Abstract
Background
Measures adopted to contain the spread of SARS-CoV-2 could have led to a reduction in the rate of non-COVID-19 infections. We assessed whether a similar reduction was present in patients with stroke.
Methods
We performed a hospital-based study nested in a prospective population-based registry. We compared prevalence of infections and in-hospital mortality in subjects admitted for acute stroke between the first pandemic year (study period, from March 2020 to February 2021) and the pre-pandemic year (control period, from March 2019 to February 2020). Infections were reported as pneumonia (PNA), urinary tract infections (UTI), and any infection (INF).
Results
From the control (n = 677) to the study period (n = 520), the prevalence of INF decreased from 11.5 to 4.6% (p < 0.001) and that of PNA decreased from 6.9 to 2.5% (p = 0.001). No changes in in-hospital mortality and length of hospital stay were observed between the two periods.
Conclusions
The observed reduction of in-hospital pneumonias in patients with stroke was likely attributable to the use of protective measures and limitation of hospital visits. Maintaining some of those measures in the long term may contribute to control infections in hospitalized patients with stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The COVID-19 pandemic had a profound impact on care for non-communicable diseases [1] including stroke [2, 3]. While overall health systems were adversely affected by the pandemic, the adoption of stringent measures to prevent the spread of SARS-CoV-2 may have provided benefits in control of other infections. This is suggested by some reports [4, 5] but has not been explored in the setting of dedicated acute stroke care. We assessed whether the COVID-19 pandemic period was associated with a reduction of in-hospital infections in patients hospitalized with stroke.
Methods
Our study complies with the Strengthening The Reporting of OBservational studies in Epidemiology (STROBE) statement [6] (Supplementary Material).
This hospital-based study is nested within an ongoing prospective population-based registry conducted in the 298,343 residents [7] in the district of L’Aquila, central Italy. The district hosts 4 public hospitals, two of which have Stroke Units. The protocol was approved by the Internal Review Board of the University of L’Aquila with registration number 13/2018. Informed consent was obtained from the study participants or their authorized proxies. Data supporting findings of the present study are available from the corresponding author upon reasonable request.
We considered the study period as the first pandemic year from March 1, 2020, to February 28, 2021; comparisons were made with the period spanning from March 1, 2019, to February 29, 2020. The system of care for stroke did not change during the COVID-19 outbreak in the district. However, hospital protocols included mandatory use of surgical masks for all hospital staff, frequent use of sanitizing gel for hand hygiene, and visitor access restrictions; visitors also had to wear face masks and use sanitizing gel before entering wards.
We included all patients hospitalized for any type of stroke (cerebral ischemia, intracerebral hemorrhage, subarachnoid hemorrhage) within the study period. Two neurologists (RO and SS) validated the diagnoses. The presence of infections was assessed by checking medical records for pneumonia (PNA, ICD-9-CM codes 482–486), urinary tract infections (UTI, ICD-9-CM code 599), and generic infections without specified site (ICD-9-CM code 041). Diagnoses were validated by a geriatrician (GC). We excluded patients with COVID-19 including those with pneumonia.
Recorded information included patients’ age, sex, stroke type (ischemic stroke, intracerebral or subarachnoid hemorrhage), type of infection, Stroke Unit admission, length of hospital stay, and in-hospital mortality. Infections were reported as PNA, UTI, and any infection (INF, as a cumulative outcome of PNA and/or UTI and/or other generic infections without specified site).
Statistical analysis
We compared the yearly and quarterly (March–May, June–August, September–November, December–February) rates of PNA, UTI, and INF in the study period compared with the control period. Comparisons were made by the chi-squared test or Fisher exact test as appropriate. The distribution of patients’ characteristics between the study and control periods, including sex, median age, stroke subtypes, Stroke Unit admission, median length of hospital stay, and in-hospital mortality, was compared by the chi-squared or Wilcoxon test as appropriate, to verify comparability. Analyses were performed with the R software, version 4.1.2.
Results
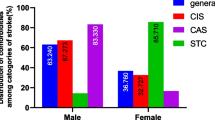
Patients hospitalized with stroke decreased from 667 in the control period to 520 in the study period (− 23.0%; p < 0.001). Patients’ characteristics did not differ between the two periods, except from a lower proportion of patients with stroke admitted to a Stroke Unit from the control to the study period (61.4 to 49.6%, p < 0.001; Table 1). From the control to the study period, INF decreased from 77 (11.5%) to 24 (4.6%; p < 0.001); in detail, PNA decreased from 46 (6.9%) to 13 (2.5%; p = 0.001), while UTI changed from 23 (3.4%) to 9 (1.7%; p = 0.103; Fig. 1). The decreases in the rate of PNA were significant during the second (June–August) and fourth quarter (December–February) of the considered years (Fig. 2). There was no difference in median length of hospital stay (7 vs 6 days, p = 0.826) and in-hospital case-fatality (11.3% vs 11.5%, p = 0.989) between the study and the control periods (Table 1).
Discussion
We observed a decrease in infections in patients hospitalized for stroke during the COVID-19 pandemic. In detail, the decrease was evident for PNAs, but not UTIs, which suggests a specific impact of preventive measures for airborne infections that can be attributed to the use of face masks, restriction of visits, and enhanced sanitization. Previous reports of decreased incidence of non-COVID-19 infections during the COVID-19 pandemic [4, 5] were not focused on patients with stroke. In our study, reduction of infections was not paralleled by reduced mortality or length of hospital stay possibly because of the low numbers of patients with infections in this analysis. Nevertheless, it is well known that infections—and mostly PNA [8]—can prolong hospital stay and increase mortality [9]; consequently, their prevention represents an important contribution to better stroke outcomes.
Considering our results, it may be suggested that maintaining use of face masks, restriction in visits to hospitalized patients, and enhanced sanitization in the long term could provide a benefit to patients with stroke. However, continuous use of face masks by the hospital staff could lead to discomfort, problems with communication, adherence, and misuse in the long term [10]. We have also to consider the additional cost and hospital waste brought by continuous use of face masks [11]. Besides, limitation of visits to patients might be associated with psychological distress and feelings of loneliness by patients, thus increasing the risk of delirium [12]. Lack of assistance by caregivers might also increase the burden on the hospital staff.
The strengths of our study include linkage to a population-based registry, comparable populations between the study and control periods, and additional analyses according to infection type and seasonality. As stated above, a limitation of the study is the low number of included patients with infections both before and during the pandemic, which could explain the lack of difference in in-hospital mortality between the two periods. Additionally, the diagnosis of infections was assessed by checking the codes in the medical records and we could not distinguish community-acquired from hospital-acquired pneumonia. We also cannot exclude that the decreased proportion of patients with stroke admitted to a Stroke Unit and the lowered attention to non-COVID-19 infections during the pandemic could have led to an underdiagnosis of infections. We do not have clear explanations for decreased admissions to Stroke Units; however, they could be determined at least in part by the reorganization of acute health care during the pandemic. We did not retrieve data about the severity of infections, as well as their long-term consequences. It is also worth noting that post-stroke pneumonia is not necessarily airborne but may be caused by weakness of swallowing leading to aspiration [13, 14]. Besides, we cannot fully exclude that other factors, such as decreased hospitalizations for stroke [2, 3], could have had a role in the decrease of non-COVID-19 infections in hospital settings.
In conclusion, during the COVID-19 pandemic, we observed a reduction of in-hospital pneumonias in patients with stroke, likely attributable to measures to contain COVID-19. Maintaining some of those measures in the long term may help controlling infections in patients with stroke and potentially improve patients’ outcomes.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Sheldon TA, Wright J (2020) Twin epidemics of covid-19 and non-communicable disease. BMJ m2618. https://doi.org/10.1136/bmj.m2618
Sacco S, Ricci S, Ornello R et al (2020) Reduced admissions for cerebrovascular events during COVID-19 outbreak in Italy. Stroke 51:3746–3750. https://doi.org/10.1161/STROKEAHA.120.031293
Nogueira RG, Abdalkader M, Qureshi MM et al (2021) Global impact of COVID-19 on stroke care. Int J Stroke 16:573–584. https://doi.org/10.1177/1747493021991652
Huang C (2021) The COVID-19 pandemic and the incidence of the non-COVID-19 pneumonia in adults. Front Med (Lausanne) 8: https://doi.org/10.3389/fmed.2021.737999
Tanislav C, Kostev K (2022) Fewer non-COVID-19 respiratory tract infections and gastrointestinal infections during the COVID-19 pandemic. J Med Virol 94:298–302. https://doi.org/10.1002/jmv.27321
von Elm E, Altman DG, Egger M et al (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370:1453–1457. https://doi.org/10.1016/S0140-6736(07)61602-X
Istituto Nazionale di Statistica (ISTAT) (2011) Censimento della popolazione e delle abitazioni 2011. https://dati.istat.it. Accessed 25 July 2022
Katzan IL, Cebul RD, Husak SH et al (2003) The effect of pneumonia on mortality among patients hospitalized for acute stroke. Neurology 60:620–625. https://doi.org/10.1212/01.WNL.0000046586.38284.60
Westendorp WF, Nederkoorn PJ, Vermeij J-D et al (2011) Post-stroke infection: a systematic review and meta-analysis. BMC Neurol 11:110. https://doi.org/10.1186/1471-2377-11-110
Bakhit M, Krzyzaniak N, Scott AM et al (2021) Downsides of face masks and possible mitigation strategies: a systematic review and meta-analysis. BMJ Open 11:e044364. https://doi.org/10.1136/bmjopen-2020-044364
Feng S, Shen C, Xia N et al (2020) Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med 8:434–436. https://doi.org/10.1016/S2213-2600(20)30134-X
Manca R, de Marco M, Venneri A (2020) The impact of COVID-19 infection and enforced prolonged social isolation on neuropsychiatric symptoms in older adults with and without dementia: a review. Front Psychiatry 11: https://doi.org/10.3389/fpsyt.2020.585540
Kumar S, Selim MH, Caplan LR (2010) Medical complications after stroke. Lancet Neurol 9:105–118. https://doi.org/10.1016/S1474-4422(09)70266-2
Johnston KC, Li JY, Lyden PD et al (1998) Medical and neurological complications of ischemic stroke. Stroke 29:447–453. https://doi.org/10.1161/01.STR.29.2.447
Funding
Open access funding provided by Università degli Studi dell’Aquila within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
Conceptualization: Simona Sacco, Raffaele Ornello; methodology: Simona Sacco, Raffaele Ornello; formal analysis and investigation: Giulia Ceccanti, Leondino Mammarella; writing—original draft preparation: Raffaele Ornello, Enrico Colangeli; writing—review and editing: Simona Sacco, Giovambattista Desideri.
Corresponding author
Ethics declarations
Ethical approval
The study is part of a protocol approved by the Internal Review Board of the University of L’Aquila with registration number 13/2018.
Research involving human participants and/or animals
This study was performed in line with the principles of the Declaration of Helsinki.
Informed consent
Informed consent was signed by patients or their authorized proxies.
Conflict of interest
RO reports personal fees from Novartis, Teva, and Eli Lilly and non-financial support from Novartis and Teva, all unrelated to the submitted work. SS reports personal fees as a speaker or advisor from Abbott, Allergan-Abbvie, AstraZeneca, Eli Lilly, Lundbeck, Novartis, NovoNordisk, Pfizer, and Teva; research grants from Allergan, Novartis, and Uriach; non-financial support from Abbott, Allergan, Bayer, Bristol-Myers Squibb, Daiichi-Sankyo, Eli Lilly, Lundbeck, Medtronic, Novartis, Pfizer, Starmed, and Teva; and fees for CME/education from Medscape and Neurodiem Ology Medical Education. All other authors declare no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ornello, R., Colangeli, E., Ceccanti, G. et al. Reduction of in-hospital non-COVID-19 pneumonia in stroke patients during the COVID-19 pandemic. Neurol Sci 44, 1849–1853 (2023). https://doi.org/10.1007/s10072-023-06712-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-06712-0