Abstract
Background
At the moment, the possible options for the management of cognitive dysfunctions in patients with MS (pMS) are pharmacological interventions, cognitive rehabilitation (CR), and physical exercise. However, worldwide, multimodal programs are infrequently applied in pMS and CR is not easily accessible through the National Health System as MR.
Objective
The aim of the study is to explore if the combination of motor and cognitive rehabilitation may favor better outcomes on cognitive efficiency compared to separate trainings.
Methods
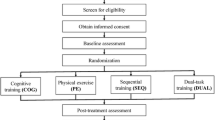
Forty-eight pMS were submitted to detailed neuropsychological and motor assessments, before (T0) and after (T1) having performed one of three rehabilitation conditions (two cognitive trainings/week-Reha1; one cognitive and one motor training/week-Reha2; two motor trainings/week-Reha3, for 12 weeks); they were randomly assigned to one condition or another. The CR was focused on memory functioning and performed with the Rehacom program.
Results
No significant differences in age, sex, education, and disease course were found between the three groups (sig. > .05). Reha1 patients increased only their cognitive performance, and Reha3 only increased their motor performance, while Reha2 increased both cognitive and motor performances. This benefit was also confirmed by the cognitive efficiency expressed by the Cognitive Impairment Index.
Conclusions
These data confirm that to include cognitive training within rehabilitation programs may induce important benefits in pMS. Furthermore, pMS seem to benefit from a combined approach (cognitive and motor) more than from CR and motor rehabilitation separately (ClinicalTrial.gov ID: NCT05462678; 14 July 2022, retrospectively registered).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple sclerosis (MS) is a demyelinating disease of the central nervous system characterized by inflammation, axonal demyelination, and neurodegeneration. It affects people in the prime of their life [1]. Its chronic course and consequent disabilities can highly impact on patients and families’ quality of life, affective and relational life, and on work activity.
From a clinical point of view, patients with MS (pMS) have a rather heterogeneous clinical condition, characterized by motor, sensory, autonomic disorders, and cognitive dysfunctions [2]: in about 60% of pMS, cognitive deficits appear associated with motor disabilities. The main consequences of motor disability concern walking difficulties and balance maintaining [3] as they have a more direct impact on daily tasks. pMS often cut down on their activities because of their fear of the exacerbation of symptoms and this can cause a deconditioning effect that may reduce their access to everyday life activities [4]. For these reasons, a rehabilitation program focused on the enhancement of walking ability is considered essential by the 65% of pMS [5].
Advances in physical rehabilitation of MS include conventional exercise (resistance/endurance training, balance training) and task-oriented training, which can be performed in addition to different types of “passive” treatments, such as noninvasive brain stimulation (NIBS: repetitive transcranial magnetic stimulation, magnetic theta burst stimulation, and transcranial direct current stimulation). These treatments aim to enhance the effects of physical rehabilitation, which range from improvement of muscle power and strength, exercise tolerance and mobility-related activities, improvement of cardiorespiratory capacity, reduction of patient-reported fatigue, to coordination of sensorimotor processes needed for balance and gait, as emphasized in a recent review [6].
Although once motor deficits appear they are not easy to be reduced by pharmacological treatments, a good efficacy of rehabilitation strategies on motor deficits has widely been demonstrated [7, 8]. In particular, it seems that motor rehabilitation (MR) is able to improve the compromised functional aspects when pMS undergo a specific treatment, and this effect is probably connected to structural and functional changes in the brain.
On the other hand, the cognitive disability and its impact on pMS’ life has also been widely reported in the scientific literature. Several studies showed that, regardless of illness duration and physical disability level, cognitive impairments (CI) have a significant functional impact and a negative influence on pMS’ quality of life, professional career, and social participation [9]. CI have recently been found to negatively affect daily activities such as driving, vocational status, absenteeism, and instrumental activities in pMS. In particular, pMS with CI show reduced levels of activity and participation in daily life, work, and social activities when compared with cognitively preserved pMS [10]. Furthermore, CI interferes with coping strategies and adherence to treatments [11, 12].
As widely suggested by the literature, CI affects every course of the disease with specific cognitive profiles [13]. The most frequently impaired domains are memory, attention, and processing speed and deficits seem to be more prevalent and severe in progressive forms of the disease [13, 14]. This may be explained by the fact that, in the early phases of the disease, pMS undergo a functional brain reorganization that may contribute to the maintenance of normal levels of cognitive performance; in the more advanced phases of the disease, the functional reorganization may contribute to cognitive dysfunctions [15]. Furthemore, memory deficit is the one that most severely impacts on relational and social aspects [16].
Till now, CI appears to be particularly resistant to the positive effects of drug therapies, both those disease modifying and those specifically aimed at treating cognitive deficits [17]. Therefore, it is important to seek other treatments aimed at strengthening cognitive functions. Promising results have been found for cognitive rehabilitation (CR) especially for the CR applied to memory complaint which seems to be particularly susceptible to cognitive trainings [18]. However, it should be noted that, even today, we can find conflicting results on which rehabilitation approach is most suitable for the enhancement of specific cognitive functions. Some studies focused their approach on CR of the specific impaired function [19]. Others with a more widespread approach focused on the rehabilitation of cognitive functions associated with that of interest [20]. Still others demonstrated how a better rehabilitation outcome can derive from a multimodal approach that associates CR paths with motor exercise training [21].
However, the primary problem is that, in this confounding context of results, CI remains often untreated and the preferential rehabilitation approach still remains focused on motor aspects.
It has been recently found that the real disabling impact of a neurological condition, like MS, is hardly computable without considering the effect of the interaction between cognitive and motor aspects [22]. Given this, we can speculate that even for rehabilitation the concurrent stimulation of both motor and cognitive functions may give pMS a better outcome in everyday life.
Unlike MR, CR has been little explored and applied for rehabilitation/enhancement of cognitive functions in MS. For this reason, primary aim of this study is to evaluate which of the three rehabilitation interventions (CR, MR, and combined CR + MR) can offer patients a better outcome with a specific focus on cognitive efficiency (especially on memory). This may increase the possibilities of treating CI and guaranteeing better outcomes for pMS, on both motor and cognitive efficiency. We also aim to explore which one of the three approaches gives pMS a better outcome in terms of everyday cognitive efficiency, and gait,,balance and mood improvement.
Materials and methods
Participants
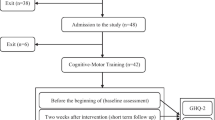
A total number of 48 patients with a diagnosis of definite MS (McDonald’s criteria revised by Polman) [23] and age up to 65 years, who attended the MS Clinic of “Santa Lucia” Foundation and the outpatient service of the “Filippo Turati” Foundation, were consecutively enrolled in this study. pMS could be either suffering from relapsing–remitting (RRMS) or secondary-progressive (SPMS) courses diagnosed by a certified neurologist. To be included in the sample, all participants had to be native Italian speakers and to have no pathological condition (such as neurological or psychiatric pathologies) other than MS severe enough to interfere with cognitive functioning. pMS should have an Expanded Disability Status Scale (EDSS) [24] score lower or equal to 6.0. Furthermore, pMS with clinical relapses or undergoing steroid therapy during the 3 months prior to the enrolment have not been considered as suitable. Current drug therapies for the treatment of the disease (e.g., Immunomodulatory drugs) have not constituted exclusion criteria, but have been taken into consideration during the statistical processing of the data, if necessary. pMS who had a clinical relapse or disease activity highlighted on MRI during the treatment period have been considered as drop-out. PMS with severe upper limb dysfunction like paralysis or tremor that were not able to hold the computer-mouse were excluded from the study. Similarly, at the beginning of the cognitive test visual acuity is assessed and pMS that could not read the instructions were excluded from performing the test. As we intended to consider the effect induced by each rehabilitation approach within patients, no specific disability level (both motor and/or cognitive) constituted exclusion criteria.
The study was approved by the local ethics committee (CE/PROG.698). The study was conducted from October 2018, and all data were collected till January 2020. All participants gave their written informed consent before taking part in the study. This study protocol was retrospectively registered in approved public trials registry (ClinicalTrial.gov ID: NCT05462678) and published elsewhere [25].
Assessment
After having confirmed their suitability for the study and having signed the informed consent, all participants underwent, in a 1-day session, a clinical and neuropsychological assessment, a complete motor assessment, and then were randomly assigned to one of the three treatment conditions with a simple randomization procedure. Each group was composed of 16 participants. The randomization procedure was followed by the project administrator with a random numeric sequence.
The clinical assessment was performed by a trained clinician who administered the EDSS and the multiple sclerosis functional composite (MSFC), composed by the timed 25-foot walk test (T25FT), the 9-hole peg test (9HPT), and the paced auditory serial addition test (PASAT) [26]. The neuropsychological assessment was performed by a trained psychologist and was composed by the Italian version of minimal assessment of cognitive functioning in multiple sclerosis (MACFIMS) [27, 28] and the multiple sclerosis neuropsychological questionnaire (MSNQ) [29]. pMS have also completed questionnaires for the assessment of depression (Beck Depression Inventory—BDI) [30] and anxiety (State Trait Anxiety Inventory—Y1 e Y2–STAY 1–2) [31]. The motor assessment was performed by a trained physiotherapist and included the 6-min walking test (6MWT) [32], the Tinetti Scale-gait and balance (TS-1; TS-2) [33], and the Berg Balance Scale (BBS) [34] for the assessment of gait and balance.
Procedures
For the aims of the study, we chose to use the Rehacom program for the CR (http://www.emsmedical.net) [35,36,37]. After the assessment and the randomization, each patient followed one of the three following training programs for a total of 12 weeks:
-
Reha1: the first group carried out a training of CR by three memory modules of the Rehacom program. Each patient performed two weekly sessions of 45 min each, for 12 weeks
-
Reha2: the second group followed a mixed training program with the use of the three memory modules of the Rehacom program combined with the MR training. Each patient performed one session per week (45 min) of CR and one session per week of traditional MR training for 12 weeks
-
Reha3: the third group carried out a traditional MR training through two weekly sessions, of 45 min each, for a total of 12 weeks
The complete assessment carried out at T0 has been performed again at the end of the rehabilitation program (T1).
REHACOM modules
RehaCom is a sophisticated software designed by clinicians and engineers for the treatment of CI resulting from numerous pathological states. It has been used in an increasing number of studies on CR in MS [36, 37], highlighting a significant efficacy in enhancing attention, information processing speed, executive functions [38], and memory [39]. RehaCom can be used in an acute stage of the pathology as well as throughout all stages of recovery. The software automatically adjusts to the patient’s performance level: the difficulty will only increase in response to improved performance while remaining challenging without becoming frustrating [40]. It has over 20 modules from which to choose the specific ones for the cognitive functions that you intend to enhance/rehabilitate. For each module, the therapist can select a certain number of variables (duration of the session, initial level of the session, choice of stimuli, time limits for the resolution of activities, etc.) that allow an individualized approach for each patient.
Memory deficit is one of the most common CI observed in pMS, with a prevalence of 40–65%, with 30% of patients presenting severe deficits [41]. In most cases, long-term memory [13] and working memory are compromised [42]. For the aim of the study, we decided to use three memory modules of the Rehacom program focused to the memory components most frequently involved in MS-related impairment [43]. In particular, three modules of the Rehacom software were used, specific for long-term, short-term, and working memory deficits:
-
Working memory (WOME) exercises the ability to memorize and manipulate information that does not or no longer exist in the patient “external environment”
-
Figural memory (BILD) is used for training long-term non-verbal and verbal memory
-
Verbal memory (VERB) aims to improve the short-term memory of verbal information by short stories displayed on the screen.
Statistical analysis
An a priori sample size analysis was performed to establish the adequate number of participants [44]. The statistic used was the ANOVA (repeated measures, within-between interaction), and the type of power analysis chosed was the A-priori: compure required sample size- given α, power, and effect size. Therefore, for three groups and 2 repeat evaluations, an effect size of 0.3, an α error probability of 0.05, and a power effect of 0.95, the minimum number of patients’ required was 48 (to be divided into three equivalent groups).
Demographic data were compared between the three pMS groups (Reha1, Reha2, and Reha3) with an independent sample T tests for age and education, and a chi-square test for gender. T tests were also used to test for group differences on cognitive, motor, and mood performance at T0. The normality of data distribution was studied by the Shapiro–Wilk test.
For the purposes of the study, different types of statistical analyses have been carried out.
-
Within-group analysis: these statistical analyses aimed at evaluating any improvement in pMS’ cognitive performance. Within each group of pMS, the assessments at T0 have been compared with that at T1 through a T test. Similarly, the same analyses were conducted to compare the levels of anxiety and depression and the self-perception of cognitive deficit.
-
Between-group analysis: these statistical analyses aimed at comparing the benefit obtained by each group from T0 to T1, with those of the other 2 groups. Therefore, for each scale, we derived a score which is the result of the difference resulting from the performance at T1 and that of T0. These variables were then compared between groups by using an ANOVA. In case of significance, post hoc tests were performed and Bonferroni correction was applied. Also in this case, the same comparative analyses were carried out on the following variables: levels of anxiety and depression and self-perception of cognitive difficulties.
To conclude, we also decide to explore the effect of the three types of training on the Cognitive Impairment Index (CII). The CII is an index of global cognitive impairment derived from the computation of the cognitive tests included in the Italian version of MACFIMS [29]. It is the sum of the degree of impairment on each of the 11 scales of the MACFIMS. With the CII, the percentage of pMS in the preserved, mild, or severe range of total CI was calculated.
Results
From the comparison analysis between groups at T0, no statistical difference was found between participants assigned to the three conditions for clinical variables and demographics (Table 1). Furthermore, a preliminar comparison analysis between the three groups was peformed for cognitive and motor efficiency scales in order to avoid baseline differences that may bias the results. By this analysis, no difference in any motor or cognitive variable was found between the three groups.
Table 2 shows the results of the within-group analysis. For each group, pre- and post-data were expressed in terms of mean and standard deviation with the relative level of significance. Concerning cognitive aspects, as reported in Table 2, pMS in the Reha1 group had significant better performances on PASAT (p = 0.012), CVLT_IR (p = 0.043), BVMTR_DR (p = 0.015), and an improvement in the CII (p = 0.050). Reha2 group increase the performance on CVLT_IR (p = 0.050) and BVMTR_IR (p = 0.048), while no benefit was found in the Reha3 group for cognitive aspects.
The motor performance of Reha2 also gained a benefit on TS (p = 0.034) and on BBS (p = 0.039). pMS in the Reha3 group showed a better performance on T25FW (p = 0.039) and on BBS (p = 0.003). No significant improvement was found for pMS in the Reha1 group for motor aspects (Table 3).
Mood and self-perceived cognitive deficit were not significantly different in the pre- and post-treatment for any condition and between groups (Table 2c; Table 3c).
Table 4 shows the results of the between-group analysis. As reported in the Table 4, by the between groups ANOVA, a statistical significant difference was found between the three groups in the benefit obtained by the treatment for SDMT (p = 0.009) and the total CII (p = 0.031). For the first variable, the significant difference in the benefit obtained was due to the comparison between Reha1 and Reha2 (p = 0.045) with Reha2 having a positive increase in SDMT score and Reha1 having a worsening performance. Similarly, for CII, the significant difference obtained is due from the comparison of Reha1 and Reha3 with the formers obtaining a worsening perfromance from T0 to T1 (p = 0.027).
As shown in the Table 5, with the same analysis between the three groups in the benefit obtained by the treatment, a significant difference for TS gait scale (p = 0.001) and for BBS (p = 0.008) was found. For the former, the difference in post hoc analysis was found to be due to the comparison between Reha1 and Reha2 with the second group showing a better effect of the training compared to the first (p = 0.019). The latter variable in the post hoc analysis was found to be due to the comparison between the performance of Reha2 and Reha3 (p = 0.007) with Reha2 having an higher benefit compared to Reha3.
Discussion
Actually, the possible options for the management of cognitive dysfunctions in MS are pharmacological interventions, CR and MR: all these approaches may be applied separately or as a part of a multimodal program. In clinical practice, multimodal programs are infrequently performed and pMS are primarily treated via pharmacological approach and subsequently via motor exercise training (physiotherapy). CR remains an infrequent approach to pMS.
Recent studies suggest the potential role of MR as a disease-modifying treatment, due to the induction of selective resting-state functional thalamo-cortical connectivity leading to cognitive processing speed improvements [45].
Furthermore, recent data on the onset of cognitive deficits suggest the existence of a 5-year window during which pMS can benefit more from interventions to maintain cognitive health [46]. Therefore, we believe that including CR into routine clinical rehabilitative practice, may significantly impact on the subsequent development of CI in this clinical population. In fact, CR, as a structured set of therapeutic activities, can both be used to prevent to- and to recover from- cognitive impairment [47].
It is possible that the association of CR with MR could give a double advantage to pMS: make them more autonomous in daily motor activities (promoting balance in more complex real-life activities and reducing falls’ risks and occurrence with their consequences) and in daily life activities management (in both domestic and work environments). This would also have the secondary benefit of lightening the burden of caregivers and reduce the economic and social costs of the disease.
The results of the actual study show that the group of pMS who underwent Reha1 had a significant improvement of cognitive performances (especially those specifically treated by the program, that is memory functions). As expected, these pMS did not show any benefit on the untreated motor functions. The opposite pattern was found in the Reha3 group who performed MR only. These pMS, in fact, significantly improved the performances on gait and balance parameters but showed no significant improvement on cognitive performances. These two groups’ results confirmed the efficacy of both cognitive and motor rehabilitation administered alone, in a focused program, as widely reported in the literature. Particularly interesting is that pMS who received a combined treatment (Reha2) improved both cognitive performances (especially, memory functions) and static/dynamic balance efficiency.
Of note, an higher benefit could be expected for other cognitive variables in the group of patients who only performed CR, but we should consider that patients were included in the study with moderately or no cognitive impairment so the margin for the improvement could not always be such as to achieve significance. This could be considered a limitation of the study from the one hand; from the other, we should consider that cognitive trainings could have the better benefits for patients in the early phases of impairment and a cognitive oriented training could give a benefit also in terms of brain stimulation. In these phases, a brain plasticity induced by treatments could hesitate in a functional reorganization.
The same explaination can be assigned for mood and MSNQ for which no significant difference between pre- and post-treatments has been obtained: in this case, we excluded patients with severe psychiatric conditions so the margin for change is significantly reduced. Furthermore, anxiety and depression are chronic conditions in pMS and may be linked to the instability of the disease. The MSNQ scores did not show any significance as well, but even a previous study has found that the self-report questionnaire of MSNQ is not sensitive for the detection of neuropsychological impairment [48].
Concerning the ANOVA analysis, the results reported in Table 4 showed that, after rehabilitation, pMS in Reha2 obtained a processing speed efficiency improvement significantly higher than the group who followed a CR training. Again the Reha2 group benefit was significantly higher than that obtained in Reha1 and Reha3 for gait efficiency.
These results show that even patients with mild or moderate MS-related impairment can have a higher benefit from the integration of motor and cognitive trainings; this is probably due to the concurrent stimulation of brain circuits involved in the two functions: their overlap may favour a more efficient brain reorganization.
It has been demonstrated that goal-oriented locomotion is not a purely automatic process but requires the involvement of higher-order cognitive processes: this highlights the strong relationship between motor and cognitive functioning [22, 49]. In this regard, the separate assessment of cognitive abilities and walking skills may not reflect reality as, usually, people perform a motor task simultaneously with a cognitive task in the so-called “dual tasking” condition [17]. The limited capacity of executive functions can generate cognitive-motor interferences [49] and a loss of efficacy in one or both tasks [50]. Mutual interference/facilitation may justify the results of our study. Therefore, integrated rehabilitation strategies may be used alternatively or in association with motor and cognitive rehabilitation alone [51].
The Italian validation of MACFIMS gives the possibility to describe degrees of global CI [28]: we have used the CII to establish the cognitive benefit obtained by pMS after the three kinds of rehabilitative approaches. Both Reha1 and Reha2 groups had a higher number of participants who were cognitively preserved after the treatment program and a very lower number of participants who remained severely impaired (Fig. 1). As expected, these changes were not found in the Reha3 pMS. Again this data was supported by the results of the between group analysis with Reha1 having a significant improvement of CII compared to Reha3 (Table 4). The CII is a summary score of all the cognitive components examined by the MACFIMS; therefore, its improvement goes beyond that of the cognitive functions stimulated by the training. This improvement could be explained as the consequence of the benefit obtained by both an isolated cognitive intervention or a combined motor-cognitive one.
The concurrent stimulation of both motor and cognitive functions may give pMS a better outcome in everyday life. We have maintained the same number of sessions and the same duration for each session: benefits have been obtained even when the time for cognitive and motor training was halved: in Reha1 and Reha3, pMS underwent 24 sessions of 45 min of cognitive or motor treatment, and in the Reha2, they did 12 sessions of 45 min of cognitive training and 12 sessions of 45 min of motor training.
These preliminary results need to be confirmed by a trial with a wider sample and more intensive treatments, but they represent, however, an encouraging incentive to perform other studies taking into account long-term effects with follow-up of adequate duration [47]. It could be important in future studies to explore the time duration of the benefits obtained by the three rehabilitation approaches across the time, by re-assess participants at 6 and 12 months after the end of the rehabilitation sessions. In this study, we could not assess this effect as, according to the period in which we concluded T1 assessments, the COVID-19 pandemic imposed restrictions and biases that could have interfered with the reliabilty of the results. Furthermore, it would be interesting to investigate the influence of other variables, such as cognitive reserve, on rehabilitation outcomes. Future studies will overcome these limitations.
Conclusions
In conclusion, notwithstanding the relevance of cognitive functioning and the frequent occurrence of CI in pMS, at the moment, there is a widely spread difficulty both in accessing to CR and in having continuity. In fact, CR is easily warranted by the Italian Health System in the rehabilitative care unit as part of the Integrated Rehabilitation Plan after an acute neurological disorder, or in other multidisciplinary contexts, in which specialized figures (such as physician, psychologist/neuropsychologist) cooperate. Nevertheless, these centers are not ubiquitously distributed on the national territory, as it happens for the MR. Therefore, pMS who need rehabilitation of cognitive functions, are forced to undergo private access treatments, with a relevant economic burden. This study underline that rehabilitation approaches integrating CR and MR could give an advantage in the improvement of MS-related symptoms with a double benefit in a shorter time frame in comparison with performing them separately. We could state that we do not need to give patients two separate rehabiltiations when we can only integrate cognitive training in motor one. This could result in saving time, costs, and clinical resources.
Data Availability
The data supporting findings of this study are available from the corresponding author upon reasonable request.
Change history
20 January 2023
A Correction to this paper has been published: https://doi.org/10.1007/s10072-023-06630-1
References
Argento O, Nocentini U (2019) Neuropsychological assessment in multiple sclerosis. In: El-Baz A, Suri JS (eds) Neurological disorders and imaging physics, volume 2; engineering and clinical perspectives of multiple sclerosis. IOP Publishing
Maggio MG, Russo M, Cuzzola MF, Destro M, La Rosa G, Molonia F, Bramanti P, Lombardo G, De Luca R, Calabrò RS (2019) Virtual reality in multiple sclerosis rehabilitation: a review on cognitive and motor outcomes. J Clin Neurosci 65:106–111. https://doi.org/10.1016/j.jocn.2019.03.017
Kasser SL, Jacobs JV, Foley JT, Cardinal BJ, Maddalozzo GF (2011) A prospective evaluation of balance, gait, and strength to predict falling in women with multiple sclerosis. Arch Phys Med Rehabil 92:1840–1846. https://doi.org/10.1016/j.apmr.2011.06.004
Argento O, Incerti CC, Pisani V, Magistrale G, Di Battista G, Romano S, Ferraro E, Caltagirone C, Nocentini U (2014) Domestic accidents and multiple sclerosis: an exploratory study of occurrence and possible causes. Disabil rehabil 36:2205–2209. https://doi.org/10.3109/09638288.2014.895429
Barbarulo AM, Lus G, Signoriello E, Trojano L, Grossi D, Esposito M, Costabile T, Lanzillo R, Saccà F, Morra VB, Conchiglia G (2018) Integrated cognitive and neuromotor rehabilitation in multiple sclerosis: a pragmatic study. Front Behav Neurosci 12:196. https://doi.org/10.3389/fnbeh.2018.00196
Amatya B, Khan F, Galea M (2019) Rehabilitation for people with multiple sclerosis: an overview of Cochrane Reviews. Cochr Database Syst Rev (1). https://doi.org/10.1002/14651858.CD012732.pub2
Kesselring J, Beer S (2005) Symptomatic therapy and neurorehabilitation in multiple sclerosis. Lancet Neurol 4:643–652. https://doi.org/10.1016/S1474-4422(05)70193-9
Beer S, Khan F, Kesselring J (2012) Rehabilitation interventions in multiple sclerosis: an overview. J Neurol 259:1994–2008. https://doi.org/10.1007/s00415-012-6577-4
Amato MP, Morra VB, Falautano M, Ghezzi A, Goretti B, Patti F, Mattioli F (2018) Cognitive assessment in multiple sclerosis—an Italian consensus. Neurol Sci 39:1317–1324. https://doi.org/10.1007/s10072-018-3427-x
Fenu G, Fronza M, Lorefice L, Arru M, Coghe G, Frau J, Marrosu MG, Cocco E (2018) Performance in daily activities, cognitive impairment and perception in multiple sclerosis patients and their caregivers. BMC Neurol 18:212. https://doi.org/10.1186/s12883-018-1224-z
Amato MP, Portaccio E, Zipoli V (2006) Are there protective treatments for cognitive decline in MS? J Neurol Sci 245:183–186. https://doi.org/10.1016/j.jns.2005.07.017
Goretti B, Portaccio E, Zipoli V, Hakiki B, Siracusa G, Sorbi S, Amato MP (2009) Coping strategies, psychological variables and their relationship with quality of life in multiple sclerosis. Neurol Sci 30:15–20. https://doi.org/10.1007/s10072-008-0009-3
Brochet B, Ruet A (2019) Cognitive impairment in multiple sclerosis with regards to disease duration and clinical phenotypes. Front neurol 10:261. https://doi.org/10.3389/fneur.2019.00261
Chiaravalloti ND, DeLuca J (2008) Cognitive impairment in multiple sclerosis. Lancet Neurol 7:1139–1151. https://doi.org/10.1016/S1474-4422(08)70259-X
Rocca MA, Amato MP, De Stefano N, Enzinger C, Geurts JJ, Penner IK (2015) MAGNIMS Study Group. Clinical and imaging assessment of cognitive dysfunction in multiple sclerosis. Lancet Neurol 14:302–317. https://doi.org/10.1016/S1474-4422(14)70250-9
Nocentini U, Caltagirone C, Tedeschi G (Eds.) (2012) Neuropsychiatric dysfunction in multiple sclerosis. Springer Science & Business Media
Leone C, Patti F, Feys P (2015) Measuring the cost of cognitive-motor dual tasking during walking in multiple sclerosis. Mult Scler 21:123–131. https://doi.org/10.1177/1352458514547408
Benedict RH, Amato MP, DeLuca J, Geurts JJ (2020) Cognitive impairment in multiple sclerosis: clinical management, MRI, and therapeutic avenues. The Lancet Neurology 19(10):860–871
Chiaravalloti ND, Moore NB, Nikelshpur OM, DeLuca J (2013) An RCT to treat learning impairment in multiple sclerosis: the MEMREHAB trial. Neurol 81:2066–2072. https://doi.org/10.1212/01.wnl.0000437295.97946.a8
Mattioli F, Stampatori C, Bellomi F, Danni M, Compagnucci L, Uccelli A, Pardini M, Santuccio G, Fregonese G, Pattini M, Allegri B, Clerici R, Lattuada A, Montomoli C, Corso B, Capra R (2015) A RCT comparing specific intensive cognitive training to aspecific psychological intervention in RRMS: the SMICT study. Front Neurol 5:278. https://doi.org/10.3389/fneur.2014.00278
Motl RW, Sandroff BM, DeLuca J (2016) Exercise training and cognitive rehabilitation: a symbiotic approach for rehabilitating walking and cognitive functions in multiple sclerosis? Neurorehabil Neural Repair 30:499–511. https://doi.org/10.1177/1545968315606993
Argento O, Spanò B, Pisani V, Incerti CC, Bozzali M, Foti C, Nocentini U (2021) Dual-task performance in multiple sclerosis’ PMS: cerebellum matters? Arch Clin Neuropsychol 36:517–526. https://doi.org/10.1093/arclin/acaa089
Polman CH, Reingold SC, Banwell B, Clanet M, Cohen JA, Filippi M, Fujihara K, Havrdova E, Hutchinson M, Kappos L, Lublin FD, Montalban X, O’Connor P, Sandberg-Wollheim M, Thompson AJ, Waubant E, Weinshenker B, Wolinsky JS (2011) Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol 69:292–302. https://doi.org/10.1002/ana.22366
Kurtzke JF (1983) Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurol 33:1444–1452. https://doi.org/10.1212/wnl.33.11.1444
Argento O, Piacentini C, Bossa M, Caltagirone C, Santamato A, Saraceni V, Nocentini U (2022) Study protocol: strategies and techniques for the rehabilitation of cognitive and motor deficits in patients with multiple sclerosis. NeuroSci 3:395–407
Fischer JS, Rudick RA, Cutter GR, Reingold SC, National MS Society Clinical Outcomes Assessment Task Force (1999) The Multiple Sclerosis Functional Composite measure (MSFC): an integrated approach to MS clinical outcome assessment. Mult Scler. 5:244–250. https://doi.org/10.1177/135245859900500409
Benedict RH, Cookfair D, Gavett R, Gunther M, Munschauer F, Garg N, Weinstock-Guttman B (2006) Validity of the minimal assessment of cognitive function in multiple sclerosis (MACFIMS). J Int Neuropsychol Soc 12:549–558. https://doi.org/10.1017/s1355617706060723
Argento O, Incerti CC, Quartuccio ME, Magistrale G, Francia A, Caltagirone C, Nocentini U (2018) The Italian validation of the minimal assessment of cognitive function in multiple sclerosis (MACFIMS) and the application of the Cognitive Impairment Index scoring procedure in MS patients. Neurol Sci 39:1237–1244. https://doi.org/10.1007/s10072-018-3417-z
Benedict RH, Munschauer F, Linn R, Miller C, Murphy E, Foley F, Jacobs LJMSJ (2003) Screening for multiple sclerosis cognitive impairment using a self-administered 15-item questionnaire. Mult Scler 9:95–101. https://doi.org/10.1191/1352458503ms861oa
Beck AT, Steer RA, Brown G (1996) Beck depression inventory–II. Psychological Assessment
Spielberger CD (1983) Manual for the State-Trait Anxiety Inventory (Form Y) (‘Self-Evaluation Questionnaire’). Consulting Psychologists Press; Palo Alto, CA
Enright PL (2003) The six-minute walk test. Respir Care 48:783–785
Tinetti ME (1986) Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc 34:119–126. https://doi.org/10.1111/j.1532-5415.1986.tb05480.x
Berg KO, Wood-Dauphinée S, Williams JI, Maki B (1992) Measuring balance in the elderly: validation of an instrument. Can J Public Health 83:7-S11
EMS sistemi elettromedicali. Available online: URL:http://www.emsmedical.net.
Mattioli F, Stampatori C, Zanotti D, Parrinello G, Capra R (2010) Efficacy and specificity of intensive cognitive rehabilitation of attention and executive functions in multiple sclerosis. J Neurol Sci 288:101–105. https://doi.org/10.1016/j.jns.2009.09.024
Cerasa A, Gioia MC, Valentino P, Nisticò R, Chiriaco C, Pirritano D, Tomaiuolo F, Mangone G, Trotta M, Talarico T, Bilotti G, Quattrone A (2013) Computer-assisted cognitive rehabilitation of attention deficits for multiple sclerosis: a randomized trial with fMRI correlates. Neurorehabil Neural Repair 27:284–295. https://doi.org/10.1177/1545968312465194
Mattioli F, Stampatori C, Scarpazza C, Parrinello G, Capra R (2012) Persistence of the effects of attention and executive functions intensive rehabilitation in relapsing remitting multiple sclerosis. Multiple sclerosis and related disorders 1(4):168–173
Ernst A, Botzung A, Gounot D, Sellal F, Blanc F, De Seze J, Manning L (2012) Induced brain plasticity after a facilitation programme for autobiographical memory in multiple sclerosis: a preliminary study. Mult Scler Int. https://doi.org/10.1155/2012/820240
Campbell J, Langdon D, Cercignani M, Rashid W (2016) A randomised controlled trial of efficacy of cognitive rehabilitation in multiple sclerosis: a cognitive, behavioural, and MRI study. Neur Plast 2016. https://doi.org/10.1155/2016/4292585
Oreja-Guevara C, Ayuso Blanco T, Brieva Ruiz L, Hernández Pérez MÁ, Meca-Lallana V, Ramió-Torrentà L (2019) Cognitive dysfunctions and assessments in multiple sclerosis. Front Neurol 10:581
Guimarães J, Sá MJ (2012) Cognitive dysfunction in multiple sclerosis. Front Neurol 3:74
Amato MP, Portaccio E, Goretti B, Zipoli V, Hakiki B, Giannini M et al (2010) Cognitive impairment in early stages of multiple sclerosis. Neurol Sci 31(2):211–214. https://doi.org/10.1007/s10072-010-0376-4
Faul F, Erdfelder E, Buchner A, Lang AG (2009) Statistical power analyses using G* Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41(4):1149–1160
Sandroff BM, Wylie GR, Sutton BP, Johnson CL, DeLuca J, Motl RW (2018) Treadmill walking exercise training and brain function in multiple sclerosis: preliminary evidence setting the stage for a network-based approach to rehabilitation. Mult Scler J–Exp Trans Clin 4(1):2055217318760641. https://doi.org/10.1177/2055217318760641
Achiron A, Chapman J, Magalashvili D, Dolev M, Lavie M, Bercovich E et al. (2013) Modeling of cognitive impairment by disease duration in multiple sclerosis: a cross-sectional study. PloS One 8(8):e71058. https://doi.org/10.1371/journal.pone.0071058
Lincoln NB, Bradshaw LE, Constantinescu CS, Day F, Drummond AE, Fitzsimmons D, das Nair R (2020) Group cognitive rehabilitation to reduce the psychological impact of multiple sclerosis on quality of life: the CRAMMS RCT. Health Technol Assess 24:1–182. https://doi.org/10.3310/hta24040
O’Brien A, Gaudino-Goering E, Shawaryn M, Komaroff E, Moore NB, DeLuca J (2007) Relationship of the Multiple Sclerosis Neuropsychological Questionnaire (MSNQ) to functional, emotional, and neuropsychological outcomes. Arch Clin Neuropsychol 22:933–948. https://doi.org/10.1016/j.acn.2007.07.002
Yogev-Seligmann G, Hausdorff JM, Giladi N (2008) The role of executive function and attention in gait. Mov Disord 23:329–342. https://doi.org/10.1002/mds.21720
Leone C, Feys P, Moumdjian L, D’Amico E, Zappia M, Patti F (2017) Cognitive-motor dual-task interference: a systematic review of neural correlates. Neurosci Biobehav Rev 75:348–360. https://doi.org/10.1016/j.neubiorev.2017.01.010
Learmonth YC, Pilutti LA, Motl RW (2015) Generalised cognitive motor interference in multiple sclerosis. Gait Posture 42:96–100. https://doi.org/10.1016/j.gaitpost.2015.04.014
Acknowledgements
We thank all patients and healthy subjects for their willing participation in the study.
Funding
This research was funded by the “Filippo Turati” Foundation with a 1-year direct scholarship to O.A (scholarship grant FTO.1) and by the Italian National Health System (SSN; SS 2018–2020 Clinical Neuroscience and Neurodegeneration—CNN; Brain Disorders and Clinical Neuroscience-IRG).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Saraceni and Dr. Santamato are part of the Scientific Direction of “Filippo Turati” Foundation who financed 1 year scholarship of the first author of this study. The other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The above article was published with error in author names. Family names was captured first instead of the given names. Thus, author names have been inverted in all the principal sites.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Argento, O., Piacentini, C., Bossa, M. et al. Motor, cognitive, and combined rehabilitation approaches on MS patients’ cognitive impairment. Neurol Sci 44, 1109–1118 (2023). https://doi.org/10.1007/s10072-022-06552-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-06552-4