Abstract
Aims
The objective of the present study was to evaluate sleep features and sleep-modifying factors in patients with chronic migraine (CM) during the first Italian COVID-19 lockdown.
Material and methods
The study was based on an e-mail survey addressed to CM patients of our headache center. The survey investigated demographic, life-style, sleep, psychological, and migraine features during the first COVID-19 lockdown period and the month before. The outcomes were sleep quality (measured using PSQI) and variation in sleep quality, duration, and latency.
Results
Ninety-two patients were included. The mean PSQI was 11.96. Sleep quality was improved in 14.1%, stable in 47.8%, and worsened in 38.0%. Sleep latency was reduced in 5.4%, stable in 46.7%, and increased in 47.8%. Sleep duration was reduced in 29.3%, stable in 34.8%, and increased in 35.9%. Significant associations were found with age, work/study, remote working, job loss, meal quality change, smoking variation, COVID-19 province prevalence, home-inhabitant relationship, ratio of house size/number of people, stress, state anxiety, anxiety/depression variation, future concern variation, computer hours, internet hours, and television hours.
Conclusion
The study described sleep features of chronic migraineurs during COVID-19 lockdown, pinpointing the main factors involved in sleep quality and sleep changes. Our findings revealed that migraineurs’ sleep was closely linked with life-style and psychological features. Several modifiable factors came to light and they should be considered in order to develop an optimal management of CM. An appropriate and more aware treatment of sleep problems could be a way to improve migraineurs’ life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Migraine and sleep are closely associated and their relationship is highlighted by a large body of literature [1,2,3]. A sleep disturbance can precede and predict new onset migraine several years ahead, patients frequently report insomnia in the night before an early morning migraine attack, and sleep disorders are associated with more severe migraine and headache chronification [1, 2, 4, 5]. Chronic migraineurs, especially, have a higher risk of sleep disorders and are more influenced by these [2]. The association between migraine and sleep was further highlighted by several studies during the COVID-19 lockdown. Lockdown measures determined important migraine changes that were attributed to different factors, in particular sleep problems and sleep changes during this period [6,7,8,9,10,11]. Studying sleep in migraineurs constituted a way in order to better understand migraine and how to relieve it. Although several papers reported the relationship between migraine and sleep in the COVID-19 lockdown, no study has investigated which factors determined sleep quality and sleep modification in migraineurs during this period. The aim of this study is to bridge this gap, analyzing sleep and sleep-modifying factors in chronic migraineurs.
Methods
The present work is based on data obtained for a previous study on chronic migraine during the COVID-19 lockdown. The data were collected using an e-mail survey addressed to patients suffering from chronic migraine followed at our headache center. More detailed information is available in the previous paper [10]. The questionnaire is available on supplementary materials (S1, S2). The present study investigated sleep quality and sleep changes in chronic migraineurs during the previous month and the Italian COVID-19 lockdown period which went from March 9th, 2020 to May 3rd, 2020. The survey started on April 24th, 2020 and closed on May 3rd, 2020.
Inclusion criteria
Patients were selected according to the following criteria:
-
chronic migraine diagnosis based on International Classification of Headache Disorders, third edition criteria [12]
-
age ≥ 18 years
-
written informed consent to participate to the study
Data included in the study
Information on demographic features, life-style, sleep, migraine, and psychological status was extracted from our survey.
The demographic and life-style variables included age, gender, educational qualifications, number of sons/daughters, age of sons/daughters, COVID-19 prevalence in patients’ province, size of the house, rent or mortgage to pay, number of people in house, ratio of house size/number of people, living with parents, quality of home-inhabitant relationship, unemployment, work/study stop, remote working (RW), job loss during the COVID-19 pandemic, hours of computer use, changes in duration of computer use, hours of smartphone use, changes in duration of smartphone use, hours of Internet use, changes in duration of the internet use, hours of television viewing, changes in duration of television viewing, coffee consumption, change in coffee consumption, quality variation of nutrition, variation of meal regularity, smoking, variation of smoking habit, times a day to research information about on COVID-19, times a day to go outside, perceived reduction of noise pollution, and COVID-19 infection.
The sleep data were the Pittsburgh Sleep Quality Index score (PSQI, used to evaluate sleep quality, the score ranges from 0 to 21, a higher score is associated with a worse condition), perceived variation of sleep quality, change in sleep duration (sleep duration defined as hours of actual sleep), and variation of sleep latency (sleep latency defined as the period from lights out to sleep onset).
The following migraine information was evaluated: migraine familiarity, anti-migraine drug overuse history, migraine with aura, age of onset, age of migraine chronification, and discontinuation of the therapy performed within the headache center (botulinum toxin or monoclonal antibodies) due to lockdown.
Regarding psychological status, the following data were analyzed: Beck Depression Inventory score (BDI, measures the severity of depression, score ranges from 0 to 63, a higher score is associated with a worse condition), State-Trait Anxiety Inventory score (STAI, evaluates anxiety through two different scores, one for the trait anxiety, one for the state anxiety, each one ranges from 20 to 80 and a higher score is associated with a higher anxiety level), variation in perceived anxiety/depression, perceived stress scale score (PSS, asses perceived stress, it ranges from 0 to 40 and a higher score is associated with higher stress perception), variation in perceived stress, concern for the future during lockdown, variation of concern for the future, and concern for COVID-19.
Study outcomes
Every included variable was referred to the following outcomes:
-
• Sleep quality measured by PSQI
-
• Perceived variation of sleep quality
-
• Change in sleep duration
-
• Variation of sleep latency
Ethics
This study was conducted according to the guidelines laid down in the Declaration of Helsinki. Ethics approval was obtained from the local institutional review board and written informed consent was obtained from patients.
Statistical analysis
All statistical analyses were performed using R software. Continuous variables were expressed as mean ± standard deviation; categorical variables were expressed as absolute frequencies and percentages. Continuous variables were analyzed by the Shapiro–Wilk test to evaluate normal distribution. Mann–Whitney U or Student’s t-test for independent samples was used for comparison between categorical variables with two levels and continuous variables as appropriate. ANOVA test or Kruskal–Wallis test was used for comparison between categorical variables with > 2 levels and continuous variables on the basis of normal distribution. The chi-square test was used for comparison between categorical variables. The method of partitioning the degrees of freedom was applied to refuse H0 hypothesis as appropriate. Spearman’s rank or Pearson’s correlation coefficient was used for comparison between continuous variables as appropriate.
The multivariate analysis was performed using multiple linear regression or the binomial logistic regression model as appropriate. Regarding perceived variation of sleep quality, we built two different models. In the first model, “improved” and “no change” categories were unified; in the second model, “worsened” and “no change” categories were unified. Regarding the variation of sleep time duration and the variation of sleep latency, we also created two models. In one model, “reduction” and “no variation” groups were unified; in another model, “increase” and “no variation” groups were joined together. We built these models in order to perform the logistic regression analyses. A value of P < 0.05 was considered significant.
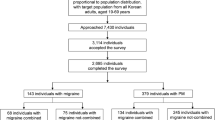
Results
Ninety-two patients suffering from chronic migraine were included in the present study. The mean age was 42.2 years; 42.2% of patients were ≤ 40 years old. 85.9% of migraineurs were female. The mean PSQI was 11.96 during the lockdown. Sleep quality between the previous month and lockdown was improved in 14.1%, stable in 47.8%, and worsened in 38.0%. Sleep latency was reduced in 5.4%, stable in 46.7%, and increased in 47.8%. Sleep time was reduced in 29.3%, stable in 34.8%, and increased in 35.9%. Sleep data are reported in Table 1 and Fig. 1. Demographic, life-style, migraine, and psychological data are reported in Tables 2 and 3.
Influences of demographic, life-style, psychological, and migraine features on sleep
PSQI
A higher PSQI was associated with a smaller house size, a lower ratio of house size/number of people, home-inhabitant relationship quality, unemployment, continuing to work or study during lockdown, meal regularity changes, migraine with aura, depression, anxiety/depression increase, higher STAI-S score, higher STAI-T score, higher PSS score, stress increase, higher future concern, and increase in concern for the future (Table 4).
On multivariate analysis, only ratio of house size/number of people, STAI-S score, and increase in future concern remained significant.
Variation of sleep quality
The variation of sleep quality was related with rent/mortgage, home-inhabitant relationship, work/study during lockdown, computers hours, smartphone hours, meal quality, BDI, anxiety/depression variation, PSS, and perceived stress variation (Table 5).
Multivariate analysis showed that:
-
sleep quality increase was related with very good home-inhabitant relationship and lower stress levels.
-
sleep quality reduction was associated with work/study during lockdown, five or more hours on computer, and increased anxiety/depression.
Change in sleep duration
The change in sleep duration was associated with age, educational levels, stop working/studying during lockdown, job loss, number of computer hours, changes in computer hours, number of smartphone hours, variation in smartphone hours, number of internet hours, internet hours variation, change in television hours, changes in coffee consumption, meal quality change, time to focus on COVID-19 news, age of migraine chronification, PSS, perceived stress variation, and change in concern for the future (Table 5).
Multivariate analysis confirmed that:
-
an increased sleep time was related with younger age, stop to work/study during lockdown, an increase in television hours, and no variation/reduction in concern for the future.
-
a reduction in sleep time was linked with no job loss, five or more hours on computer, an increase in internet hours, and high-moderate PSS score.
Variation of sleep latency
The variation of sleep latency was associated with COVID-19 prevalence in patients’ province, remote working, computer hours, meal quality, and smoke variation (Table 5).
Multivariate analysis showed that:
-
an increased latency was linked with low COVID-19 prevalence and a change in meal quality.
-
a reduced latency was linked with remote working and increased smoking.
Discussion
Our patients presented globally a poor sleep quality during the lockdown as indicated by the high PSQI score. These data confirmed the close association of migraine with sleep, also in this peculiar period. The most respondents (47.8%) reported no sleep quality change but a consistent group (38.0%) presented a worsening, whereas 14.1% showed an improvement. Regarding the sleep latency, the most migraineurs (47.8%) had a time increment, a consistent group (46.7%) reported no changes, and only 5.4% experienced a reduction. The sleep time changes were more homogenous: 35.9% reported an increase, 34.8% no variations, and 29.3% a reduction. Several other studies investigated sleep features in migraineurs during COVID-19 lockdown. Smith et al. showed that patients suffering from migraine were more likely than non-migraine peers to have new or worsening sleep problems (48.5% vs 31.2%), and the younger people were more at risk [6]. In Al-Hashel and Ismail survey, 78.1% of the migraineurs reported sleep disturbance during the lockdown [9]. Munoz-Ceron et al. observed that sleep disturbances increased from 53.87 to 87.3% between lockdown week 0 and week 12 [13]. Di Stefano et al. showed a global worsening of sleep quality, evaluated using the Insomnia Severity Index: migraineurs had a pre-lockdown score of 7 and a lockdown score of 8 [8]. In Japanese migraineurs, a sleep quality worsening was also reported, although it was lower than other studies [7]. Gonzalez-Martinez et al. reported that 80.6% of their patients experienced a sleep change and insomnia increased from 48.6 to 70.3% between pre-lockdown and lockdown period [11]. Delussi et al. showed a sleep quality improvement in 36.3% of their migraineurs, a worsening in 10.4%, and no change in 52.9%. It is important to highlight that we observed a lower improvement rate and a higher percentage of worsening than Delussi et al. The same difference was reported for migraine changes between their study and our previous work [10]. These diverse trends could be explained through the different interview time. Our survey was started on April 24th and was closed on May 3rd, and theirs between March 27th and April 18th. Delussi et al. attributed migraine improvement to patients’ resilience [21] that could have also led to sleep improvement. This resilience could have been eroded by time, justifying the difference between our and their results. Another substantial difference was that our patients were all chronic migraineurs, whereas most patients of Delussi et al. suffered from episodic migraine: the chronic migraineurs represented a frailer population and they had an increased sleep vulnerability [2].
In the present study, sleep quality and sleep changes were associated with several elements: from age to work, from life-style to psychological features.
A younger age was associated with an increased sleep time. The same association was seen in another study on general population in Argentina during the lockdown [14]. This element is in line with the natural tendency of young people to sleep more hours [15]. They took advantage of the lockdown to adjust their sleep habits according to their biological need. Lockdown probably represented an opportunity for many young people to indulge their physiological rhythms by having to work and study from home or not work at all.
Our study showed that computer and internet use had a negative impact on sleep: five or more hours on computer were related with a reduction in sleep time and quality; an increase in internet use was linked with a decrease in sleep time. Salfi et al. showed in the general population during lockdown that an increased electronic device usage led to a sleep worsening [16]. These results are in accordance with a large body of literature that related increased screentime prior to bedtime with sleep alterations [17,18,19,20,21,22]. This association is probably due to an alteration of melatonin secretion, sleep displacement, and an excessive exposition to excitatory contents. On the other hand, it is interesting to observe that increased television use was associated with more sleep hours in our patients. Television is, probably, less interactive than other electronic devices, providing less excitatory stimuli. Its use could have been a way to get everyone closer to other family members/home inhabitant during the lockdown, watching together the same content, compared to a solitary use of the internet, computer, and smartphone. From this point of view, an increase in television use could have been a better coping strategy than an increase in the use of other electronic devices. Another important observation is that television is not generally accessible out of the home and its use could probably have been increased in different time slots during lockdown compared to smartphone and computer in our patients. In particular, its increase could have been mainly in the morning and in the afternoon when most people are usually out of the home, sparing the night time devoted to sleep. This difference could also explain the diverse sleep impact of television compared to the other electronic devices.
Regarding job/study, we found that unemployed people had a higher rate of sleep quality reduction, and migraineurs who stopped working/studying or lost their job during lockdown had the tendency to sleep more hours. The unemployed had a bad sleep quality, probably because they were more afraid of their economic condition and future, and a bad rest quality coupled with more free time led to sleep more. These data were in line with studies on the general population during lockdown that showed the unemployed were frequently poor sleepers [23, 24]. It is interesting to observe that remote working was associated with sleep latency reduction in our study. We previously described migraine benefit due to remote working [10]. Also in this case, the improvement could be explained through a better management of the time and the work with a habit reshaping that allow these workers to be more relaxed at bedtime. Our data diverged from Cellini et al. results on the general population that showed an increased latency in remote workers between pre-lockdown and lockdown period with a significant difference in the Italian but not in the Belgian group [25]. Another study on the general population observed that remote working was associated with a lower sleep latency compared to classical workers and the unemployed but without a significant value [26]. We found this association, probably because chronic migraineurs represented a vulnerable part of workers that could take more advantage of a work reorganization and a more autonomous management.
Stress, depression, and anxiety had significant impact on our patients’ sleep, highlighting a well-known association that was extensively studied in the general population during the lockdown [27]. Regarding anxiety, the sleep worsening was linked with state anxiety rather than trait anxiety. In the same way, there was an association with an increase in concern for the future, highlighting the deep psychological wound due to lockdown and pandemic. It is important to pinpoint that psychological features, sleep, and migraine are always strongly interconnected [2]. Psychological aspect should always be investigated and treated in migraineurs, especially in this particular period. A collaboration with professionals, such as psychologists and psychiatrists, could be useful in order to improve patients’ quality of life.
An important food for thought is offered by home-inhabitant relationship and ratio of house size/number of people. Migraineurs with a very good home-inhabitant relationship had an increased possibility of sleep quality improvement, underlining the importance of family support in lockdown. In the general population, Varma et al. and Xiao et al. showed how sleep quality was linked with loneliness and social capital (concept including social trust, belonging, and participation) [24, 28]. On the other hand, a low ratio of house size/number of people in our study was related with poor sleep quality, probably because having a small space to share with the other family members created more stressful conditions and problems with sleep repercussion. Furthermore, night noises could be more frequent, more easily perceived in a small space with many people and they could disturb home inhabitants’ sleep.
We also found a link between a lower COVID-19 prevalence and an increased sleep latency: it could be justified through an increased stress and aversion to lockdown that was seen as an excessive measure leading only economic and social damage in these areas. Salfi et al. had already reported that living in southern Italy was a predictor of sleep disturbance and this area was less affected by COVID-19 pandemic during the first lockdown whereas it was severely affected by economic crisis [23].
Regarding nutrition and smoking, our study highlighted two peculiar associations. Increased smoking was related with a reduction in sleep latency. Smoking is a well-known factor associated with sleep disturbances [29] but smoking more cigarettes probably constituted a valid coping strategy, allowing smokers to relieve stress in lockdown. Concerning nutrition, our results pointed out that migraineurs who maintained their meal quality had more chance of improving or preserving their sleep latency, suggesting a benefit in patients who had a stable nutrition in spite of the social earthquake due to lockdown.
Our study offered a cross-section of sleep in migraineurs during COVID-19 lockdown, pinpointing in particular the influence of life-style and psychological aspects. Some studies showed how cognitive-behavioral therapy for sleep disorders can improve both insomnia and migraine [2, 30,31,32]. This evidence and our results suggested that little changes in life-style habits and mental approach can have an important influence on sleep and migraine. There are many modifiable factors that should be taken into account and be object to specific treatment in a multidisciplinary context in order to improve life quality in migraineurs.
The present study has several limitations. The first limitation is the small number of patients. Second, cross-sectional design enabled us to relate sleep with several elements, without allowing us to determine the direction of many cause-effect relationships, but manifold associations were probably bidirectional (e.g., high stress could be a cause but also a consequence of sleep alteration). Third, a selection bias could be represented by non-response to the web survey. Fourth, we do not have standardized data in the pre-lockdown period, and we are based on patients’ perception and reporting. Fifth, many evaluated outcomes and variables have subjective characteristics and are prone to determine bias. In particular, some sleep parameters (latency, sleep time) could only be perceived as altered by the patients. Sixth, we did not specifically evaluate irregularities in circadian rhythms that may have played an important role in our patients during the lockdown. Lastly, the study in a single center may have affected the selection of patients.
Conclusions
The present study analyzed sleep features of chronic migraineurs during the first COVID-19 lockdown, pinpointing the main factors involved in sleep quality and sleep changes in this particular period. We found associations with several elements: from stress and depression to home-inhabitant relationship, from screentime exposure and remote working to nutrition and smoking habits. Our findings revealed that migraineurs’ sleep is closely linked with life-style and psychological features: there are several modifiable factors that should be considered in order to develop an optimal management of patients suffering from migraine. An appropriate and more aware treatment of sleep problems could be a way to improve migraineurs’ quality of life.
Availability of data and material
Derived data supporting the findings of this study are available from the corresponding author on request.
References
Cevoli S, Giannini G, Favoni V et al (2012) Migraine and sleep disorders. Neurol Sci 33:43–46. https://doi.org/10.1007/s10072-012-1030-0
Rains JC (2018) Sleep and migraine: assessment and treatment of comorbid sleep disorders. Headache 58:1074–1091. https://doi.org/10.1111/head.13357
Vgontzas A, Pavlović JM (2018) Sleep disorders and migraine: review of literature and potential pathophysiology mechanisms. Headache 58:1030–1039. https://doi.org/10.1111/head.13358
Ødegård SS, Sand T, Engstrøm M et al (2011) The long-term effect of insomnia on primary headaches: a prospective population-based cohort study (HUNT-2 and HUNT-3). Headache 51:570–580. https://doi.org/10.1111/j.1526-4610.2011.01859.x
Alstadhaug K, Salvesen R, Bekkelund S (2007) Insomnia and circadian variation of attacks in episodic migraine. Headache 47:1184–1188. https://doi.org/10.1111/j.1526-4610.2007.00858.x
Smith M, Nakamoto M, Crocker J, et al (2020) Early impact of the COVID‐19 pandemic on outpatient migraine care in Hawaii: results of a quality improvement survey. Headache J Head Face Pain 1–8. https://doi.org/10.1111/head.14030
Suzuki K, Takeshima T, Igarashi H et al (2021) Impact of the COVID-19 pandemic on migraine in Japan: a multicentre cross-sectional study. J Headache Pain 22:1–10. https://doi.org/10.1186/s10194-021-01263-1
Di Stefano V, Ornello R, Gagliardo A et al (2021) Social distancing in chronic migraine during the COVID-19 outbreak: results from a multicenter observational study. Nutrients 13:1–13. https://doi.org/10.3390/nu13041361
Al-Hashel JY, Ismail II (2020) Impact of coronavirus disease 2019 (COVID-19) pandemic on patients with migraine: a web-based survey study. J Headache Pain 21:115. https://doi.org/10.1186/s10194-020-01183-6
Currò CT, Ciacciarelli A, Vitale C et al (2021) Chronic migraine in the first COVID-19 lockdown: the impact of sleep, remote working, and other life/psychological changes. Neurol Sci. https://doi.org/10.1007/s10072-021-05521-7
Gonzalez-Martinez A, Planchuelo-Gómez Á, Guerrero ÁL et al (2021) Evaluation of the impact of the COVID-19 lockdown in the clinical course of migraine. Pain Med (United States) 22:2079–2091. https://doi.org/10.1093/pm/pnaa449
Headache Classification Committee of the International Headache Society (2018) The international classification of headache disorders, 3rd edition. Cephalalgia 38:1–211. https://doi.org/10.1177/0333102417738202
Munoz-Cerón J, Gallo L, Suarez J (2021) Clinical course of migraine during strict quarantine due to SARS-CoV-2: effect of psychiatric comorbidities in a clinical cohort. Eur Neurol 84:348–353. https://doi.org/10.1159/000516320
Leone MJ, Sigman M, Golombek DA (2020) Effects of lockdown on human sleep and chronotype during the COVID-19 pandemic. Curr Biol 30:R930–R931. https://doi.org/10.1016/j.cub.2020.07.015
Mander BA, Winer JR, Walker MP (2017) Sleep and human aging. Neuron 94:19–36. https://doi.org/10.1016/j.neuron.2017.02.004
Salfi F, Amicucci G, Corigliano D et al (2021) Changes of evening exposure to electronic devices during the COVID-19 lockdown affect the time course of sleep disturbances. Sleep 44:1–9. https://doi.org/10.1093/sleep/zsab080
Bhat S, Pinto-Zipp G, Upadhyay H, Polos PG (2018) “To sleep, perchance to tweet”: in-bed electronic social media use and its associations with insomnia, daytime sleepiness, mood, and sleep duration in adults. Sleep Heal 4:166–173. https://doi.org/10.1016/j.sleh.2017.12.004
Fossum IN, Nordnes LT, Storemark SS et al (2014) The association between use of electronic media in bed before going to sleep and insomnia symptoms, daytime sleepiness, morningness, and chronotype. Behav Sleep Med 12:343–357. https://doi.org/10.1080/15402002.2013.819468
Gamble AL, D’Rozario AL, Bartlett DJ et al (2014) Adolescent sleep patterns and night-time technology use: results of the Australian Broadcasting Corporation’s Big Sleep Survey. PLoS ONE 9:1–9. https://doi.org/10.1371/journal.pone.0111700
Hysing M, Pallesen S, Stormark KM et al (2015) Sleep and use of electronic devices in adolescence: results from a large population-based study. BMJ Open 5:1–7. https://doi.org/10.1136/bmjopen-2014-006748
Lastella M, Rigney G, Browne M, Sargent C (2020) Electronic device use in bed reduces sleep duration and quality in adults. Sleep Biol Rhythms 18:121–129. https://doi.org/10.1007/s41105-019-00251-y
Šmotek M, Fárková E, Manková D, Kopřivová J (2020) Evening and night exposure to screens of media devices and its association with subjectively perceived sleep: should “light hygiene” be given more attention? Sleep Heal 6:498–505. https://doi.org/10.1016/j.sleh.2019.11.007
Salfi F, Lauriola M, D’Atri A et al (2021) Demographic, psychological, chronobiological, and work-related predictors of sleep disturbances during the COVID-19 lockdown in Italy. Sci Rep 11:1–12. https://doi.org/10.1038/s41598-021-90993-y
Varma P, Burge M, Meaklim H, et al (2021) Poor sleep quality and its relationship with individual characteristics, personal experiences and mental health during the COVID‐19 pandemic. Int J Environ Res Public Health 18 https://doi.org/10.3390/ijerph18116030
Cellini N, Conte F, De Rosa O et al (2021) Changes in sleep timing and subjective sleep quality during the COVID-19 lockdown in Italy and Belgium: age, gender and working status as modulating factors. Sleep Med 77:112–119. https://doi.org/10.1016/j.sleep.2020.11.027
Lipert A, Musiał K, Rasmus P (2022) Working mode and physical activity as factors determining stress and sleep quality during COVID-19 pandemic lockdown in Poland. Life 12. https://doi.org/10.3390/life12010028
O’regan D, Jackson ML, Young AH, Rosenzweig I (2021) Understanding the impact of the COVID-19 pandemic, lockdowns and social isolation on sleep quality. Nat Sci Sleep 13:2053–2064. https://doi.org/10.2147/NSS.S266240
Xiao H, Zhang Y, Kong D et al (2020) Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in China. Med Sci Monit 26:1–8. https://doi.org/10.12659/MSM.923921
Amiri S, Behnezhad S (2020) Smoking and risk of sleep-related issues a systematic review and meta-analysis of prospective studies. Can J Public Heal 111:775–786. https://doi.org/10.17269/s41997-020-00308-3
Smitherman TA, Walters AB, Davis RE et al (2016) Randomized controlled pilot trial of behavioral insomnia treatment for chronic migraine with comorbid insomnia. Headache 56:276–291. https://doi.org/10.1111/head.12760
Smitherman TA, Kuka AJ, Calhoun AH et al (2018) Cognitive-behavioral therapy for insomnia to reduce chronic migraine: a sequential bayesian analysis. Headache 58:1052–1059. https://doi.org/10.1111/head.13313
Calhoun AH, Ford S (2007) Behavioral sleep modification may revert transformed migraine to episodic migraine. Headache 47:1178–1183. https://doi.org/10.1111/j.1526-4610.2007.00780.x
Acknowledgements
The first author would like to thank: Messina that is in the author’s heart and thoughts; Mirano, L.B. and his group for their warm welcome and the beautiful experience.
Author information
Authors and Affiliations
Contributions
C.C.T. developed the study design; C.C.T., A.C., and C.V. performed the data collection; T.G. performed the statistical analysis; A.T., M.A., G.V., P.L., and R.S. supervised the research; C.C.T., A.C., C.V., R.S., and M.A. wrote the article.
Corresponding author
Ethics declarations
Ethical approval
The research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The study protocol has been approved by the research institute’s committee on human research.
Consent to participate and for publication
All the patients have given their written informed consent.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Currò, C.T., Ciacciarelli, A., Vitale, C. et al. Sleep and sleep-modifying factors in chronic migraine patients during the COVID-19 lockdown. Neurol Sci 43, 6639–6655 (2022). https://doi.org/10.1007/s10072-022-06378-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-06378-0