Abstract
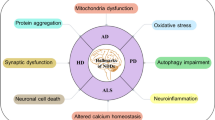
Neurological diseases (NDs) are one of the leading causes of disability and the second leading cause of death globally. Among these stroke, Alzheimer's disease (AD), and Parkinson's disease (PD) are the most common NDs. A rise in the absolute number of individuals affected with these diseases indicates that the current treatment strategies in management and prevention of these debilitating diseases are not effective sufficiently. Therefore, novel treatment strategies are being explored to cure these diseases by addressing the causative mechanisms at the molecular level. Advanced therapies like gene therapy (gene editing and gene silencing) and stem cell therapies aim to cure diseases by gene editing, gene silencing and tissue regeneration, respectively. Gene editing results in the deletion of the aberrant gene or insertion of the corrected gene which can be executed using the CRISPR/Cas gene editing tool a promising treatment strategy being explored for many other prevalent diseases. Gene silencing using siRNA silences the gene by inhibiting protein translation, thereby silencing its expression. Stem cell therapy aims to regenerate damaged cells or tissues because of their ability to divide into any type of cell in the human body. Among these approaches, gene editing and gene silencing have currently been applied in vitro and to animal models, while stem cell therapy has reached the clinical trial stage for the treatment of NDs. The current status of these strategies suggests a promising outcome in their clinical translation.






Similar content being viewed by others
Data availability
Not applicable.
References
Collaborators GBDN (2019) Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 18(5):459–480
Kuriakose D, Xiao Z (2020) Pathophysiology and Treatment of Stroke: Present Status and Future Perspectives. Int J Mol Sci 21(20):7609
Broughton BR, Reutens DC, Sobey CG (2009) Apoptotic mechanisms after cerebral ischemia. Stroke 40(5):e331–e339
Flaherty ML et al (2005) Racial variations in location and risk of intracerebral hemorrhage. Stroke 36(5):934–937
de Leon BK, Zetterberg MJH (2006) Alzheimer’s disease. Lancet 29:368
Bondi MW, Edmonds EC, Salmon D (2017) Alzheimer’s disease: past, present, and future. J Int Neuropsychol Soc 23(9–10):818–831
Scheltens P, Blennow K, Breteler M, de Strooper B, Frisoni GB, Salloway S, van der Flier WM (2016) Alzheimer’s disease. Lancet 388(10043):505–517
Cummings JL, Tong G, Ballard C (2019) Treatment Combinations for Alzheimer’s Disease: Current and Future Pharmacotherapy Options. J Alzheimers Dis 67(3):779–794
Li HC, Luo KX, Wang JS, Wang QX (2020) Extrapyramidal side effect of donepezil hydrochloride in an elderly patient: a case report. Medicine 99(11)
Jankovic J, Tan EK (2020) Parkinson’s disease: Etiopathogenesis and treatment. J Neurol Neurosurg Psychiatry 91(8):795–808
Mhyre TR et al (2012) Parkinson’s disease. Subcell Biochem 65:389–455
Calabresi P et al (2008) Molecular mechanisms underlying levodopa-induced dyskinesia. Mov Disord: Off J Mov Disord Soc 23(S3):S570–S579
Eyford BA et al (2021) A nanomule peptide carrier delivers siRNA across the intact blood-brain barrier to attenuate ischemic stroke. Front Mol Biosci 8:133
Kim JS (2019) tPA helpers in the treatment of acute ischemic stroke: are they ready for clinical use? J Stroke 21(2):160
Tawil SE, Muir KW (2017) Thrombolysis and thrombectomy for acute ischaemic stroke. Clin Med (Lond) 17(2):161–165
O’Carroll CB, Aguilar MI (2015) Management of postthrombolysis hemorrhagic and orolingual angioedema complications. Neurohospitalist 5(3):133–141
Shah J, Liu S, Yu W (2022) Contemporary antiplatelet therapy for secondary stroke prevention: A narrative review of current literature and guidelines. Stroke Vasc Neurol svn-2021
Mohr J et al (2001) A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke. N Engl J Med 345(20):1444–1451
Martinsson L, Eksborg S (2004) Drugs for Stroke Recovery. Drugs Aging 21(2):67–79
Eyford BA, Singh CS, Abraham T, Munro L, Choi KB, Hill T, Hildebrandt R, Welch I, Vitalis TZ, Gabathuler R, Gordon JA (2021) A nanomule peptide carrier delivers siRNA across the intact blood-brain barrier to attenuate ischemic stroke. Front Mol Biosci, p 133
Fan W et al (2014) Caspase-3 modulates regenerative response after stroke. Stem Cells 32(2):473–486
Kim M et al (2019) Delivery of high mobility group box-1 siRNA using brain-targeting exosomes for ischemic stroke therapy. J Biomed Nanotechnol 15(12):2401–2412
Schneider LS (2022) A critical review of cholinesterase inhibitors as a treatment modality in Alzheimer's disease. Dialogues Clin Neurosci
Robinson DM, Keating GM (2006) Memantine. Drugs 66(11):1515–1534
Dunn B (2021) Stein, and Cavazzoni, Approval of aducanumab for Alzheimer disease—the FDA’s perspective. JAMA Intern Med 181(10):1276–1278
Chopade P, Chopade N, Zhao Z, Mitragotri S, Liao R, Chandran Suja V (2022) Alzheimer's and Parkinson's disease therapies in the clinic. Bioeng Transl Med e10367
Park H et al (2019) In vivo neuronal gene editing via CRISPR–Cas9 amphiphilic nanocomplexes alleviates deficits in mouse models of Alzheimer’s disease. Nat Neurosci 22(4):524–528
Wong E et al (2019) GSAP modulates γ-secretase specificity by inducing conformational change in PS1. Proc Natl Acad Sci 116(13):6385–6390
Nagata K et al (2018) Generation of App knock-in mice reveals deletion mutations protective against Alzheimer’s disease-like pathology. Nat Commun 9(1):1–7
Lee JK, Kim N-J (2017) Recent advances in the inhibition of p38 MAPK as a potential strategy for the treatment of Alzheimer’s disease. Molecules 22(8):1287
Fan X et al (2014) Stem-cell challenges in the treatment of Alzheimer’s disease: a long way from bench to bedside. Med Res Rev 34(5):957–978
Park D, Joo SS, Kim TK, Lee SH, Kang H, Lee HJ, Lim I, Matsuo A, Tooyama I, Kim YB, Kim SU (2012) Human neural stem cells overexpressing choline acetyltransferase restore cognitive function of kainic acid-induced learning and memory deficit animals. 365–371
Lee JK et al (2010) Intracerebral transplantation of bone marrow-derived mesenchymal stem cells reduces amyloid-beta deposition and rescues memory deficits in Alzheimer’s disease mice by modulation of immune responses. Stem cells 28(2):329–343
Bae J-S et al (2013) Bone marrow-derived mesenchymal stem cells contribute to the reduction of amyloid-β deposits and the improvement of synaptic transmission in a mouse model of pre-dementia Alzheimer’s disease. Curr Alzheimer Res 10(5):524–531
Takamatsu K et al (2014) Degradation of amyloid beta by human induced pluripotent stem cell-derived macrophages expressing Neprilysin-2. Stem Cell Res 13(3):442–453
Li X et al (2016) Human neural stem cell transplantation rescues cognitive defects in APP/PS1 model of Alzheimer’s disease by enhancing neuronal connectivity and metabolic activity. Front Aging Neurosci 8:282
Zhou Y et al (2020) Blood-brain barrier–penetrating siRNA nanomedicine for Alzheimer’s disease therapy. Sci Adv 6(41):eabc7031
Liu Y et al (2013) Investigation of the performance of PEG–PEI/ROCK-II-siRNA complexes for Alzheimer’s disease in vitro. Brain Res 1490:43–51
Kriebel-Gasparro A (2016) Parkinson’s disease: update on medication management. J Nurse Pract 12(3):e81–e89
Wilson SM et al (2020) Classics in chemical neuroscience: pramipexole. ACS Chem Neurosci 11(17):2506–2512
Frampton JE (2019) Rotigotine transdermal patch: a review in Parkinson’s disease. CNS Drugs 33(7):707–718
Cruz M (2017) Xadago (Safinamide): A Monoamine oxidase B inhibitor for the adjunct treatment of motor symptoms in Parkinson’s disease. Pharm Ther 42(10):622
Paik J, Keam SJ (2018) Amantadine extended-release (GOCOVRI™): a review in levodopa-induced dyskinesia in Parkinson’s disease. CNS Drugs 32(8):797–806
Aradi SD, Hauser RA (2020) Medical management and prevention of motor complications in Parkinson’s disease. Neurotherapeutics 17(4):1339–1365
Agbo F et al (2021) Pharmacokinetics and comparative bioavailability of apomorphine sublingual film and subcutaneous apomorphine formulations in patients with parkinson’s disease and “OFF” episodes: results of a randomized, three-way crossover, open-label study. Neurol Ther 10(2):693–709
Chen Y et al (2016) Chemical control of grafted human PSC-derived neurons in a mouse model of Parkinson’s disease. Cell Stem Cell 18(6):817–826
Lee J et al (2019) CRISPR/Cas9 edited sRAGE-MSCs protect neuronal death in Parkinson’s disease model. Int J Stem Cells 12(1):114124
Kantor B et al (2018) Downregulation of SNCA expression by targeted editing of DNA methylation: a potential strategy for precision therapy in PD. Mol Ther 26(11):2638–2649
Liao YJ, Liao CH, Chen LR, Yang JR (2022) Dopaminergic neurons derived from porcine induced pluripotent stem cell like cells function in the Lanyu pig model of Parkinson's disease. Anim Biotechnol 1–12
Zhang F, Wen Y, Guo X (2014) CRISPR/Cas9 for genome editing: progress, implications and challenges. Hum Mol Genet 23(R1):R40–R46
Savić N, Schwank G (2016) Advances in therapeutic CRISPR/Cas9 genome editing. Transl Res 168:15–21
Karimian A et al (2020) CRISPR/Cas9 novel therapeutic road for the treatment of neurodegenerative diseases. Life Sci 259:118165
György B et al (2018) CRISPR/Cas9 mediated disruption of the Swedish APP allele as a therapeutic approach for early-onset Alzheimer’s disease. Mol Ther-Nucleic Acids 11:429–440
Thangavel R et al (2018) Co-expression of glia maturation factor and apolipoprotein E4 in Alzheimer’s disease brain. J Alzheimers Dis 61(2):553–560
Schmid B et al (2019) Generation of a set of isogenic, gene-edited iPSC lines homozygous for all main APOE variants and an APOE knock-out line. Stem Cell Res 34:101349
Wadhwani AR et al (2019) Neuronal apolipoprotein E4 increases cell death and phosphorylated tau release in alzheimer disease. Ann Neurol 85(5):726–739
Guan L et al (2022) CRISPR-Cas9-Mediated Gene Therapy in Neurological Disorders. Mol Neurobiol 59(2):968–982
Bayarsaikhan E et al (2015) Microglial AGE-albumin is critical for neuronal death in Parkinson’s disease: a possible implication for theranostics. Int J Nanomed 10(Spec Iss):281
Li Z et al (2020) Stem cell-based therapies for ischemic stroke: a systematic review and meta-analysis of clinical trials. Stem Cell Res Ther 11(1):252–252
Levy ML et al (2019) Phase I/II study of safety and preliminary efficacy of intravenous allogeneic mesenchymal stem cells in chronic stroke. Stroke 50(10):2835–2841
Mazini L et al (2020) Hopes and limits of adipose-derived stem cells (ADSCs) and mesenchymal stem cells (MSCs) in wound healing. Int J Mol Sci 21(4):1306
Tsai S-T et al (2021) Stem cell therapy in stroke. Vessel Plus 5:9
Tobin MK et al (2020) Activated mesenchymal stem cells induce recovery following stroke via regulation of inflammation and oligodendrogenesis. J Am Heart Assoc 9(7):e013583
Horita Y et al (2006) Intravenous administration of glial cell line-derived neurotrophic factor gene-modified human mesenchymal stem cells protects against injury in a cerebral ischemia model in the adult rat. J Neurosci Res 84(7):1495–1504
Kalladka D et al (2016) Human neural stem cells in patients with chronic ischaemic stroke (PISCES): a phase 1, first-in-man study. Lancet 388(10046):787–796
Nito C et al (2018) Transplantation of human dental pulp stem cells ameliorates brain damage following acute cerebral ischemia. Biomed Pharmacother 108:1005–1014
Song M et al (2017) Human dental pulp stem cells are more effective than human bone marrow-derived mesenchymal stem cells in cerebral ischemic injury. Cell Transplant 26(6):1001–1016
Suda S et al (2020) Recent advances in cell-based therapies for ischemic stroke. Int J Mol Sci 21(18):6718
Zhang X et al (2020) Transplanted hair follicle stem cells migrate to the penumbra and express neural markers in a rat model of cerebral ischaemia/reperfusion. Stem Cell Res Ther 11(1):1–12
Han F et al (2020) Stem cell therapy for Alzheimer’s disease. Stem Cell-based Therapy for Neurodegenerative Diseases. Springer, pp 39–55
Garcia KO et al (2014) Therapeutic effects of the transplantation of VEGF overexpressing bone marrow mesenchymal stem cells in the hippocampus of murine model of Alzheimer’s disease. Front Aging Neurosci 6:30
Park I-H et al (2008) Disease-specific induced pluripotent stem cells. Cell 134(5):877–886
Cha M-Y et al (2017) Protein-induced pluripotent stem cells ameliorate cognitive dysfunction and reduce Aβ deposition in a mouse model of Alzheimer’s disease. Stem Cells Transl Med 6(1):293–305
Ager RR et al (2015) Human neural stem cells improve cognition and promote synaptic growth in two complementary transgenic models of Alzheimer’s disease and neuronal loss. Hippocampus 25(7):813–826
Tang J et al (2008) Embryonic stem cell-derived neural precursor cells improve memory dysfunction in Aβ (1–40) injured rats. Neurosci Res 62(2):86–96
Yue W et al (2015) ESC-derived basal forebrain cholinergic neurons ameliorate the cognitive symptoms associated with Alzheimer’s disease in mouse models. Stem Cell Reports 5(5):776–790
Dana H et al (2017) Molecular mechanisms and biological functions of siRNA. Int J Biomed Sci: IJBS 13(2):48
Lopez-Barbosa N et al (2020) Multifunctional magnetite nanoparticles to enable delivery of siRNA for the potential treatment of Alzheimer’s. Drug Deliv 27(1):864–875
Wang Z et al (2020) SYNERGIC treatment of Alzheimer’s disease with brain targeted nanoparticles incorporating NGR-Sirna and brain derived neurotrophic factor. Smart Mater Med 1:125–130
Dhall A, Self W (2018) Cerium Oxide Nanoparticles: A Brief Review of Their Synthesis Methods and Biomedical Applications. Antioxidants (Basel, Switzerland) 7(8):97
Helmschrodt C et al (2017) Polyethylenimine nanoparticle-mediated siRNA delivery to reduce α-Synuclein expression in a model of Parkinson’s disease. Mol Ther-Nucleic Acids 9:57–68
Li R et al (2021) Multifunctional Nanoprobe for the Delivery of Therapeutic siRNA and Real-Time Molecular Imaging of Parkinson’s Disease Biomarkers. ACS Appl Mater Interfaces 13(10):11609–11620
Cooper JM et al (2014) Systemic exosomal siRNA delivery reduced alpha-synuclein aggregates in brains of transgenic mice. Mov Disord 29(12):1476–1485
Pinho AG et al (2020) Cell secretome: basic insights and therapeutic opportunities for CNS disorders. Pharmaceuticals 13(2):31
Drago D et al (2013) The stem cell secretome and its role in brain repair. Biochimie 95(12):2271–2285
Hathout Y (2007) Approaches to the study of the cell secretome. Expert Rev Proteomics 4(2):239–248
Mukherjee P, Mani S (2013) Methodologies to decipher the cell secretome. Biochim Biophys Acta BBA Protein Proteomics 1834(11):2226–2232
Mendes-Pinheiro B et al (2018) Secretome of undifferentiated neural progenitor cells induces histological and motor improvements in a rat model of Parkinson’s disease. Stem Cells Transl Med 7(11):829–838
Doeppner TR et al (2015) Extracellular vesicles improve post-stroke neuroregeneration and prevent postischemic immunosuppression. Stem Cells Transl Med 4(10):1131–1143
Huang W et al (2015) Paracrine factors secreted by MSCs promote astrocyte survival associated with GFAP downregulation after ischemic stroke via p38 MAPK and JNK. J Cell Physiol 230(10):2461–2475
Zhang Q et al (2020) Neural stem cell secretome and its role in the treatment of neurodegenerative disorders. J Integr Neurosci 19(1):179–185
Li J et al (2017) Effect of VEGF on inflammatory regulation, neural survival, and functional improvement in rats following a complete spinal cord transection. Front Cell Neurosci 11:381
Aly AE-E et al (2019) Intranasal delivery of pGDNF DNA nanoparticles provides neuroprotection in the rat 6-hydroxydopamine model of Parkinson’s disease. Mol Neurobiol 56(1):688–701
Ishizaka S et al (2013) Intra-arterial cell transplantation provides timing-dependent cell distribution and functional recovery after stroke. Stroke 44(3):720–726
Schäbitz W-R et al (2000) Intravenous brain-derived neurotrophic factor reduces infarct size and counterregulates Bax and Bcl-2 expression after temporary focal cerebral ischemia. Stroke 31(9):2212–2217
Schäbitz W-R et al (2007) Intravenous brain-derived neurotrophic factor enhances poststroke sensorimotor recovery and stimulates neurogenesis. Stroke 38(7):2165–2172
Miki Y et al (2007) Vascular endothelial growth factor gene-transferred bone marrow stromal cells engineered with a herpes simplex virus type 1 vector can improve neurological deficits and reduce infarction volume in rat brain ischemia. Neurosurgery 61(3):586–595
Zhou L et al (2017) Enhanced neuroprotective efficacy of bone marrow mesenchymal stem cells co-overexpressing BDNF and VEGF in a rat model of cardiac arrest-induced global cerebral ischemia. Cell Death Dis 8(5):e2774–e2774
Oh SH et al (2017) The cleavage effect of mesenchymal stem cell and its derived matrix metalloproteinase-2 on extracellular α-synuclein aggregates in parkinsonian models. Stem Cells Transl Med 6(3):949–961
Nutt J et al (2003) Randomized, double-blind trial of glial cell line-derived neurotrophic factor (GDNF) in PD. Neurology 60(1):69–73
Lang AE et al (2006) Randomized controlled trial of intraputamenal glial cell line–derived neurotrophic factor infusion in Parkinson disease. Ann Neurol 59(3):459–466
Allen SJ et al (2013) GDNF, NGF and BDNF as therapeutic options for neurodegeneration. Pharmacol Ther 138(2):155–175
Ahmed NEMB, Murakami M, Hirose Y, Nakashima M (2016) Therapeutic potential of dental pulp stem cell secretome for Alzheimer’s disease treatment: an in vitro study. Stem Cells Int 8102478. https://doi.org/10.1155/2016/8102478
Santamaria G et al (2021) Intranasal delivery of mesenchymal stem cell secretome repairs the brain of Alzheimer’s mice. Cell Death Differ 28(1):203–218
Hijroudi F, Rahbarghazi R, Sadigh-Eteghad S, Bahlakeh G, Hassanpour M, Shimia M, Karimipour M (2022) Neural stem cells secretome increased neurogenesis and behavioral performance and the activation of Wnt/β-Catenin signaling pathway in mouse model of Alzheimer’s disease. Neuromolecular Med 1–13
Acknowledgements
Financial assistance from DST-FIST, Indian Council of Medical Research (ICMR), New Delhi, and Council for Scientific and Industrial Research (CSIR), India, is highly acknowledged.
Funding
Financial support from ICMR, New Delhi (RFC No. (p-64) NCD/Adhoc/139/2020–21), DST-FIST (SR/FST/LS-I/2017/49) and SRF awarded to Mr. Abhilash Ludhiadch (Award No-09/ 1051(0029)/2 019-EMR-1) from the Council for Scientific and Industrial Research (CSIR) India is acknowledged with thanks.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethics approval
Not applicable.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Katta, M., Mathew, B.A., Chaturvedi, P. et al. Advanced molecular therapies for neurological diseases: focus on stroke, alzheimer's disease, and parkinson's disease. Neurol Sci 44, 19–36 (2023). https://doi.org/10.1007/s10072-022-06356-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-06356-6