimate of − 0.5044 suggests that, under these ideal conditions, the mean difference or effect size is approximately − 0.5044. However, the wide confidence interval (− 1.0807 to 0.0719) indicates substantial uncertainty in this estimate.
The results of the regression test for funnel plot asymmetry for ADAS-cog14
The results of the regression test for funnel plot asymmetry suggest that there is no statistically significant evidence of publication bias or funnel plot asymmetry in the meta-analysis. The p-value of 0.8812 indicates that the relationship between study precision SE and effect size is not significantly different from what would be expected by chance. In other words, the distribution of studies in the funnel plot appears to be symmetric and not skewed due to publication bias.
The limit estimate as SE approaches zero gives an estimate of the effect size under ideal conditions, assuming that the studies had perfect precision. The point estimate of − 1.1020 suggests that, under these ideal conditions, the mean difference or effect size is approximately − 1.1020. However, the wide confidence interval (− 4.2541 to 2.0502) indicates substantial uncertainty in this estimate.
Variability and heterogeneity
The heterogeneity p-value is a statistical measure that helps assess whether there is significant variability in the effect sizes observed across different studies included in a meta-analysis. A low p-value (typically less than 0.05) suggests the presence of significant heterogeneity, indicating that the variation in effect sizes is not likely due to chance alone.
The Egger’s test p-value > 0.05 generally indicates no evidence of significant publication bias. The I2 value represents the proportion of total variability across studies due to heterogeneity.
These results suggest a lack of significant heterogeneity in the analyses related to ADCOMS Change, CDR-SB Change, and ADAS-cog14 Change, with I2 values of 0.0%. The Egger’s test for publication bias yielded non-significant results across all analyses, indicating a relatively consistent pattern in the findings without substantial publication bias. However, the high heterogeneity (I2 = 96.8%) and statistically significant p-value (< 0.0001) for the “Any TEAE Outcome” indicate substantial variability in the TEAE outcomes across the included studies this variability may be due to the huge difference in sample size between studies. This level of heterogeneity suggests that there might be differences in study populations, interventions, or methodologies that contribute to the observed variation in TEAE outcomes (Table 5).
Quality assessment
The quality of research design and reporting was assessed in several studies by Swanson et al., Logovinsky et al., Van Dyck et al., and Mcade et al. The analyzed studies present varying levels of bias across different domains. Swanson et al. and Logovinsky et al. have low risk of bias in multiple domains, particularly in terms of selection and performance. Van Dyck et al. demonstrate consistently low risk across all domains. On the other hand, Mcade et al. exhibit high risk in the selection and performance domains. Overall, domains such as selection and performance show lower bias across the studies, while attention to minimizing bias is warranted in domains such as detection and attrition, particularly in the study by Mcade et al. These findings indicate variations in the methodological rigor and potential bias in these studies (Fig. 5) (Table 6). For further details, please refer to Sect. 7 in the supplementary file.
Discussion
Our efficacy results in perspective to other literature
The examination of lecanemab at a dosage of 10 mg/kg versus a placebo reveals a substantial and statistically significant positive impact on ADCOMS, CDR-SB, and ADAS-cog14 scores in patients with Alzheimer’s disease (AD) (p < 0.0001). This discovery implies that administering lecanemab at this specific dose elicits a beneficial effect in terms of slowing the progression of the disease.
The validity of these results is further bolstered by the consistency observed across the studies. The narrow 95% confidence intervals, common effect model, and random effects model all estimate very similar mean differences. The absence of significant heterogeneity among the studies (p > 0.05) underscores the consensus in their findings.
The evidence from this meta-analysis strongly supports the idea that lecanemab at a dosage of 10 mg/kg, administered biweekly, leads to a significant reduction in the evaluated cognitive and functional scores in AD patients. These findings hold promise for the potential efficacy of lecanemab as a treatment option in this context.
The FDA granted accelerated approval to lecanemab (Leqembi) for Alzheimer’s disease, despite uncertainties about its impact on patients. This approval was based on phase 2 data indicating a reduction in amyloid β plaques in early-stage patients. Lecanemab, priced at $26,500 per patient per year, targets and removes Aβ aggregates associated with the disease [15]. While the phase 2 trial did not meet its 12-month primary endpoint, it showed reduced brain amyloid and consistent clinical improvement at 18 months [6]. Phase 3 results in the New England Journal of Medicine revealed reduced amyloid markers and moderately less cognitive and functional decline after 18 months with lecanemab compared to a placebo [12]. This accelerated approval allows the drug to be marketed before full effectiveness is proven.
A separate meta-analysis reinforces our results, demonstrating that lecanemab brings about statistically significant slower decline in cognition, functionality, and behavior among patients in the early stages of Alzheimer’s disease [16]. However, it is important to note that the methodology of this analysis is vague and still requires further investigation and clarification.
A systematic review and meta-analysis of randomized clinical trials conducted by Yue Qiao et al. found that lecanemab was beneficial to stabilize or slow down the decrease in CDR-SB, ADCOMS, and ADAS-cog in patients with early AD. The study also reported that lecanemab showed significant positive statistical efficacy with respect to cognition, function, and behavior in patients with early AD though the actual clinical significance is yet to be established [17].
One phase 3 trial has been initiated with the objective of validating the effectiveness and safety of lecanemab, the AHEAD trial (NCT04468659) for preclinical Alzheimer’s disease. The 18-month data from the phase 2 Study 201 were instrumental in properly powering the Clarity AD trial, which recently published positive preliminary results for a variety of robust outcomes [18].
While lecanemab did show a statistically significant reduction in the rate of cognitive decline, it may not necessarily translate to clinically meaningful changes, as indicated by published data on the Minimal Clinically Important Difference (MCID) and the opinions of certain clinical experts [19].
Lecanemab treatment was estimated to slow disease progression, extending the duration of mild cognitive impairment due to Alzheimer’s disease (MCI due to AD) and mild AD dementia while shortening the time to reach moderate and severe AD dementia. On average, it added 2.51, 3.13, and 2.34 years to the time to reach mild, moderate, and severe AD dementia, respectively. However, the model faces limitations: Mortality risk and patient utility data sources are uncertain. It solely focused on cognition’s indirect impact via CDR-SB, neglecting other severity domains and composite measures. Simulated population profiles might not accurately reflect those of Study 201. Severity projection leaned heavily on CDR-SB alone, with simplistic estimates for institutional care risk and patient utility [20].
Our safety results in perspective to other literature
Lecanemab at 10 mg/kg, administered biweekly, was assessed for its safety on three outcomes: The meta-analysis found no statistically significant difference in TEAE occurrence between lecanemab and placebo. The results were not conclusive and showed substantial variation among the studies. The analysis revealed a significant, increased risk of ARIA-E associated with lecanemab treatment at 10 mg/kg, administered biweekly, compared to placebo. This risk was consistent across studies.
Also indicated a notable, statistically significant increased risk of ARIA-H linked to lecanemab treatment at the same dosage (10 mg/kg) and frequency compared to placebo. This risk was consistent among the included studies and raises concerns about the safety of lecanemab, particularly regarding ARIA-H.
In certain studies, a risk ratio of 0 in the treatment group compared to the control group suggests no adverse events among treated patients. However, caution is needed due to the small sample size. Further research with larger cohorts is necessary to validate these findings and understand the clinical significance of the observed protective effect, which refers to a reduction in the risk or severity of adverse outcomes associated with a particular intervention or factor.
In both the phase 2 core and OLE studies, the occurrence of ARIA-E was infrequent, affecting less than 10% of participants, and symptomatic cases were below 3%. ARIA-E is typically presented as asymptomatic, mild to moderately severe, and manifested within the initial three months of treatment. The incidence of ARIA-E was associated with the highest concentration of lecanemab in the bloodstream and was more common in individuals who were homozygous carriers of apolipoprotein E4 (ApoE4). Notably, ARIA-H and ARIA-E had a similar occurrence rate in both the core and OLE phases of the study [21].
Subgroup analyses revealed that lecanemab had a more pronounced effect in slowing cognitive decline in individuals who are ApoE ε4 noncarriers compared to carriers and had the least impact on participants who were ApoE ε4 homozygotes. Since ApoE ε4 carriers are at a higher risk of experiencing ARIA, it is important to carefully consider the balance between benefits and potential harms for such patients [22].
In the base-case analysis, it resulted in an increase of 0.73 life years (LY) and 0.75 quality-adjusted LYs (QALY), with a reduction of 0.03 years in caregiver QALYs lost. The model also predicted a lower lifetime likelihood of institutional care admission for those receiving lecanemab alongside standard care (25% versus 31%) [20].
Results from the Cochrane risk of bias assessment
Evaluating research by Swanson, Logovinsky, Van Dyck, and Mcade uncovers differing levels of bias. Swanson and Logovinsky show minimal bias, particularly in selection and performance. Van Dyck consistently maintains low bias. In contrast, Mcade raises concerns with higher bias, particularly in selection and performance domains. In separate meta-analyses, they used the cochrane risk of bias tool. However, their results slightly differ from ours; they found unclear risk of bias in performance and detection, in contrast to our findings [16].
Future research recommendations
Suggest initiating comprehensive, long-term safety studies to enhance insights. Conduct comparative safety analyses, directly comparing lecanemab with established Alzheimer’s treatments like donepezil or rivastigmine. Collaboratively pinpoint specific risk factors and incorporate patient-reported outcomes for a thorough comprehension of lecanemab’s impact. Implement trials across diverse geographic locations and various ethnicities to ensure global efficacy and safety assessments.
Strengths and limitations
In our meta-analysis, we specifically emphasized the efficacy and safety of lecanemab at a dosage of 10 mg/kg—the same dose available on the market. Our focus was to address any inconsistencies in the findings among various trials, ensuring clarity regarding the drug’s performance. By concentrating on this specific dosage, we aimed to provide a comprehensive understanding of lecanemab’s safety and efficacy for consumers, thereby resolving potential conflicts in its profile across different studies.
We were compelled to compute the mean difference and standard error (SE) for the meta-analysis since the studies did not support the use of standard deviation (SD). We reached out to Eisai Company to request this information, but they responded that they would discuss the matter and provide a decision. Unfortunately, we did not receive any further communication from them. In the case of the study by Mcade et al., we had to estimate the SE by imputing data from other studies due to insufficient information for SE calculation.
There are inconsistencies between the Prospero registration and the full text. In the registration, we stated that studies in languages other than English would be excluded, but we discovered four studies without English translations, all of which were either irrelevant or mere reviews. Additionally, we planned to assess the mini-mental state examination (MMSE) and positron emission tomography standardized uptake value ratio (PET SUVr), but the available data proved insufficient.
Conclusion
The lack of notable heterogeneity, except for a significant heterogeneity observed in the case of TEAE with an I2 of 96.8%, underscores the reliability of the efficacy results. The consistent outcomes across the studies affirm the dependability of the findings. The meta-analysis indicates that administering lecanemab at a dosage of 10 mg/kg biweekly is linked to a positive impact on enhancing cognitive outcomes measured across various parameters in individuals with AD. These results provide valuable insights into the potential effectiveness of lecanemab as a therapeutic intervention for addressing cognitive impairment in this patient population.
While no strong evidence supports a significant difference in the occurrence of TEAE, the meta-analysis raises substantial safety concerns related to the increased risk of ARIA-E and ARIA-H associated with lecanemab at a dosage of 10 mg/kg administered biweekly when compared to placebo. These findings, particularly the elevated risk of ARIA-H, highlight the need for careful consideration and monitoring of the safety profile of lecanemab in clinical practice.
Data availability
All data generated or analyzed during this study are included in this published article (and its supplementary information file).
References
Scheltens P, Blennow K, Breteler MM, de Strooper B, Frisoni GB, Salloway S et al (2016) Alzheimer’s disease. Lancet 388:505–517
Golde TE (2022) Disease-modifying therapies for Alzheimer’s disease: more questions than answers. Neurotherapeutics 19:209–227
Prince M, Ali GC, Guerchet M, Prina AM, Albanese E, Wu YT (2016) Recent global trends in the prevalence and incidence of dementia, and survival with dementia. Alzheimers Res Ther 8:23
Swanson CJ, Zhang Y, Dhadda S, Wang J, Kaplow J, Lai RYK et al (2021) A randomized, double-blind, phase 2b proof-of-concept clinical trial in early Alzheimer’s disease with lecanemab, an anti-Aβ protofibril antibody. Alzheimers Res Ther 13:80
Reish NJ, Jamshidi P, Stamm B, Flanagan ME, Sugg E, Tang M et al (2023) Multiple cerebral hemorrhages in a patient receiving lecanemab and treated with t-PA for stroke. N Engl J Med 388:478–479
McDade E, Cummings JL, Dhadda S, Swanson CJ, Reyderman L, Kanekiyo M et al (2022) Lecanemab in patients with early Alzheimer’s disease: detailed results on biomarker, cognitive, and clinical effects from the randomized and open-label extension of the phase 2 proof-of-concept study. Alzheimers Res Ther 14:191
Schindler SE, Bollinger JG, Ovod V, Mawuenyega KG, Li Y, Gordon BA et al (2019) High-precision plasma β-amyloid 42/40 predicts current and future brain amyloidosis. Neurology 93:e1647–e1659
Li Y, Schindler SE, Bollinger JG, Ovod V, Mawuenyega KG, Weiner MW et al (2022) Validation of plasma amyloid-β 42/40 for detecting Alzheimer disease amyloid plaques. Neurology 98:e688–e699
Shcherbinin S, Evans CD, Lu M, Andersen SW, Pontecorvo MJ, Willis BA et al (2022) Association of amyloid reduction after donanemab treatment with tau pathology and clinical outcomes: the TRAILBLAZER-ALZ randomized clinical trial. JAMA Neurol 79:1015–1024
Cummings J, Apostolova L, Rabinovici GD, Atri A, Aisen P, Greenberg S et al (2023) Lecanemab: appropriate use recommendations. J Prev Alzheimer’s Dis 10:362–377
Reardon S (2023) FDA approves Alzheimer’s drug lecanemab amid safety concerns. Nature
van Dyck CH, Swanson CJ, Aisen P, Bateman RJ, Chen C, Gee M et al (2022) Lecanemab in early Alzheimer’s disease. N Engl J Med 388:9–21
Logovinsky V, Satlin A, Lai R, Swanson C, Kaplow J, Osswald G et al (2016) Safety and tolerability of BAN2401–a clinical study in Alzheimer’s disease with a protofibril selective Aβ antibody. Alzheimers Res Ther 8:14
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Elisabeth M (2023) Alzheimer’s disease: FDA approves lecanemab amid cost and safety concerns. BMJ 380:p73
Qiao Y, Chi Y, Zhang Q, Ma Y (2023) Safety and efficacy of lecanemab for Alzheimer’s disease: a systematic review and meta-analysis of randomized clinical trials. Front Aging Neurosci 15:1169499
Iwatsubo T (2023) Clinical implementation of lecanemab: challenges, questions and solutions. J Prev Alzheimer’s Dis 10:353–355
Dhadda S, Kanekiyo M, Li D, Swanson CJ, Irizarry M, Berry S et al (2022) Consistency of efficacy results across various clinical measures and statistical methods in the lecanemab phase 2 trial of early Alzheimer’s disease. Alzheimer’s Res Ther 14:182
Lansdall CJ, McDougall F, Butler LM, Delmar P, Pross N, Qin S et al (2023) Establishing clinically meaningful change on outcome assessments frequently used in trials of mild cognitive impairment due to Alzheimer’s disease. J Prev Alzheimer’s Dis 10:9–18
Tahami Monfared AA, Tafazzoli A, Ye W, Chavan A, Zhang Q (2022) Long-term health outcomes of lecanemab in patients with early Alzheimer’s disease using simulation modeling. Neurol Ther 11:863–880
Honig LS, Barakos J, Dhadda S, Kanekiyo M, Reyderman L, Irizarry M et al (2023) ARIA in patients treated with lecanemab (BAN2401) in a phase 2 study in early Alzheimer’s disease. Alzheimers Dement (N Y) 9:e12377
Wright AC, Lin GA, Whittington MD, Agboola F, Herron-Smith S, Rind D et al (2023) The effectiveness and value of lecanemab for early Alzheimer disease: a summary from the Institute for Clinical and Economic Review’s California Technology Assessment Forum. J Manag Care Spec Pharm 29:1078–1083
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
K.A. started with the conceptualization of the study. K.A. and H. A designed and planned the study. The retrieval and screening of studies were handled by K.A. and A.A.A. and cross-checked by K.A. and B.A. K.A., A.A.A., and B.A. were responsible for data collection and analysis. All authors contributed to the data interpretation and research conclusions. The manuscript was written by K.A. A.A.A., B.A., HA, and A.I.E. with critical input from all authors.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdelazim, K., Allam, A.A., Afifi, B. et al. The efficacy and safety of lecanemab 10 mg/kg biweekly compared to a placebo in patients with Alzheimer’s disease: a systematic review and meta-analysis of randomized controlled trials. Neurol Sci 45, 3583–3597 (2024). https://doi.org/10.1007/s10072-024-07477-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-024-07477-w