Abstract
Background
Retinal biomarkers in neurodegenerative disorders have attracted much attention in recent years. Recent studies have reported visual dysfunction in Huntington’s disease (HD). However, little is known about retinal structural changes in HD.
Methods
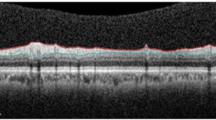
A total of 50 subjects, including 25 motor-manifest HD patients and 25 gender- and age-matched controls, were enrolled. Unified Huntington’s Disease Rating Score-Motor part was assessed in HD patients. Spectral-domain Optical Coherence Tomography (SD-OCT) was used to evaluate the macular thickness and peripapillary retinal nerve fiber layer (pRNFL). Superficial and deep capillary plexus densities were measured using OCT angiography (OCTA). To account for inter-eye correlation, generalized estimating equation (GEE) model was used.
Results
HD patients had a significant reduction in macular thickness in both inner and outer superior sectors and the inferior outer sector. Inferior pRNFLs were significantly decreased in thickness. There was no significant difference in retinal capillary plexus density between the two groups. Age and disease duration were negatively correlated with macular thickness in HD patients. However, the severity of motor involvement was not correlated with SD-OCT or OCTA parameters.
Conclusions
We observed attenuated pRNFL and macular retinal thickness in patients with HD, independent of macular capillary plexus parameters. It can support the hypothesis that the retina may be a potential biomarker for monitoring the neurodegenerative process in HD.


Similar content being viewed by others
References
Roos RA (2010) Huntington’s disease: a clinical review. Orphanet J Rare Dis 5(1):1–8. https://doi.org/10.1186/1750-1172-5-40
Andrade C, Beato J, Monteiro A, Costa A, Penas S, Guimarães J, Reis FF, Garrett C (2016) Spectral-domain optical coherence tomography as a potential biomarker in Huntington’s disease. Mov Disord 31(3):377–383. https://doi.org/10.1002/mds.26486
Di Maio LG, Montorio D, Peluso S, Dolce P, Salvatore E, De Michele G, Cennamo G (2021) Optical coherence tomography angiography findings in Huntington’s disease. Neurol Sci 42(3):995–1001. https://doi.org/10.1007/s10072-020-04611-2
Kersten HM, Danesh-Meyer HV, Kilfoyle DH, Roxburgh RH (2015) Optical coherence tomography findings in Huntington’s disease: a potential biomarker of disease progression. J Neurol 262(11):2457–2465. https://doi.org/10.1007/s00415-015-7869-2
Gatto E, Parisi V, Persi G, Fernandez Rey E, Cesarini M, Luis Etcheverry J, Rivera P, Squitieri F (2018) Optical coherence tomography (OCT) study in Argentinean Huntington’s disease patients. Int J Neurosci 128(12):1157–1162. https://doi.org/10.1080/00207454.2018.1489807
Mason SL, Barker RA (2016) Novel targets for Huntington’s disease: future prospects. Degener Neurol Neuromuscul Dis 6:25. https://doi.org/10.2147/DNND.S83808
Ha AD, Fung VS (2012) Huntington’s disease. Curr Opin Neurol 25(4):491–498. https://doi.org/10.1097/WCO.0b013e3283550c97
Crair MC, Mason CA (2016) Reconnecting eye to brain. J Neurosci 36(42):10707–10722. https://doi.org/10.1523/JNEUROSCI.1711-16.2016
Trost A, Lange S, Schroedl F, Bruckner D, Motloch KA, Bogner B, Kaser-Eichberger A, Strohmaier C, Runge C, Aigner L (2016) Brain and retinal pericytes: origin, function and role. Front Cell Neurosci 10:20. https://doi.org/10.3389/fncel.2016.00020
Doustar J, Torbati T, Black KL, Koronyo Y, Koronyo-Hamaoui M (2017) Optical coherence tomography in Alzheimer’s disease and other neurodegenerative diseases. Front Neurol 8:701. https://doi.org/10.3389/fneur.2017.00701
Moinuddin O, Khandwala NS, Young KZ, Sathrasala SK, Barmada SJ, Albin RL, Besirli CG (2021) Role of optical coherence tomography in identifying retinal biomarkers in frontotemporal dementia: a review. Neurol Clin Pract 11(4):e516–e523. https://doi.org/10.1212/CPJ.0000000000001041
Sengupta P, Dutta K, Ghosh S, Mukherjee A, Pal S, Basu D (2018) Optical coherence tomography findings in patients of Parkinson’s disease an Indian perspective. Ann Indian Acad Neurol 21(2):150. https://doi.org/10.4103/aian.AIAN_152_18
Abd Hamid MR, Hitam W-HW, Abd Halim S (2021) Retinal nerve fiber layer and macular thickness in Parkinson’s disease patients. Cureus 13(7):e16224. https://doi.org/10.7759/cureus.16224
Schneider M, Müller H-P, Lauda F, Tumani H, Ludolph AC, Kassubek J, Pinkhardt EH, Retinal single-layer analysis in Parkinsonian syndromes (2014) an optical coherence tomography study. J Neural Transm 121(1):41–47. https://doi.org/10.1007/s00702-013-1072-3
Chan VT, Sun Z, Tang S, Chen LJ, Wong A, Tham CC, Wong TY, Chen C, Ikram MK, Whitson HE (2019) Spectral-domain OCT measurements in Alzheimer’s disease: a systematic review and meta-analysis. Ophthalmology 126(4):497–510. https://doi.org/10.1016/j.ophtha.2018.08.009
Dhalla A, Pallikadavath S, Hutchinson CV (2019) Visual dysfunction in Huntington’s disease: a systematic review. J Huntingtons Dis 8(2):233–242. https://doi.org/10.3233/JHD-180340
Hui J, Zhao Y, Yu S, Liu J, Chiu K, Wang Y (2021) Detection of retinal changes with optical coherence tomography angiography in mild cognitive impairment and Alzheimer’s disease patients: a meta-analysis. PLoS ONE 16(8):e0255362. https://doi.org/10.1371/journal.pone.0255362
Tsokolas G, Tsaousis KT, Diakonis VF, Matsou A, Tyradellis S (2020) Optical coherence tomography angiography in neurodegenerative diseases: a review. Eye Brain 12:73. https://doi.org/10.2147/EB.S193026
Siesling S, van Vugt JP, Zwinderman KA, Kieburtz K, Roos RA (1998) Unified Huntington’s disease rating scale: a follow up. Mov Disord 13(6):915–919. https://doi.org/10.1002/mds.870130609
Ghasemi Falavarjani K, Mirshahi R, Ghasemizadeh S, Sardarinia M (2020) Stepwise segmentation error correction in optical coherence tomography angiography images of patients with diabetic macular edema. Ther Adv Ophthalmol 27:12. https://doi.org/10.1177/2515841420947931
Zou J, Liu K, Li F, Xu Y, Shen L, Xu H (2020) Combination of optical coherence tomography (OCT) and OCT angiography increases diagnostic efficacy of Parkinson’s disease. Quant Imaging Med Surg 10(10):1930. https://doi.org/10.21037/qims-20-460
Sevim DG, Unlu M, Gultekin M, Karaca C (2019) Retinal single-layer analysis with optical coherence tomography shows inner retinal layer thinning in Huntington’s disease as a potential biomarker. Int Ophthalmol 39(3):611–621. https://doi.org/10.1007/s10792-018-0857-7
Parisi V, Restuccia R, Fattapposta F, Mina C, Bucci MG, Pierelli F (2001) Morphological and functional retinal impairment in Alzheimer’s disease patients. Clin Neurophysiol 112(10):1860–1867. https://doi.org/10.1016/S1388-2457(01)00620-4
Lu Y, Li Z, Zhang X, Ming B, Jia J, Wang R, Ma D (2010) Retinal nerve fiber layer structure abnormalities in early Alzheimer’s disease: evidence in optical coherence tomography. Neurosci Lett 480(1):69–72. https://doi.org/10.1016/j.neulet.2010.06.006
Kesler A, Vakhapova V, Korczyn AD, Naftaliev E, Neudorfer M (2011) Retinal thickness in patients with mild cognitive impairment and Alzheimer’s disease. Clin Neurol Neurosurg 113(7):523–526. https://doi.org/10.1016/j.clineuro.2011.02.014
Chi Y, Wang Y-h, Yang L (2010) The investigation of retinal nerve fiber loss in Alzheimer’s disease. [Zhonghua yan ke za zhi] Chinese J Ophthalmol 46(2):134–139
Kromer R, Serbecic N, Hausner L, Aboul-Enein F, Froelich L, Beutelspacher S (2014) Detection of retinal nerve fiber layer defects in Alzheimer’s disease using SD-OCT. Front Psych 5:22. https://doi.org/10.3389/fpsyt.2014.00022
Zabel P, Kałużny JJ, Wiłkość-Dębczyńska M, Gębska-Tołoczko M, Suwała K, Kucharski R, Araszkiewicz A (2019) Peripapillary retinal nerve fiber layer thickness in patients with Alzheimer’s disease: a comparison of eyes of patients with Alzheimer’s disease, primary open-angle glaucoma, and preperimetric glaucoma and healthy controls. Med Sci Monit 25:1001. https://doi.org/10.12659/MSM.914889
Yu J-G, Feng Y-F, Xiang Y, Huang J-H, Savini G, Parisi V, Yang W-J, Fu X-A (2014) Retinal nerve fiber layer thickness changes in Parkinson disease: a meta-analysis. PLoS ONE 9(1):e85718. https://doi.org/10.1371/journal.pone.0085718
Rohani M, Langroodi AS, Ghourchian S, Falavarjani KG, SoUdi R, Shahidi G (2013) Retinal nerve changes in patients with tremor dominant and akinetic rigid Parkinson’s disease. Neurol Sci 34(5):689–693. https://doi.org/10.1007/s10072-012-1125-7
Birkeldh U, Manouchehrinia A, Hietala MA, Hillert J, Olsson T, Piehl F, Kockum IS, Brundin L, Zahavi O, Wahlberg-Ramsay M (2017) The temporal retinal nerve fiber layer thickness is the most important optical coherence tomography estimate in multiple sclerosis. Front Neurol 8:675. https://doi.org/10.3389/fneur.2017.00675
Gómez-Esteban JC, Lezcano E, Zarranz JJ, Velasco F, Garamendi I, Pérez T, Tijero B (2007) Monozygotic twins suffering from Huntington’s disease show different cognitive and behavioural symptoms. Eur Neurol 57(1):26–30. https://doi.org/10.1159/000097006
Georgiou N, Bradshaw JL, Chiu E, Tudor A, O’Gorman L, Phillips JG (1999) Differential clinical and motor control function in a pair of monozygotic twins with Huntington’s disease. Mov Disord 14(2):320–325. https://doi.org/10.1002/1531-8257(199903)14:2%3c320::AID-MDS1018%3e3.0.CO;2-Z
Ferrari L, Huang S-C, Magnani G, Ambrosi A, Comi G, Leocani L (2017) Optical coherence tomography reveals retinal neuroaxonal thinning in frontotemporal dementia as in Alzheimer’s disease. J Alzheimers Dis 56(3):1101–1107. https://doi.org/10.3233/JAD-160886
Chan ST, Mercaldo ND, Kwong KK, Hersch SM, Rosas HD (2021) Impaired cerebrovascular reactivity in Huntington’s disease. Front Physiol 12:663898. https://doi.org/10.3389/fphys.2021.663898
Bodis-Wollner I (2013) Foveal vision is impaired in Parkinson’s disease. Parkinsonism Relat Disord 19(1):1–14. https://doi.org/10.1016/j.parkreldis.2012.07.012
Polo V, Rodrigo MJ, Garcia-Martin E, Otin S, Larrosa JM, Fuertes MI, Bambo MP, Pablo LE, Satue M (2017) Visual dysfunction and its correlation with retinal changes in patients with Alzheimer’s disease. Eye (Lond) 31(7):1034–1041. https://doi.org/10.1038/eye.2017.23
Nanetti L, Contarino VE, Castaldo A, Sarro L, Bachoud-Levi A-C, Giavazzi M, Frittoli S, Ciammola A, Rizzo E, Gellera C (2018) Cortical thickness, stance control, and arithmetic skill: an exploratory study in premanifest Huntington disease. Parkinsonism Relat Disord 51:17–23. https://doi.org/10.1016/j.parkreldis.2018.02.033
Odish O, Reijntjes R, van den Bogaard S, Roos R, Leemans A (2018) Progressive microstructural changes of the occipital cortex in Huntington’s disease. Brain Imaging Behav 12(6):1786–1794. https://doi.org/10.1007/s11682-018-9849-5
Johnson EB, Rees EM, Labuschagne I, Durr A, Leavitt BR, Roos RA, Reilmann R, Johnson H, Hobbs NZ, Langbehn DR (2015) The impact of occipital lobe cortical thickness on cognitive task performance: an investigation in Huntington’s disease. Neuropsychologia 79:138–146. https://doi.org/10.1016/j.neuropsychologia.2015.10.033
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All the procedures contributing to this work were in accordance with the ethical standards of the relevant national and institutional review board guidelines on human experimentation Iran University of Medical Sciences IR.IUMS.FMD.REC.1399.350 and compliant with the Helsinki Declaration.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Amini, E., Moghaddasi, M., Habibi, S.A.H. et al. Huntington’s disease and neurovascular structure of retina. Neurol Sci 43, 5933–5941 (2022). https://doi.org/10.1007/s10072-022-06232-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-06232-3