Abstract
Objective
Aneurysmal subarachnoid hemorrhage (aSAH) is an aggressive disease with higher mortality rate in the elderly population. Unfortunately, the previous models for predicting clinical prognosis are still not accurate enough. Therefore, we aimed to construct and validate a visualized nomogram model to predict online the 3-month mortality in elderly aSAH patients undergoing endovascular coiling.
Method
We conducted a retrospective analysis of 209 elderly aSAH patients at People’s Hospital of Hunan Province, China. A nomogram was developed based on multivariate logistic regression and forward stepwise regression analysis, then validated using the bootstrap validation method (n = 1000). In addition, the performance of the nomogram was evaluated by various indicators to prove its clinical value.
Result
Morbid pupillary reflex, age, and using a breathing machine were independent predictors of 3-month mortality. The AUC of the nomogram was 0.901 (95% CI: 0.853–0.950), and the Hosmer–Lemeshow goodness-of-fit test showed good calibration of the nomogram (p = 0.4328). Besides, the bootstrap validation method internally validated the nomogram with an area under the curve of the receiver operator characteristic (AUROC) of 0.896 (95% CI: 0.846–0.945). Decision curve analysis (DCA) and clinical impact curve (CIC) indicated the nomogram’s excellent clinical utility and applicability.
Conclusion
An easily applied visualized nomogram model named MAC (morbid pupillary reflex-age-breathing machine) based on three accessible factors has been successfully developed. The MAC nomogram is an accurate and complementary tool to support individualized decision-making and emphasizes that patients with higher risk of mortality may require closer monitoring. Furthermore, a web-based online version of the risk calculator would greatly contribute to the spread of the model in this field.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aneurysmal subarachnoid hemorrhage (aSAH) is a relatively rare but severely aggressive disease that leads to a tremendous mortality rate, with approximately one-third of patients not surviving, particularly in elderly patients [1,2,3]. As the treatment of choice for ruptured aneurysms, endovascular coiling has been used to a growing extent because of the ability to yield less symptomatic vasospasm and a higher rate of disability-free survival [4, 5]. However, As with neurosurgical clipping of the aneurysm, undergoing coil embolization is also followed by complications associated with a decline in postoperative Glasgow Coma Scale (GCS) scores, such as thromboembolic events, which could contribute to poor neurological outcomes [6]. Therefore, it is significant to predict the mortality after aSAH in elderly patients who underwent coiling early to support.
Despite the promising results of conventional prediction models, such as the prognostic model based on the ISAT database, the ffANN prediction model and the HHPA model [4, 7,8,9,10], each has one or more weaknesses. In summary, the main limitation of its application in clinical practice is that the risk factors allowing prediction of individual patients are not ideal, most of them including variables that are difficult to define objectively or are not easily obtained at admission and rely on the results of clinical neurological examinations. In addition, compared to younger patients, older patients are more likely to have preexisting conditions such as hypertension and diabetes, which makes intracranial SAH susceptible, so they are more likely to develop complications including hydrocephalus and rebleeding after aASH, leading to a poorer prognosis [11,12,13,14]. Hence, previous models based on the overall population cannot be extrapolated to predict the case-fatality of elderly subgroups accurately.
The nomogram is a visual graphical statistical tool incorporating many variables to develop a continuous scoring system that reflects the individual and precise risk probability. As an important decision-making tool in modern medicine, the nomogram allows rapid prognostic prediction based on selected clinical parameters and has been widely applied in predicting outcomes, including cancer, surgery, and COVID-19 [15,16,17].
Therefore, this study has developed a visualized nomogram model based on the limited number of readily available impact factors, which can be individually used to predict the mortality of 3 months in Chinese elderly aSAH patients who have undergone endovascular coiling.
Methods
Study population
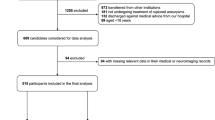
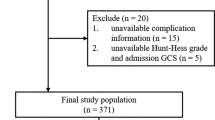
In this retrospective study, we collected elderly patients admitted to the People’s Hospital of Hunan Province for aSAH from January 2016 to June 2021. The eligibility criteria in this study were as follows: (1) age ≥ 65 years; (2) patients with intracranial saccular aneurysms who underwent specialized endovascular coil embolization; (3) intracranial aneurysms were diagnosed by computed tomography (CT) angiography or digital subtraction angiography (DSA); (4) patient survival until completion of the main treatment. Exclusion criteria included the followings: (1) more than 3 days from attack to admission; (2) with blood blister-like, fusiform, or dissecting aneurysms; (3) with other complications which seriously affect the prognosis of disease, such as carcinoma of the pancreas; (4) withdrew from the medical care due to economic factors or other reasons. All aSAH patients included in this study were treated with routine SAH treatment, and the clinical team also underwent uniform, highly standardized training. We excluded variables with more than 20% missing values and patients with missing features for further analysis. The Ethics Committee approved the present study of Hunan Provincial People’s Hospital, and the Ethics Committee waived the requirement of written informed consent for participation.
Demographic and clinical factors
We reviewed baseline characteristics of the elderly patients, which were recorded on admission, including demographic characteristics, such as age and sex; medical histories, such as hypertension and diabetes mellitus; smoking; drinking; baseline data, such as creatinine and fasting blood glucose (FBG); radiological variables, such as size and location of the aneurysm, as well as the modified Fisher scale; and clinical assessment on admissions, such as the Hunt and Hess score (H&H) and the World Federation of Neurological Surgeons (WFNS) grade. We also collected in-hospital treatment, such as preoperative using anticoagulant drugs, intraoperative using tirofiban and a breathing machine (referring to continuous invasive mechanical ventilation after endovascular treatment), dexmedetomidine, and other sedatives for multimodal analgesia in the procedure). Besides, complications such as hydrocephalus, cerebral infarction, intracranial infection, and rebleeding (a sudden clinical deterioration with signs of increased hemorrhage on consecutive CT scans) were gathered. The data mentioned above were collected by clinicians that are well-versed in the SAH patient journey to reduce the admission of incorrect data.
Patient outcome
The patient outcome of our study was death in 3 months, defined as a 3-month modified Rankin Score (mRS) of 6. Thus, according to mRS, the primary outcomes of elderly patients at 3 months were divided into the non-death group (mRS < 6) and the death (mRS = 6) group.
Statistical analysis
First, the Shapiro–Wilk test was used to confirm whether the continuous data followed a normal distribution. Next, continuous variables were described as mean ± standard deviation or median value with an interquartile range; categorical variables were reported as the number of events and the proportion of events occurring. Finally, differences between the two groups were assessed using the t-test or Mann–Whitney U-test for continuous variables and the χ2-test or Fisher’s exact test for categorical variables.
Variable selection and construction of nomogram
A nomogram model was generated to predict the probability of a 3-month unfavorable outcome. All variables with a probability value < 0.05 and traditionally considered risk factors of the unfavorable outcome were entered into a logistic regression model to generate the nomogram. Moreover, a forward stepwise regression was carried out to confirm the final variables composing the nomogram model. To enhance the predictive performance, we estimated the multicollinearity of the selected variables using the variance inflation factor (VIF), and VIF < 5 was considered non-significant. Probability values < 0.05 were considered statistically significant in the above steps. Finally, we calculated the regression coefficients and odds ratios (OR) with two-sided 95% confidence intervals (95% CIs) of each variable found to be significantly associated with unfavorable outcomes.
Validation of nomogram
Model performance was assessed by discrimination and calibration. Discrimination of the model is the ability to separate patients with an unfavorable versus favorable outcome, and calibration is the ability to predict the actual outcome in patients. The area under the curve of the receiver operator characteristic (AUROC) with a corresponding 95% CI was used to quantify discrimination of the nomogram model, and we used Hosmer–Lemeshow test to assess calibration. When the model’s predictive value matches the patient’s actual risk, a 45° line indicates perfect calibration. In order to prevent the overfitting bias, we also conducted an internally validated nomogram through the bootstrap validation method (n = 1000).
The statistical analysis was conducted using SPSS version 25.0 (IBM Corporation, Armonk, NY, USA) statistical software, and the software package R (version 4.1.3, R Development Core Team, Auckland, New Zealand) was used for model visualization.
Results
Clinical characteristics
In this study, 213 patients with aneurysmal subarachnoid hemorrhage enrolled in our study; after excluding four patients with missing variables, 209 patients were included in the final dataset. The cohort’s median age was 70 (interquartile range: 68–74) years, and 27.8% (58) were men. According to the clinical outcome, 169 patients (80.9%) were in the non-death group (median age: 70 years; number of male patients: 48), and 40 patients (19.1%) were in the death group (median age: 73 years; number of male patients: 10).
Variable selection
Table 1 shows patients’ clinical, demographic, and laboratory characteristics in the non-death and death groups. Age, systolic blood pressure (SBP), diastolic blood pressure (DBP), FBG, white blood cell count (WBC), neutrophil to lymphocyte ratio (NLR), lymphocyte to monocyte ratio (LMR), systemic inflammatory response index (SIRI), systemic immune-inflammation (SII), aspartate transaminase (AST), D-dimer, fibrinogen degradation product (FDP), lactate dehydrogenase (LDH), Fisher scale, multiple aneurysms, external ventricular drainage (EVD), complicated with cerebral infarction, symptomatic cerebral vasospasm, complicated with pulmonary infection, using a breathing machine, ventricular hematocele, complicated with cerebral hemorrhage, rebleeding, and pupillary reflex were found to be significant in the univariate analysis.
Twenty-seven variables (including traditional prognostic risk factors such as size and position of the aneurysm, H&H) entered the multivariate analysis. After multivariate analysis and forward stepwise regression analysis, age (OR: 1.090, 95% CI: 1.004–1.189, p = 0.045), using a breathing machine (OR: 5.689, 95% CI: 2.074–16.072, p < 0.001), and pupillary reflex (OR: 8.072, 95% CI: 2.858–24.381, p < 0.001) remained independent predictors of 3-month death and finally entered into a logistic regression model to construct the nomogram to predict the probability of 3-month death in elderly cohort with aSAH who received endovascular coil embolization (Table 2). The nomogram is shown in Fig. 1. No significant statistical collinearity was observed for all of the variables we selected.
Construction of visualized online nomogram
We presented the predictive model as a nomogram by distributing a preliminary graphic score to each independent predictor with a point range from 0 to 100. The total point is then summed by all points assigned to each predictor. Finally, we can acquire the probability of 3-month death by converting the total point. To make the prediction model more user-friendly, we also constructed the visualized nomogram for convenience, and the nomogram page is shown in Fig. 2. A free online calculator is accessible for all clinicians and patients at https://macnomogram.shinyapps.io/dynnomapp/. Then, the information on predictive prognosis can be acquired easily by choosing the characteristics of each patient on the interface of the website. This web-based tool can be used for more precise calculations. Additionally, it also reports 95% prediction intervals. Moreover, to achieve the effect of forecasting on mobile phones anytime and anywhere, as well as make the prediction model more widely used, we further converted the website into a two-dimensional code (Fig. 3).
Validation of nomogram
The AUROC of the nomogram was 0.901 (95% CI: 0.853–0.950) in the cohort (Fig. 4), which showed good discrimination of the nomogram. Furthermore, the calibration curve showed that the predicted value of the nomogram was in agreement with the observed outcome (Fig. 5). The Hosmer–Lemeshow goodness-of-fit test showed good calibration of the nomogram (p = 0.4328). The characteristics of the nomogram, such as sensitivity, accuracy, and positive predictive value (PPV), are shown in Table 3. The results of DCA showed that using the nomogram to predict a 3-month unfavorable outcome would generate more net benefit than the “treat all” or “treat none” strategies when the threshold probabilities ranged from 5 to 62% (Fig. 6). The CIC visually showed the estimated number of high-risk patients predicted by the nomogram and actual numbers for each risk threshold (Fig. 7). For example, if a 20% risk thresholds were used, 1000 patients would be screened, 290 patients would be predicted as being high risk, but about 190 patients were high risk. Moreover, according to the bootstrap validation method, the nomogram was internally validated with an AUROC of 0.896 (95% CI: 0.846–0.945) and proved the accuracy of predictive ability.
Calibration curve of the nomogram. The x-axis represents the nomogram-predicted probability, and the y-axis represents the actual probability of 3-month mortality. The 45° dashed line is a reference line that shows perfect prediction. The dotted line is the performance of the nomogram, while the solid line corrects for any bias in the nomogram
Discussion
Based on a study of a cohort of elderly aSAH patients undergoing endovascular coiling, we performed multivariate logistic regression analysis and found that older age, morbid pupillary reflex, and ventilated breathing status were independently associated with 3-month mortality outcome as well as successfully developed a predictive model named MAC with an AUROC curve of 0.901.
To begin with, one of the strengths of our model is its excellent predictive performance and the fact that predictions can be accessed visually through the network. On the one hand, as expected, the MAC nomogram with the three indicators mentioned above attained an eximious sensitivity of 92.5%, and specificity of 82.2%, whereas several models show a significant imbalance in prediction sensitivity and specificity. In addition, the negative predictive values of our model achieved 97.9%, indicating that, to a large extent, the MAC nomogram can correctly identify who is more likely to survive after 3 months of coiling in elderly patients. On the other hand, a web-based risk calculator has also been developed. With this visualization tool, clinicians will be able to access prediction results online in a more intuitive way, identifying patients at high risk of severe poor outcomes or even death after embolization, which facilitates the application of predictive models in the clinical setting and has a potential role in the more reasonable allocation of medical resources and personalized medical care treatment.
A further advantage of our model is that it is constructed using objective, simple, and readily available clinical information as risk factors. Compared to the ABC score and the HAIR score [18, 19], the MAC model developed in this study eliminates the need to consider numerous biologically characteristic indicators, such as troponin and S100β at admission, making it easier for clinicians to follow and generalize, and saving costs in patient care. Moreover, risk stratification can be intuitively performed through the risk probability displayed in the visualized online nomogram, reducing unnecessary waste of healthcare resources. For example, the nomogram assigns about a 90% probability of death in an aSAH patient aged 88 years (80 points) after endovascular coiling, which is using a breathing machine (72 points), with morbid pupillary reflex (85 points), and then, the total score of the patient is 237 points. On the contrary, a chance of approximately 5% probability of death is indicated for a patient who is 75 years old (33 points) and does not use a breathing machine (0 points), with normal pupillary reflex (0 points), and the total score is 33 points.
Most of the collected data were recorded through a manual review of medical records, and eligible patients were screened using strictly objective unified inclusion and exclusion criteria. The incidence and mortality rate of aSAH patients in the study were generally in line with the reports from other researchers [20,21,22], indicating that our patient cohort generally reflects the approximate status of the real world and confirming the scientific value of the MAC model. Thus, we envisage that this predictive tool, which can be used to identify the risk of death 3 months after coiling in elderly patients, will be helpful to clinicians in making more timely and beneficial decisions in postoperative management. This is also the third and, simultaneously, the most significant strength of this study.
Collectively, the pathophysiological status of patients after aSAH is complex and variable, and there are many factors associated with the clinical outcome after aSAH. First of all, it is not surprising to observe from the results of this study that elderly patients are more likely to die in the short term. Similarly, increasing age has consistently been an independent predictor of poor prognosis, as previously reported in related fields of study [2, 14, 23,24,25,26]. The incidence of aSAH is positively correlated with increasing age due to the multiple clinical complications and vascular risk factors in elderly patients [11, 14]. Regardless of the treatment choice, older patients tend to have a worse prognosis and an abrupt decline in survival following ruptured intracranial aneurysm bleeding. However, early intervention and aggressive care for them have been demonstrated to improve survival rates significantly [27], suggesting that clinicians should pay more attention to the postoperative management of the patients. Secondly, the morbid pupillary reflex, including unilateral or bilateral unresponsive dilated pupils or anisocoria (pupil size asymmetries), strongly predicts mortality in patients. When the pupils are dilated, it often means an irreversible late event. Many studies have confirmed that abnormal pupillary responses are an early indicator of increased intracranial pressure (ICP), often in patients with severe traumatic brain injury (TBI), aSAH, or intracerebral hemorrhage (ICH), and may reflect neurological recuperation [28,29,30,31]. Also, in a study of poor-grade aSAH patients, Mack et al. concluded that pupillary response is more sensitive and specific than H&H as a reliable predictor of prognosis in patients [32]. Therefore, it is possible to predict the prognosis for survival and minimize the incidence of unfavorable outcomes by observing the normal light reactivity of the pupils. Furthermore, based on the clinical experience given by neurosurgeons, there is clear evidence that patients who undergo prompt intervention once pupillary abnormalities are present have more potential for favorable outcomes. Thirdly, the worse the neurological system, the greater the need for prolonged use of a breathing machine. However, while the use of breathing machines could reflect the disease severity, it can also potentially contribute to prognostic outcomes directly. In ventilated patients, blood oxygen levels tend to fluctuate according to the adjustment of ventilator parameters, and lower than normal blood oxygen levels or hypoxemia may exacerbate cerebral ischemia to worsen the illness [33]. As well, invasive mechanical ventilation can induce additional injuries including infectious complications, acute kidney injury, gastrointestinal bleeding, and perioral pressure ulcers [34,35,36]. In particular, several studies have mentioned nosocomial pneumonia, and hyperventilation can result in hypocapnia [37, 38]. A retrospective study found that hypocapnia increases the risk of symptomatic vasospasm and is independently associated with poor functional outcomes and delayed cerebral ischemia (DCI) [39]. Nevertheless, more research data suggest that most patients with aSAH show a higher mortality rate without ventilators [40,41,42]. Consequently, there is necessary to select the use of ventilators for elderly patients. If some patients recover well, excessive interventions, such as prolonged use of breathing machines, should be avoided. Finally, although some scales, such as WFNS grade, H&H, and modified Fisher grading scale, were not included in our MAC model, the performance of our nomogram model did not degrade due to the inclusion of the three variables mentioned above and the superior data handling capabilities of the nomogram model. In this regard, the following explanations are given. (i) If the patients were intubated or sedated, assessing the clinical grading correctly at admission was impossible. As a result, the various scoring scales are prone to potential misclassification [2, 43]. (ii) The scores are not predictors of mortality but rather markers of the overall patient complexity. Therefore, using such scoring scales alone or their inclusion in the model does not necessarily predict morbidity and mortality more accurately. This is also confirmed by comparison with the results of previous studies, where the HHPA model had a lower AUC of 0.841 than our model of 0.901 [10]. (iii) The subjective variability between observers when grading patients on the basis of CT findings may also hamper the utility of scoring scales [44, 45]. Moreover, some of the findings for the whole population refer to radiological features, such as aneurysm lumen size and intraventricular hemorrhage, as predictors of mortality outcome [7, 19, 46,47,48], while data on these features were also collected in our study. However, due to the fact that advanced age itself is strongly associated with many traditional factors, prognostic factors in the elderly subgroup may become quite limited, and rebleeding may not be easily detected objectively. Hence, the above variables are not optimal predictors of mortality in those aged ≥ 65 years and ultimately do not exist in our model.
Nonetheless, several limitations have to be taken into consideration seriously. Firstly, the results of the present study are based on single-center data and relate only to the Chinese elderly population, which may be less effective than expected when applied to other subgroups. However, all patients enrolled in the study underwent highly standardized clinical management, allowing the model to be more generalizable. Furthermore, the inclusion of only elderly patients definitively treated with endovascular coiling resulted in a small sample size, which may not capture all variables potentially affecting the outcomes. Therefore, the external validity of the model remains to be determined and needs to be tested in a larger, ideally independent cohort. In addition, the inherent weaknesses of retrospective studies are one of the limitations of our study. We cannot rule out the “self-fulfilling prophecy” that could be achieved by withdrawing from active postoperative hospital care. Patients with a poor prognosis, especially older ones, are more likely to undergo withdrawal therapy or abandon further treatment, in other words, to adopt “self-fulfilling” management practices. This may ultimately affect the accuracy of the model in predicting the population. Finally, we analyzed prognostic outcomes at 3 months for just elderly patients, while long-term case fatality could not be assessed.
In summary, our model cannot replace the clinical diagnosis of surgical specialists with long experience. Nevertheless, we found that the MAC nomogram has good discriminatory and calibrated properties in predicting mortality and may be potentially superior to other models developed in previous studies in Chinese elderly patients.
Conclusion
In this study, we found that high mortality after aSAH was associated with using a breathing machine, the patient’s age, and the presence of morbid pupillary reflex. This allowed us to successfully develop an easily applied visualized prediction model named MAC (morbid pupillary reflex-age-breathing machine), the nomogram, and an online risk calculator that can be used to accurately identify Chinese elderly patients with a high probability of death 3 months after undergoing endovascular coiling. These patients will likely benefit from individualized decision-making on postoperative interventions and closer clinical monitoring to reduce mortality risk. In the future, we will perform external validation in other independent cohorts to enhance the robustness of the model.
Data availability
The datasets analyzed during the current study are available from the corresponding authors on reasonable request.
Change history
16 May 2023
A Correction to this paper has been published: https://doi.org/10.1007/s10072-023-06856-z
Abbreviations
- aSAH :
-
Aneurysmal subarachnoid hemorrhage
- AUC :
-
Area under the curve
- AUROC :
-
Area under the receiver operating characteristic curve
- DCA :
-
Decision curve analysis
- CIC :
-
Clinical impact curve
- GCS :
-
Glasgow Coma Scale
- SAH :
-
Subarachnoid hemorrhage
- FBG :
-
Fasting blood glucose
- H&H :
-
Hunt and Hess score
- WFNS :
-
World Federation of Neurosurgical Societies
- mRS :
-
Modified Rankin Score
- VIF :
-
Variance inflation factor
- 95% CIs :
-
95% Confidence intervals
- OR :
-
Odds ratios
- SBP :
-
Systolic blood pressure
- DBP :
-
Diastolic blood pressure
- WBC :
-
White blood cell count
- NLR :
-
Neutrophil to lymphocyte ratio
- LMR :
-
Lymphocyte to monocyte ratio
- SIRI :
-
Systemic inflammatory response index
- SII :
-
Systemic immune-inflammation
- AST :
-
Aspartate transaminase
- FDP :
-
Fibrinogen degradation product
- LDH :
-
Lactate dehydrogenase
- EVD :
-
External ventricular drainage
- PPV :
-
Positive predictive value
- ICP :
-
Intracranial pressure
- TBI :
-
Traumatic brain injury
- ICH :
-
Intracerebral hemorrhage
- DCI :
-
Delayed cerebral infarction
References
Jaja B, Saposnik G, Lingsma HF et al (2018) Development and validation of outcome prediction models for aneurysmal subarachnoid haemorrhage: the SAHIT multinational cohort study. BMJ 360:j5745. https://doi.org/10.1136/bmj.j5745
Goldberg J, Schoeni D, Mordasini P et al (2018) Survival and outcome after poor-grade aneurysmal subarachnoid hemorrhage in elderly patients. Stroke 49:2883–2889. https://doi.org/10.1161/STROKEAHA.118.022869
Shimamura N, Naraoka M, Katagai T et al (2016) Analysis of factors that influence long-term independent living for elderly subarachnoid hemorrhage patients. World Neurosurgery 90:504–510. https://doi.org/10.1016/j.wneu.2016.03.057
Molyneux A, Kerr R, Stratton I et al (2002) International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet 360:1267–1274. https://doi.org/10.1016/s0140-6736(02)11314-6
Wilson TJ, Davis MC, Stetler WR et al (2014) Endovascular treatment for aneurysmal subarachnoid hemorrhage in the ninth decade of life and beyond. J Neurointerv Surg 6:175–177. https://doi.org/10.1136/neurintsurg-2013-010714
Ayling OGS, Ibrahim GM, Drake B et al (2015) Operative complications and differences in outcome after clipping and coiling of ruptured intracranial aneurysms. J Neurosurg 123:621–628. https://doi.org/10.3171/2014.11.JNS141607
Risselada R, Lingsma HF, Bauer-Mehren A et al (2010) Prediction of 60 day case-fatality after aneurysmal subarachnoid haemorrhage: results from the International Subarachnoid Aneurysm Trial (ISAT). Eur J Epidemiol 25:261–266. https://doi.org/10.1007/s10654-010-9432-x
Dijkland S, Roozenbeek B, Brouwer P et al (2015) Prediction of 60-day case fatality after aneurysmal subarachnoid hemorrhage: external validation of a prediction model. Crit Care 19:P467. https://doi.org/10.1186/cc14547
de Jong G, Aquarius R, Sanaan B et al (2021) Prediction models in aneurysmal subarachnoid hemorrhage: forecasting clinical outcome with artificial intelligence. Neurosurg 88:E427–E434. https://doi.org/10.1093/neuros/nyaa581
Mader MM, Piffko A, Dengler NF et al (2020) Initial pupil status is a strong predictor for in-hospital mortality after aneurysmal subarachnoid hemorrhage. Sci Rep 10:4764. https://doi.org/10.1038/s41598-020-61513-1
Park J, Woo H, Kang D-H, Kim Y (2014) Critical age affecting 1-year functional outcome in elderly patients aged ≥ 70 years with aneurysmal subarachnoid hemorrhage. Acta Neurochir 156:1655–1661. https://doi.org/10.1007/s00701-014-2133-6
Kanamaru H, Kawakita F, Asada R et al (2020) Prognostic factors varying with age in patients with aneurysmal subarachnoid hemorrhage. J Clin Neurosci 76:118–125. https://doi.org/10.1016/j.jocn.2020.04.022
Lanzino G, Kassell NF, Germanson TP et al (1996) Age and outcome after aneurysmal subarachnoid hemorrhage: why do older patients fare worse? J Neurosurg 85:410–418. https://doi.org/10.3171/jns.1996.85.3.0410
Maeda T, Satow T, Ikeda G et al (2020) Clinical outcome of elderly patients with subarachnoid hemorrhage: validation of modality assignment based on aneurysmal morphology and location. World Neurosurgery 143:e419–e429. https://doi.org/10.1016/j.wneu.2020.07.189
Iasonos A, Schrag D, Raj GV, Panageas KS (2008) How to build and interpret a nomogram for cancer prognosis. J Clin Oncol 26:1364–1370. https://doi.org/10.1200/JCO.2007.12.9791
Balachandran VP, Gonen M, Smith JJ, DeMatteo RP (2015) Nomograms in oncology: more than meets the eye. Lancet Oncol 16:e173–e180. https://doi.org/10.1016/S1470-2045(14)71116-7
Liu L, Xie J, Wu W et al (2021) A simple nomogram for predicting failure of non-invasive respiratory strategies in adults with COVID-19: a retrospective multicentre study. Lancet Digit Health 3:e166–e174. https://doi.org/10.1016/S2589-7500(20)30316-2
Degos V, Apfel CC, Sanchez P et al (2012) An admission bioclinical score to predict 1-year outcomes in patients undergoing aneurysm coiling. Stroke 43:1253–1259. https://doi.org/10.1161/STROKEAHA.111.638197
Lee VH, Ouyang B, John S et al (2014) Risk stratification for the in-hospital mortality in subarachnoid hemorrhage: the HAIR Score. Neurocrit Care 21:14–19. https://doi.org/10.1007/s12028-013-9952-9
Etminan N, Chang H-S, Hackenberg K et al (2019) Worldwide incidence of aneurysmal subarachnoid hemorrhage according to region, time period, blood pressure, and smoking prevalence in the population: a systematic review and meta-analysis. JAMA Neurol 76:588. https://doi.org/10.1001/jamaneurol.2019.0006
Hammer A, Ranaie G, Yakubov E et al (2020) Dynamics of outcome after aneurysmal subarachnoid hemorrhage. Aging 12:7207–7217. https://doi.org/10.18632/aging.103069
Roquer J, Cuadrado-Godia E, Guimaraens L et al (2020) Short- and long-term outcome of patients with aneurysmal subarachnoid hemorrhage. Neurology 95:e1819–e1829. https://doi.org/10.1212/WNL.0000000000010618
Yue Q, Liu Y, Leng B et al (2016) A prognostic model for early post-treatment outcome of elderly patients with aneurysmal subarachnoid hemorrhage. World Neurosurgery 95:253–261. https://doi.org/10.1016/j.wneu.2016.08.020
Virta JJ, Satopää J, Luostarinen T, Raj R (2020) One-year outcome after aneurysmal subarachnoid hemorrhage in elderly patients. World Neurosurgery 143:e334–e343. https://doi.org/10.1016/j.wneu.2020.07.127
Wilson TJ, Davis MC, Stetler WR et al (2014) Endovascular treatment for aneurysmal subarachnoid hemorrhage in the ninth decade of life and beyond. J NeuroIntervent Surg 6:175–177. https://doi.org/10.1136/neurintsurg-2013-010714
Naval NS, Kowalski RG, Chang TR et al (2014) The SAH Score: a comprehensive communication tool. J Stroke Cerebrovasc Dis 23:902–909. https://doi.org/10.1016/j.jstrokecerebrovasdis.2013.07.035
Al-Mufti F, Mayer SA, Kaur G et al (2021) Neurocritical care management of poor-grade subarachnoid hemorrhage: unjustified nihilism to reasonable optimism. Neuroradiol J 34:542–551. https://doi.org/10.1177/19714009211024633
Chen J, Gombart Z, Rogers S et al (2011) Pupillary reactivity as an early indicator of increased intracranial pressure: the introduction of the neurological pupil index. Surg Neurol Int 2:82. https://doi.org/10.4103/2152-7806.82248
Brennan PM, Murray GD, Teasdale GM (2018) Simplifying the use of prognostic information in traumatic brain injury. Part 1: the GCS-Pupils score: an extended index of clinical severity. J Neurosurg 128:1612–1620. https://doi.org/10.3171/2017.12.JNS172780
Marmarou A, Lu J, Butcher I et al (2007) Prognostic value of the Glasgow Coma Scale and pupil reactivity in traumatic brain injury assessed pre-hospital and on enrollment: an IMPACT analysis. J Neurotrauma 24:270–280. https://doi.org/10.1089/neu.2006.0029
Clusmann H, Schaller C, Schramm J (2001) Fixed and dilated pupils after trauma, stroke, and previous intracranial surgery: management and outcome. J Neurol Neurosurg Psychiatry 71:175–181. https://doi.org/10.1136/jnnp.71.2.175
Mack WJ, Hickman ZL, Ducruet AF et al (2008) Pupillary reactivity upon hospital admission predicts long-term outcome in poor grade aneurysmal subarachnoid hemorrhage patients. Neurocrit Care 8:374–379. https://doi.org/10.1007/s12028-007-9031-1
Coles JP, Fryer TD, Coleman MR et al (2007) Hyperventilation following head injury: effect on ischemic burden and cerebral oxidative metabolism. Crit Care Med 35:568–578. https://doi.org/10.1097/01.CCM.0000254066.37187.88
MekontsoDessap A, Katsahian S, Roche-Campo F et al (2014) Ventilator-Associated pneumonia during weaning from mechanical ventilation. Chest 146:58–65. https://doi.org/10.1378/chest.13-2564
Sleiwah A, Nair G, Mughal M et al (2020) Perioral pressure ulcers in patients with COVID-19 requiring invasive mechanical ventilation. Eur J Plast Surg 43:727–732. https://doi.org/10.1007/s00238-020-01737-6
Ahmed Bouderka M, Fakhir B, Bouaggad A et al (2004) Early tracheostomy versus prolonged endotracheal intubation in severe head injury: The Journal of Trauma: Injury. Infect Crit Care 57:251–254. https://doi.org/10.1097/01.TA.0000087646.68382.9A
Frontera JA, Fernandez A, Schmidt JM et al (2008) Impact of nosocomial infectious complications after subarachnoid hemorrhage. Neurosurgery 62:80–87. https://doi.org/10.1227/01.NEU.0000311064.18368.EA
Zafar SF, Postma EN, Biswal S et al (2018) Electronic health data predict outcomes after aneurysmal subarachnoid hemorrhage. Neurocrit Care 28:184–193. https://doi.org/10.1007/s12028-017-0466-8
Solaiman O, Singh JM (2013) Hypocapnia in aneurysmal subarachnoid hemorrhage: incidence and association with poor clinical outcomes. J Neurosurg Anesthesiol 25:254–261. https://doi.org/10.1097/ANA.0b013e3182806465
Towner JE, Rahmani R, Zammit CG et al (2020) Mechanical ventilation in aneurysmal subarachnoid hemorrhage: systematic review and recommendations. Crit Care 24:575. https://doi.org/10.1186/s13054-020-03269-8
Ponfick M, Wiederer R, Nowak DA (2015) Outcome of intensive care unit–dependent, tracheotomized patients with cerebrovascular diseases. J Stroke Cerebrovasc Dis 24:1527–1531. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.03.021
Foerch C (2004) Survival and quality of life outcome after mechanical ventilation in elderly stroke patients. J Neurol Neurosurg Psychiatry 75:988–993. https://doi.org/10.1136/jnnp.2003.021014
Fung C, Inglin F, Murek M et al (2016) Reconsidering the logic of World Federation of Neurosurgical Societies grading in patients with severe subarachnoid hemorrhage. J Neurosurg 124:299–304. https://doi.org/10.3171/2015.2.JNS14614
Svensson E, Starmark J-E, Ekholm S et al (1996) Analysis of interobserver disagreement in the assessment of subarachnoid blood and acute hydrocephalus on CT scans. Neurol Res 18:487–494. https://doi.org/10.1080/01616412.1996.11740459
van der Jagt M, Hasan D, Bijvoet HW et al (2000) Interobserver variability of cisternal blood on CT after aneurysmal subarachnoid hemorrhage. Neurology 54:2156–2158. https://doi.org/10.1212/wnl.54.11.2156
Stienen MN, Germans M, Burkhardt J-K et al (2018) Predictors of in-hospital death after aneurysmal subarachnoid hemorrhage: analysis of a Nationwide Database (Swiss SOS [Swiss Study on Aneurysmal Subarachnoid Hemorrhage]). Stroke 49:333–340. https://doi.org/10.1161/STROKEAHA.117.019328
Jabbarli R, Reinhard M, Roelz R et al (2016) The predictors and clinical impact of intraventricular hemorrhage in patients with aneurysmal subarachnoid hemorrhage. Int J Stroke 11:68–76. https://doi.org/10.1177/1747493015607518
Jabbarli R, Reinhard M, Niesen W-D et al (2015) Predictors and impact of early cerebral infarction after aneurysmal subarachnoid hemorrhage. Eur J Neurol 22:941–947. https://doi.org/10.1111/ene.12686
Funding
This study was supported by the National Natural Science Foundation of China (82173899), the Jiangsu Pharmaceutical Association (H202108, Q202202, A2021024), the Hunan Natural Science Foundation (2021JJ70021), and the Hunan innovation guidance grant of clinical medical technology (2020SK50920).
Author information
Authors and Affiliations
Contributions
ZZ, WL, and CZ contributed equally to this work. JJZ, ZHZ, and XMD provided ideas for the conception and design of the study. ZZ, WL, and CZ carried out the literature review. CZ, LX, LX, BJW, LHG, YJS, and XML organized the database. WL performed data analysis. ZZ and WL wrote all versions of the manuscript and tables. CC and ZZ polished this article. All authors contributed to manuscript revision, read, and approved the submitted version.
Corresponding authors
Ethics declarations
Ethics approval
The studies involving human participants were reviewed and approved by the Human Research Ethics committee of Hunan Provincial People’s Hospital (article number: [2015]-10).
Informed consent
The ethics committee waived the requirement of written informed consent for participation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The Authors agreed to swap the order of JianJun Zou and XiaoMing Dai to ensure that the corresponding author list in the official publication matches the original manuscript submission.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, Z., Lu, W., Zhang, C. et al. A visualized MAC nomogram online predicts the risk of three-month mortality in Chinese elderly aneurysmal subarachnoid hemorrhage patients undergoing endovascular coiling. Neurol Sci 44, 3209–3220 (2023). https://doi.org/10.1007/s10072-023-06777-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-06777-x