Abstract
Introduction
Vaccination against the coronavirus disease 2019 (COVID-19) is recommended for patients with multiple sclerosis (MS), neuromyelitis optica spectrum disorder (NMOSD), and myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD). However, vaccine safety in these patients taking immunotherapeutic agents is unclear as they were not included in the vaccine trials.
Objectives
To evaluate the safety of COVID-19 vaccines in patients with MS, NMOSD, and MOGAD.
Methods
We reviewed the medical records of MS, NMOSD, and MOGAD patients at the Keimyung University Dongsan Hospital. Information regarding vaccination schedules and adverse events was collected.
Results
A total of 56 patients (19, 22, and 15 patients with MS, NMOSD, and MOGAD, respectively) with a median age of 48.18 ± 15.72 years (range, 16–81 years) were included. Of them, 42 (75.0%) were female. In total, 76.8% (43/56) of all patients were vaccinated, and the vaccination rate was the highest for NMOSD patients (81.8%) and the lowest for MS patients (68.4%). All vaccinated patients were administered mRNA vaccines at least once in single or multiple vaccination doses. Only 3 of 43 (7.0%) vaccinated patients experienced clinical relapse following vaccination. Facial sensory changes with a brainstem lesion developed in an MS patient taking dimethyl fumarate, while myelitis occurred in a MOGAD patient receiving azathioprine maintenance therapy. The first episode of optic neuritis occurred in a patient who was later diagnosed with MOGAD.
Conclusions
Our study demonstrated a favorable safety profile with no serious adverse events associated with COVID-19 vaccines in patients with MS, NMOSD, and MOGAD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic is a global challenge that has placed a significant burden not only on public health care, but also on the society and economy. As a protective measure, mass vaccination and herd immunity have been emphasized by the World Health Organization (WHO) [1]. Vaccines against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) have been proven safe and effective in the general population [2,3,4,5,6]. In South Korea, five types of vaccines have been approved by the government: BNT162b2, Pfizer-BioNTech; mRNA-1273, Moderna; Ad26.COV2.S, Janssen; ChAdOx1, AstraZeneca; and NVX-CoV2373, Novavax; among these, ChAdOx1, BNT162b2, and mRNA-1273 are the most administered.
Patients with central nervous system (CNS) demyelinating diseases such as multiple sclerosis (MS), neuromyelitis optica spectrum disorders (NMOSD), and myelin oligodendrocyte glycoprotein antibody–associated disease (MOGAD) can experience disease exacerbation or clinical relapse following SARS-CoV-2 infection [7, 8]. In addition, it is expected that patients with underlying neurological disabilities might be prone to severe COVID-19 infection [9,10,11,12]. Therefore, they are considered high-risk groups and are prioritized in vaccination according to the Centers for Disease Control and Prevention (CDC) recommendations [13].
Vaccination against COVID-19 is an important strategy to overcome the pandemic. However, because patients with CNS demyelinating disease were not included in previous vaccine trials, vaccine safety is not yet fully established. In addition, vaccination is a complex issue in this population considering that these patients are frequently subjected to immunomodulatory or immunosuppressive treatments. A number of recent studies of patients with MS have shown that COVID-19 vaccination does not increase the risk of clinical relapse and serious adverse events, suggesting favorable safety of COVID-19 vaccine in MS patients [14,15,16]. The issue of immunogenicity of COVID-19 vaccines in relation to MS medications has also been evaluated in some studies [17, 18]. They reported that some disease-modifying therapies for MS, such as fingolimod and ocrelizumab, can reduce the humoral response to COVID-19 vaccine, which may negatively affect vaccine efficacy. Patients with NMOSD and MOGAD showed a tolerable safety profile for the COVID-19 vaccine in two recent studies [19, 20]. However, compared to MS patients, studies on these patients are still insufficient to draw any substantive conclusions regarding the safety of COVID-19 vaccines. Therefore, this study aimed to evaluate the current vaccination status and safety profile of COVID-19 vaccines in MS, NMOSD, and MOGAD patients by examining post-vaccination adverse events and related clinical relapses.
Materials and methods
Study design and participants
This retrospective study evaluated data of patients from the CNS demyelinating disease registry of Keimyung University Dongsan Hospital. The study included patients diagnosed with MS based on the 2017 revised McDonald criteria [21], patients diagnosed with NMOSD based on the 2015 International Panel for NMO Diagnosis NMOSD diagnostic criteria [22], and patients diagnosed with MOGAD based on the 2018 proposed diagnostic criteria for MOGAD by López-Chiriboga et al. [23]. Those who did not visit the hospital after January 2021, the beginning period of COVID-19 mass vaccination in South Korea, and those without sufficient vaccination data were excluded. Finally, 56 patients (19 (33.9%), 22 (39.3%), and 15 (26.8%) patients with MS, NMOSD, and MOGAD, respectively) were enrolled in the study.
Data collection
Data were collected from the patients’ medical records and included age, sex, medical history, prescribed medications, and neurological status measured using the Expanded Disability Status Scale (EDSS). Data on COVID-19 infection and vaccination were also collected. The vaccination status with detailed schedules, types of vaccines administered, occurrence of adverse events including relapse, and/or COVID-19 infection following vaccination were investigated in individual patients. Vaccine-related adverse events were categorized as short-term local and systemic reactions and clinical relapse. Local (e.g., injection site pain, swelling, or redness) and systemic (e.g., febrile sensation, myalgia, headache, or dizziness) reactions were collected that occurred within 7 days after each dose vaccination [2,3,4]. Clinical relapses were considered vaccine-related if they occurred within 42 days of each dose vaccination [24,25,26].
Statistical analysis
Descriptive analyses of the variables were performed. The patients were stratified by diagnosis into MS, NMOSD, and MOGAD groups. Statistics were calculated for the clinical characteristics and COVID-19 vaccination data. Age and EDSS scores were described as means with standard deviations. Analysis of variance was performed to compare the means of the three groups. Disease duration was shown as the median with interquartile range. The Kruskal–Wallis test was used for non-parametric analysis to determine the differences among the three subgroups. All statistical analyses were performed using SPSS Statistics (IBM Corp. Released 2019. IBM SPSS Statistics for Windows, Version 26.0.) and Microsoft Excel (Microsoft Corp. Released 2016. Microsoft Excel). Statistical significance was set at p ≤ 0.05.
Results
Patient demographics and disease parameters
The mean patient age was 48.18 ± 15.72 years. The clinical demographics and disease parameters are shown in Table 1. NMOSD patients were older than MS and MOGAD patients (55.64 ± 16.29 years vs 40.16 ± 13.64 and 47.40 ± 12.56 years, p = 0.005). The majority of NMOSD patients (90.9%) were women. Other groups also showed female predominance, but not as definite as that in NMOSD. In total, 19 (86.4%) of NMOSD patients were seropositive for aquaporin-4 antibody, whereas all MOGAD patients were positive for MOG antibody. The median disease duration of CNS demyelinating disease from the first onset of neurologic symptoms was 33.0 (range, 14.0–88.3) months for the entire patient. The disease duration was longer in NMOSD patients than in MS and MOGAD patients (82.0 (range, 38.5–141.3) months vs 29.0 (range, 9.0–86.0) months and 17.0 (7.0–30.0) months, p = 0.002). Similarly, the EDSS score was also higher in NMOSD patients than in MS and MOGAD patients (3.21 ± 2.59 vs 1.66 ± 1.60 and 1.63 ± 2.11, p = 0.039). All MS patients, except one patient, were on disease-modifying therapy. Only two MOGAD patients were not on immunosuppressive drugs, and all NMOSD patients were on immunosuppressive therapy.
Vaccination rate, immunization information, and reason for suspending vaccination
Detailed vaccination information and reasons for suspending vaccination are presented in Table 2. In total, 43 patients were vaccinated at least once, yielding an overall vaccination rate of 76.8%. Among them, 39 and 27 patients received the second and third booster doses, respectively. In all groups, the mRNA vaccine BNT162b2 was the most frequently used type of vaccine, followed by the mRNA-1283 and ChAdOx1. All patients received mRNA vaccines at least once in single or multiple vaccination doses. NMOSD patients showed the highest vaccination rate at 81.8%, and most of them received additional doses. Of the 22 NMOSD patients, 16 and 14 patients received a second and third dose of booster injection, respectively. MS patients showed the lowest vaccination rate at 68.4%, indicating reluctance in these patients. There were 13 patients who were vaccinated, but less than half of them (6 patients) chose to receive the 3rd (booster) dose. Meanwhile, the vaccination rate in MOGAD patients was 80.0%, comparable to that in NMOSD patients. With respect to the reasons for suspending vaccination, the most common was the hypothetical worry of relapse, even without experiencing adverse symptoms. Six patients were prevented from vaccination due to active neurologic disease with preceding recent relapses. The other three patients reported suspending booster injection because of the fear of relapse as they experienced some form of a neurologic symptom as a side effect of their prior vaccination.
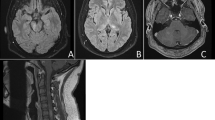
Vaccine-related adverse events and breakthrough infections
The patients reported several side effects following vaccination. One-third (16/43, 37.2%) of the patients who were vaccinated experienced minor symptoms following administration (e.g., febrile sensation, myalgia, dizziness, or injection site pain) that resolved spontaneously after a few days. Although small in number, 3/43 patients (7%) had neurologic symptoms such as a tingling sensation in the extremities or subjective weakness in the limbs. In addition, another 3 (7%) vaccinated patients experienced relevant clinical relapse following vaccination. Facial sensory changes with a brainstem lesion developed in an MS patient (34-year-old man) taking dimethyl fumarate 2 weeks following the first dose of the BNT162b2 vaccine, while myelitis presented as a left-hand tingling sensation in a MOGAD patient (30-year-old woman) receiving azathioprine maintenance therapy 4 weeks after the second dose of the BNT162b2 vaccine. The other patient was a 42-year-old woman who developed visual disturbance 1 week after the third dose of the BNT162b2 vaccine. She was later diagnosed with left optic neuritis and positive MOG-Ab. Breakthrough SARS-CoV-2 infection occurred in 14 (32.6%) of 43 vaccinated patients. Of the 13 unvaccinated patients, 3 (23.1%) developed COVID-19 infection. Comparing vaccinated patients with breakthrough SARS-CoV-2 infection with unvaccinated infected patients, there was no difference in hospitalization rates for COVID-19 infection (1/14 (7.1%) vs 0/3 (0%), respectively; p = 1). However, all three unvaccinated patients infected with SARS-CoV-2 reported neurologic deterioration following COVID-19 infection, whereas only 21.4% (3/14) of vaccinated patients with breakthrough SARS-CoV-2 infection had it (p = 0.029). The findings are presented in Table 3.
Discussion
Clinical trials of vaccines against SARS-CoV-2 infection have shown their safety and efficacy. However, the safety and efficacy of these vaccines in patients with CNS demyelinating disease are still unclear as previous studies only involved healthy adults [4, 6] and excluded those on immunotherapy [5] or with chronic neurologic disease [2]. The present study recruited 56 patients with MS, NMOSD, or MOGAD. Almost all patients (94.6%) received immunotherapy during the period of mass vaccination. MS patients were the most skeptical about vaccination, while NMOSD patients showed the highest vaccination rate. The biggest reason for suspending vaccination was the worry about worsening of neurological status.
The estimated vaccination rate against SARS-CoV-2 in South Korea is 87.3%, according to a government announcement in February 2022 [27]. The overall vaccination rate in the current study was 76.8%, lower than that in the general population. This result may reflect the prevalent vaccine hesitancy among the MS, NMOSD, and MOGAD patients. A survey study on COVID-19 vaccination hesitancy in patients with chronic neurological disorders conducted by the European Academy of Neurology NeuroCOVID-19 Task Force [28] reported that patients, particularly those with autoimmune CNS disorders and MS, were reluctant to be vaccinated. Our study confirms this tendency. In addition, the Task Force explained that the most popular arguments against vaccination in these patients were the probability of worsening of the neurological disease; adverse reactions following vaccine injection; and the possible interaction with their prescribed medications, including immunosuppressants. The most common reason for suspending vaccination in the current study was the concern about clinical relapse or neurological deterioration, regardless of the presence of neurological symptoms. Interestingly, our subjects shared similar beliefs to those in the European study despite substantial ethnic and cultural differences.
There was a conspicuous difference in vaccination rates between the MS and NMOSD groups. MS patients were more hesitant about getting vaccinated than NMOSD patients. MS patients were significantly younger than NMOSD patients, and this age factor might have influenced decision-making. Previous studies have proven that younger people are more reluctant about COVID-19 vaccination [29, 30]. In addition, it is suggested that the “infodemic,” which means the superfluous information of unreliable and unverified contents from the Internet or social media channels, can lead to fallacy among the young population [28]. In addition, NMOSD patients had a longer disease duration and a higher degree of disability than MS patients. This finding is in line with a previous CDC report [31] that people with disabilities are more willing to be vaccinated. Skepticism about vaccine safety might be decreased by a stable neurological status in chronic disease.
Among the MS, NMOSD, and MOGAD patients, the decision about getting COVID-19 vaccination is mostly affected by concerns regarding vaccine safety [28]. There have been reports describing aggravation or reactivation of CNS demyelinating disease following vaccinations [32,33,34]. Specifically, new-onset MOGAD appeared to be a reasonable adverse event [35, 36] of COVID-19 vaccination. In the current study, one patient was newly diagnosed with MOGAD with optic neuritis 1 week after the third dose of the BNT162b2 vaccine. Another patient with MOGAD had a relapse with myelitis. Three patients with MS complained of neurological symptoms, but only one had an actual clinical relapse. In our study, all patients except three were treated with immunosuppressive or immunomodulatory therapy to control disease activity. Given that most patients require such treatment to prevent relapses, relapses may be frequent due to the disease activity itself, regardless of COVID-19 vaccination. However, most patients in this study had stable disease that was well controlled with low or intermediate efficacy therapy at the time of vaccination, suggesting a low risk of relapse due to the disease itself. In particular, among the three patients with clinical relapse after COVID-19 vaccination, one was a newly developed MOGAD patient, and the other two (one MS patient and one MOGAD patient) had no relapse at all for 1 year before vaccination. Therefore, relapse in these patients may be more likely to be related to vaccination rather than due to the activity of the disease itself. However, since our study defined the association between COVID-19 vaccination and clinical relapse only as a temporal relationship, additional research is needed on the significance of relapse after vaccination.
There are quite a number of studies on the safety of the COVID-19 vaccine in patients with MS. In a Polish study of 2261 MS patients who received the COVID-19 vaccine, 70.6% (1597/2261) of patients experienced side effects after vaccination, but most of them were mild symptoms such as flu-like symptoms and injection site pain [15]. In addition, only 4.4% (99/2261) of patients experienced a relapse after vaccination. A recent systematic review and meta-analysis of 19 studies comprising 14,755 SARS-CoV-2-vaccinated patients with MS also found that the pooled proportion of MS patients with relapse after vaccination was only 1.9% [16]. Moreover, the proportion of patients with serious adverse events was as low as 0.1%. The National MS Society recently announced that both BNT162b2 and mRNA-1273 vaccines are safe for MS patients and not related to neurological exacerbations or long-term disease progression [37]. In our study, although the number of MS patients who received the COVID-19 vaccine at least once was small at 13 to evaluate the safety of the vaccine, only 1 patient experienced a relapse after vaccination, and there were no serious adverse events. Our results along with previous findings suggest that the risk of relapse and serious adverse events after COVID-19 vaccination in MS patients is low, indicating that the COVID-19 vaccine is safe for most patients with MS.
There are scant data provided from controlled studies supporting the safety of the COVID-19 vaccine in patients with NMOSD and MOGAD. Recently, a survey study on COVID-19 vaccination in 242 patients with NMOSD, 99 with MOGAD, and 79 with transverse myelitis showed a relatively low rate (16.7% of all patients) of new or worsening neurologic symptoms after vaccination [19]. Moreover, the severity of those symptoms was mild, requiring medical treatment in only 17.8% of patients with neurological deterioration. In an Italian study that investigated the risk of relapse within 1 month after COVID-19 vaccination in 26 patients with NMOSD and 30 with MOGAD, relapse occurred in only 1 patient (4%) with NMOSD and none with MOGAD [20]. In the present study, the majority of the vaccine-related complaints in patients with NMOSD and MOGAD were early reactions like injection site pain or minor systemic side effects such as febrile sensation, myalgia, and dizziness which spontaneously resolved after a few days. Even their overall rate of vaccine-related side effects was lower than that of MS patients. Relapse or new-onset disease after vaccination was not found in patients with NMOSD, but in 2 patients (16.7%) with MOGAD. This was similar to or slightly lower than the results of previous studies. Our findings support previous results on the safety of COVID-19 vaccines in patients with NMOSD and MOGAD.
COVID-19 vaccine efficacy is another important issue in patients with MS, NMOSD, and MOGAD because many of these patients are on immunotherapies. Reduced immunogenicity of the COVID-19 vaccine in patients with chronic inflammatory diseases, including those with MS and NMOSD who are taking immunotherapy drugs, has been reported in previous studies [17, 18, 38, 39]. Particularly in MS patients receiving fingolimod, alemtuzumab, or anti-CD20 monoclonal antibodies (ocrelizumab and rituximab), consideration of the timing of vaccine administration is required due to the potential for reduced vaccine efficacy associated with these drugs [37]. Immunogenicity to vaccination may also be reduced when corticosteroids are used continuously for more than 14 days in high doses of 20 mg/day or more in patients with NMOSD [40]. In the current study, all except three patients were on immunomodulatory or immunosuppressive therapy. Overall, 14 vaccinated patients (32.6%) had breakthrough COVID-19 infection. While it is unsatisfactory for reported vaccine efficacy in previous phase 3 clinical trials [2, 41], we assumed that these breakthrough infections also occurred in part by reduced immunogenicity and, more importantly, because of the spread of the omicron variant in South Korea. Among the 14 vaccinated patients with breakthrough infection, only 1 patient (7.1%) was hospitalized. In addition, all unvaccinated infected patients had neurologic deterioration after COVID-19 infection, but only 21.4% of vaccinated patients with breakthrough infection reported worsening of neurologic symptoms. The findings of this study support previous observations that vaccines play a preventive role in severe COVID-19 infections, of which patients with CNS demyelinating disease are at high risk [9, 12]. Thus, it is essential for them to be vaccinated.
The present study had some limitations. First, it was designed in a retrospective manner, and patients were recruited from a single tertiary center. In addition, the sample size was small, and thus, the results may have limited generalizability. The association between COVID-19 vaccination and adverse symptoms was defined only by a temporal relationship. The exact causality should be examined to confirm the adverse effects of vaccination. Nonetheless, it was valuable to identify concerns regarding COVID-19 vaccination among MS, NMOSD, and MOGAD patients and to evaluate the actual vaccination status in these patients. To our best knowledge, this is the first study on the actual outcome and patients’ attitudes to COVID-19 vaccination in patients including NMOSD and MOGAD in addition to MS. A number of researches were carried out to investigate the safety and efficacy of COVID-19 vaccines in MS. However, not much is determined in NMOSD and MOGAD on this topic. The strength of our study resides in including NMOSD and MOGAD patients and exploring the similar concerns among them.
In conclusion, the present study demonstrated a relatively favorable safety profile of COVID-19 vaccines without serious adverse events in patients with NMOSD and MOGAD as well as in those with MS.
Data availability
Data can be obtained by contacting the corresponding author upon reasonable request.
References
Coronavirus disease (COVID-19): Herd immunity, lockdowns and COVID-19. Internet (2022) Who.int. https://www.who.int/news-room/questions-and-answers/item/herd-immunity-lockdowns-and-covid-19. Accessed 11 Jul 2022
Baden LR, El Sahly HM, Essink B et al (2021) Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med 384:403–416. https://doi.org/10.1056/NEJMoa2035389
Rosenblum HG, Gee J, Liu R et al (2022) Safety of mRNA vaccines administered during the initial 6 months of the US COVID-19 vaccination programme: an observational study of reports to the Vaccine Adverse Event Reporting System and v-safe. Lancet Infect Dis 22:802–812. https://doi.org/10.1016/S1473-3099(22)00054-8
Sadoff J, Gray G, Vandebosch A et al (2021) Safety and efficacy of single-dose Ad26.COV2.S vaccine against Covid-19. N Engl J Med 384:2187–2201. https://doi.org/10.1056/NEJMoa2101544
Thomas SJ, Moreira ED, Kitchin N et al (2021) Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine through 6 months. N Engl J Med 385:1761–1773. https://doi.org/10.1056/NEJMoa2110345
Voysey M, Clemens SAC, Madhi SA et al (2021) Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 397:99–111. https://doi.org/10.1016/S0140-6736(20)32661-1
MacDougall M, El-Hajj Sleiman J, Beauchemin P, Rangachari M (2022) SARS-CoV-2 and multiple sclerosis: potential for disease exacerbation. Front Immunol 13:871276. https://doi.org/10.3389/fimmu.2022.871276
Topolski M, Soti V (2022) Effects of COVID-19 on multiple sclerosis relapse: a comprehensive review. Int J Med Stud 10:192–201. https://doi.org/10.5195/ijms.2022.1241
Arrambide G, Llaneza-González MÁ, Costa-Frossard França L, Meca-Lallana V, Díaz EF, Moreno-Torres I, García-Domínguez JM, Ortega-Suero G, Ayuso-Peralta L, Gómez-Moreno M, Sotoca-Fernández JJ, Caminero-Rodríguez AB, Rodríguez de Antonio LA, Corujo-Suárez M, Otano-Martínez MA, Pérez-Miralles FC, Reyes-Garrido V, Ayuso-Blanco T, Balseiro-Gómez JJ, Muñoz-Pasadas M, Pérez-Molina I, Arnal-García C, Domingo-Santos Á, Guijarro-Castro C, Íñiguez-Martínez C, Téllez Lara N, Castellanos-Pinedo F, Castillo-Triviño T, Cerdán-Santacruz DM, Pérez-Sempere Á, Torres BS, Álvarez de Arcaya A, Costa-Arpín E, Durán-Ferreras E, Fragoso-Martínez M, González-Platas M, Landete Pascual L, Millán-Pascual J, Oreja-Guevara C, Meca-Lallana JE (2021) SARS-CoV-2 infection in multiple sclerosis: results of the spanish neurology society registry. Neurol Neuroimmunol Neuroinflamm 8(5):e1024. https://doi.org/10.1212/NXI.0000000000001024
Hada M, Mosholder AD, Leishear K, Perez-Vilar S (2022) Systematic review of risk of SARS-CoV-2 infection and severity of COVID-19 with therapies approved to treat multiple sclerosis. Neurol Sci 43:1557–1567. https://doi.org/10.1007/s10072-021-05846-3
Louapre C, Collongues N, Stankoff B et al (2020) Clinical characteristics and outcomes in patients with coronavirus disease 2019 and multiple sclerosis. JAMA Neurol 77:1079–1088. https://doi.org/10.1001/jamaneurol.2020.2581
Sormani MP, De Rossi N, Schiavetti I et al (2021) Disease-modifying therapies and coronavirus disease 2019 severity in multiple sclerosis. Ann Neurol 89:780–789. https://doi.org/10.1002/ana.26028
COVID-19 vaccines for people who are moderately or severely immunocompromised. Internet (2022). Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/immuno.html. Accessed 11 Jul 2022
Di Filippo M, Cordioli C, Malucchi S et al (2022) mRNA COVID-19 vaccines do not increase the short-term risk of clinical relapses in multiple sclerosis. J Neurol Neurosurg Psychiatry 93:448–450. https://doi.org/10.1136/jnnp-2021-327200
Czarnowska A, Tarasiuk J, Zajkowska O et al (2022) Safety of vaccines against SARS-CoV-2 among Polish patients with multiple sclerosis treated with disease-modifying therapies. Vaccines (Basel) 10(5):763. https://doi.org/10.3390/vaccines10050763
Stefanou MI, Palaiodimou L, Theodorou A, Christodoulou MV, Tzartos JS, Tzanetakos D, Kitsos D, Chondrogianni M, Zouvelou V, Dardiotis E, Tzavellas E, Syrigou E, Benetou V, Paraskevas GP, Tsiodras S, Tsivgoulis G, Giannopoulos S (2023) Safety of COVID-19 vaccines in multiple sclerosis: A systematic review and metaanalysis. Mult Scler. https://doi.org/10.1177/13524585221150881
Capone F, Lucchini M, Ferraro E et al (2022) Immunogenicity and safety of mRNA COVID-19 vaccines in people with multiple sclerosis treated with different disease-modifying therapies. Neurotherapeutics 19:325–333. https://doi.org/10.1007/s13311-021-01165-9
Sormani MP, Inglese M, Schiavetti I et al (2021) Effect of SARS-CoV-2 mRNA vaccination in MS patients treated with disease modifying therapies. EBioMedicine 72:103581. https://doi.org/10.1016/j.ebiom.2021.103581
Lotan I, Romanow G, Levy M (2021) Patient-reported safety and tolerability of the COVID-19 vaccines in persons with rare neuroimmunological diseases. Mult Scler Relat Disord 55:103189. https://doi.org/10.1016/j.msard.2021.103189
Dinoto A, Sechi E, Ferrari S et al (2022) Risk of disease relapse following COVID-19 vaccination in patients with AQP4-IgG-positive NMOSD and MOGAD. Mult Scler Relat Disord 58:103424. https://doi.org/10.1016/j.msard.2021.103424
Thompson AJ, Banwell BL, Barkhof F et al (2018) Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol 17:162–173. https://doi.org/10.1016/S1474-4422(17)30470-2
Wingerchuk DM, Banwell B, Bennett JL et al (2015) International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 85:177–189. https://doi.org/10.1212/WNL.0000000000001729
López-Chiriboga AS, Majed M, Fryer J et al (2018) Association of Mog-IgG Serostatus with relapse after acute disseminated encephalomyelitis and proposed diagnostic criteria for MOG-IgG–associated disorders. JAMA Neurol 75:1355–1363. https://doi.org/10.1001/jamaneurol.2018.1814
Butler M, Tamborska A, Wood GK et al (2021) Considerations for causality assessment of neurological and neuropsychiatric complications of SARS-CoV-2 vaccines: from cerebral venous sinus thrombosis to functional neurological disorder. J Neurol Neurosurg Psychiatry 92:1144–1151. https://doi.org/10.1136/jnnp-2021-326924
Netravathi M, Dhamija K, Gupta M et al (2022) COVID-19 vaccine associated demyelination & its association with MOG antibody. Mult Scler Relat Disord 60:103739. https://doi.org/10.1016/j.msard.2022.103739
Woo EJ, Mba-Jonas A, Dimova RB et al (2021) Association of receipt of the Ad26.COV2.S COVID-19 vaccine with presumptive Guillain-Barré syndrome, February-July 2021. JAMA 326:1606–1613. https://doi.org/10.1001/jama.2021.16496
COVID-19 Vaccination. Internet (2022) Korea disease control and prevention agency. https://ncv.kdca.go.kr/. Accessed 11 Jul 2022
Rakusa M, Öztürk S, Moro E et al (2022) COVID-19 vaccination hesitancy among people with chronic neurological disorders: a position paper. Eur J Neurol 29(8):2163–2172. https://doi.org/10.1111/ene.15368
Allen JD, Feng W, Corlin L et al (2021) Why are some people reluctant to be vaccinated for COVID-19? A cross-sectional survey among U.S. Adults in May–June 2020. Prev Med Rep 24:101494. https://doi.org/10.1016/j.pmedr.2021.101494
Kim S, Eun MY, Seok HY (2023) Letter to the Editor: consideration of neuroimmunological diseases in assessments of COVID-19 vaccination rates among patients with chronic medical conditions. J Korean Med Sci 38:e35. https://doi.org/10.3346/jkms.2023.38.e35
Ryerson AB, Rice CE, Hung MC et al (2021) Disparities in COVID-19 vaccination status, intent, and perceived access for noninstitutionalized adults, by disability status - National immunization survey adult COVID module, United States, May 30–June 26, 2021. MMWR Morb Mortal Wkly Rep 70:1365–1371. https://doi.org/10.15585/mmwr.mm7039a2
Hamed Y, Abd Elaziz Shokry TM, Shehata KMA, Osman SM (2021) Could COVID-19 vaccine induce CNS demyelination. J Mult Scler 8:281
Ismail II, Salama S (2022) A systematic review of cases of CNS demyelination following COVID-19 vaccination. J Neuroimmunol 362:577765. https://doi.org/10.1016/j.jneuroim.2021.577765
Khayat-Khoei M, Bhattacharyya S, Katz J et al (2022) COVID-19 mRNA vaccination leading to CNS inflammation: a case series. J Neurol 269:1093–1106. https://doi.org/10.1007/s00415-021-10780-7
Mărginean CO, Meliț LE, Cucuiet MT, Cucuiet M, Rațiu M, Săsăran MO (2022) COVID-19 Vaccine-A potential trigger for MOGAD transverse myelitis in a Teenager-A case report and a review of the literature. Children (Basel) 9(5):674. https://doi.org/10.3390/children9050674
Matsumoto Y, Ohyama A, Kubota T et al (2022) MOG antibody-associated disorders following SARS-CoV-2 vaccination: a case report and literature review. Front Neurol 13:845755. https://doi.org/10.3389/fneur.2022.845755
Society NMS (2022) COVID-19 Vaccine guidance for people living with MS. https://www.nationalmssociety.org/coronavirus-covid-19-information/covid-19-vaccine-guidance. Accessed 29 Aug 2022
Deepak P, Kim W, Paley MA et al (2021) Effect of immunosuppression on the immunogenicity of mRNA vaccines to SARS-CoV-2: a prospective cohort study. Ann Intern Med 174:1572–1585. https://doi.org/10.7326/M21-1757
Furer V, Eviatar T, Zisman D et al (2021) Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in adult patients with autoimmune inflammatory rheumatic diseases and in the general population: a multicentre study. Ann Rheum Dis 80:1330–1338. https://doi.org/10.1136/annrheumdis-2021-220647
Cai H, Zhou R, Jiang F, Zeng Q, Yang H (2022) Vaccination in neuromyelitis optica spectrum disorders: friend or enemy? Mult Scler Relat Disord 58:103394. https://doi.org/10.1016/j.msard.2021.103394
Polack FP, Thomas SJ, Kitchin N et al (2020) Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med 383:2603–2615. https://doi.org/10.1056/NEJMoa2034577
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by both authors. The first draft of the manuscript was written by Sohyeon Kim. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Institutional Review Board of Keimyung University Dongsan Hospital approved this study.
Informed consent
Informed consent was waived by our institutional ethical board since the research involves no more than minimal risk to participants and does not adversely affect the rights and welfare of them.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, S., Seok, H.Y. Evaluation of the safety profile of COVID-19 vaccines in patients with MS, NMOSD, and MOGAD. Neurol Sci 44, 1841–1848 (2023). https://doi.org/10.1007/s10072-023-06676-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-06676-1