Abstract
Background
Identifying late epileptic seizures (LS) following cerebral venous thrombosis (CVT) can be useful for prognosis and management. We systematically reviewed the literature to identify risk factors for LS due to CVT.
Methods
We systematically searched PubMed, Scholar, and Scopus databases (May 2021) to identify studies reporting data on prevalence and risk factors for CVT-LS. The methodological quality was assessed with the Ottawa-Newcastle Scale. The risk of developing CVT-LS was summarized in meta-analyses and expressed as odds ratio (OR) and corresponding 95% confidence intervals (CIs) using random-effects models.
Results
Out of the 332 records retrieved, four studies were eventually included with a total of 1309 patients with CVT and 142 (11%) with CVT-LS. The most relevant predictors of CVT-LS were symptomatic seizures (OR 5.66, 95% CI 3.83–8.35), stupor/coma (OR 6.81, 95% CI 1.18–39.20), focal neurologic signs (OR 6.81, 95% CI 1.18–39.2), hemorrhagic component (OR 3.52, 95% CI 2.45–5.06), and superior sagittal sinus involvement (OR 1.52, 95% CI 1.04–2.21).
Conclusion
There are several risk factors for CVT-LS that should be considered in clinical practice. Further high-quality studies are warranted to develop predictive models for individualized risk stratification and prediction of CVT-LS.
Similar content being viewed by others
Introduction
Cerebral venous thrombosis (CVT) is a cerebrovascular disease most often affecting children and young adults (particularly women), with an estimated annual incidence of 3 to 10 cases per million people (estimated incidence 1.32/100,000/year in Western Europe). About 75% of affected adult patients are women [1]. The prognosis of CVT varies according to the extension of sinus involvement and of parenchymal damage to comorbidities and the underlying cause (i.e., genetic thrombophilic diseases, antiphospholipid syndrome, myeloproliferative disorders and malignancies, infections, use of oral contraceptives, pregnancy, or puerperium). Despite significant variability in the clinical presentation and course, nowadays, over 80% of patients have a good neurological outcome [1].
Common symptoms of CVT include headache, which is present in over 90% of adult patients, and impairment of consciousness, ranging from drowsiness to coma [1, 2]. Parenchymal brain lesions and focal neurological signs develop in half of the cases. Seizures, both focal and focal to bilateral tonic–clonic, occur in about 40% of patients, a much higher percentage as compared to those occurring after an ischemic stroke. A proportion of these patients present with status epilepticus, a potentially life-threatening condition. Acute symptomatic seizures, which by definition occur within 7 days from CVT (also termed early seizures) [3], can be found in approximately 35–50% of all patients, with a higher incidence (76%) in peripartum CVT [4, 5]. Late seizures (CVT-LS) occur more than 7 days after CVT and should be regarded as unprovoked seizures; they may affect the quality of life, requiring long-term treatment with anti-seizure medications (ASM) [1, 2].
According to the International League Against Epilepsy (ILAE), it is possible to diagnose epilepsy after a single unprovoked seizure in specific conditions that carry a risk of seizure recurrence greater than 60% in the following 10 years [6]. However, little is known about the probability of recurrence after a first CVT-LS.
Risk factors for acute symptomatic seizures in the course of CVT include focal neurologic deficits, supratentorial parenchymal lesions, intracerebral hemorrhage, focal edema/infarction, superior sagittal sinus thrombosis, cortical venous thrombosis, and pregnancy or puerperium [7,8,9]. Conversely, risk factors for CVT-LS are still unclear. Being able to identify predictors of late-onset seizures and CVT-LS could help neurologists to identify high-risk patients and to plan long-term treatment. For these reasons, we performed a systematic review and meta-analysis of published studies to identify the risk factors for CVT-LS.
Methods
Search strategy, study selection, and data extraction
Results of this review were reported according to the PRISMA guidelines (the checklist is reported in the Supplementary Material).
We conducted a systematic search of the literature in the following databases, from inception to May 2021: MEDLINE (accessed through PubMed interface), Google Scholar, and Scopus. The search strategies used are reported in the Supplementary Material. Studies were included if they met the following criteria: explicit differentiation between early and late post-CVT seizures; reporting data on sex, age, occurrence of acute symptomatic/early seizures, prophylaxis with ASM, impairment of consciousness, focal neurological signs, hemorrhagic component, involvement of specific venous sinuses or cortical veins, or supratentorial localization. Articles that did not meet the above criteria were excluded. The studies were initially selected for inclusion by two authors (SG and EF). From the included papers, the same authors extracted data on study design, total number of patients, age and gender, cut-off for defining LS, duration of follow-up, seizure prevalence, and details on the variables of interest. Study selection and data extraction were performed independently; discrepancies were resolved by mutual discussion.
Assessment of methodological quality
The risk of bias for all included studies was assessed using the Newcastle–Ottawa scale [10].
Statistical analysis
For each variable, we carried out a quantitative synthesis (meta-analysis) to summarize the risk of developing CVT-LS across different studies. Results were synthesized using a random-effects model to take into account the differences in clinical characteristics and design across studies. The pooled risk of developing CVT-LS was expressed using odds ratios (ORs) with 95% confidence intervals (CI). Values of p < 0.05 were considered statistically significant. The statistical heterogeneity between the studies was assessed using the I2 index and calculating the Cochran’s Q with its p-value. Meta-analyses were performed with Comprehensive Meta-Analysis, version 3.3.070.
Results
The search strategy yielded 332 results (270 through PubMed, 34 through Scopus, and 28 through Google Scholar); 315 studies were excluded either because of their irrelevance to the topic or because they were duplicated and 13 because they did not meet the inclusion criteria (Fig. 1). The meta-analyses included results from 4 studies, published between 2003 and 2020 [11,12,13,14]. Data of the included studies are summarized in Table 1. In the Newcastle–Ottawa scale evaluation, the studies scored from 4 to 6 points, indicating a medium risk of bias. Details about ratings of the single studies are reported in the Supplementary Materials.
The four studies included 1309 patients with CVT, of whom 142 were diagnosed with CVT-LS (11%). Three studies had a retrospective design and one a mixed prospective/retrospective design. As expected, all studies had a female preponderance. The occurrence of epileptic seizures was ascertained in different ways, including a review of medical records, outpatient visits, and telephone interviews.
Four variables (age, status epilepticus, cortical vein thrombosis, and supratentorial localization) were excluded from the meta-analysis due to a lack of consistent data.
Acute symptomatic seizures following cerebral venous thrombosis
Four studies were included in this analysis [11,12,13,14], with no statistical heterogeneity across studies (I2 = 0, Q value = 2.7, and p = 0.44). The occurrence of acute symptomatic seizures was associated with a fivefold increased risk of developing CVT-LS (OR 5.66, 95% IC 3.83–8.35, p < 0.001) (Fig. 2).
Prophylaxis with antiseizure medications
In this analysis, two studies were included [12, 13], with no significant statistical heterogeneity (I2 = 0, Q value = 0.32, and p = 0.58). The prophylactic use of ASM was associated with a greater probability of having CVT-LS, although with a large confidence interval, due to the small number of events and included patients (OR 10.5, 95% IC 2.28–48.03, p = 0.003) (Fig. 3).
Impairment of consciousness (stupor/coma)
Three studies were included in this analysis [11, 13, 14], with evidence of statistical heterogeneity (I2 = 69%, Q value = 6.46, and p = 0.04). Impairment of consciousness was associated with a greater probability of having CVT-LS: patients with drowsiness or coma had a sevenfold increased risk (OR 6.81, 95% IC 1.18–39.2, p = 0.032) (Fig. 4). However, the estimate was imprecise, as shown by the large confidence interval, due to the small number of events and included patients.
Focal neurological signs
In this analysis, three studies were included [11, 13, 14], with evidence of statistical heterogeneity (I2 = 69%, Q value = 6.46, and p = 0.04). The occurrence of focal neurological signs (hemiparesis, hemianopia, aphasia, or a combination of signs) was associated with a sixfold increased risk of developing CVT-LS (OR 6.81, 95% IC 1.18–39.2, p = 0.032) (Fig. 5). Again, the confidence interval of the estimate was large, due to the small number of events and included patients.
Hemorrhagic component
Three studies were included in this analysis [12,13,14], with no evidence of statistical heterogeneity across studies (I2 = 0, Q value = 0.30, and p = 0.86). A hemorrhagic component was associated with a greater probability to have CVT-LS (OR 3.52, 95% CI 2.45–5.06, p < 0.001) (Fig. 6).
Sex
Four studies were included [11,12,13,14], with I2 = 0, Q = 0.85, and p = 0.84. Sex was not a determinant of LS in patients with CVT (OR 0.81, 95% CI 0.56–1.19, p = 0.283) (Figure S1).
Involvement of specific sinuses
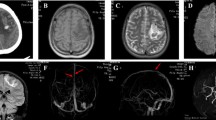
Two studies [13, 14] evaluated the involvement of specific venous sinuses, although with a moderate statistical heterogeneity across studies (I2 = 43%, Q value = 1.77, and p = 0.18). The involvement of lateral or sigmoid sinus (OR 1.40, 95% CI 0.27–7.21, p = 0.69) and straight sinus (OR 1.70, 95% CI 0.37–7.88, p = 0.495) was not associated with CVT-LS (Figures S2 and S3). Conversely, thrombosis of the superior sagittal sinus (Fig. 7) was associated with a moderate increased risk of CVT-LS (OR 1.52, 95% CI 1.04–2.21, p = 0.029).
Variables not evaluated in the meta-analysis
We were not able to analyze the following variables: age, cortical vein thrombosis, and supratentorial localization. Age was reported heterogeneously across studies: in some articles, it was analyzed as a continuous variable, whereas other studies adopted arbitrary cut-offs. The presence of cortical vein thrombosis [14] and supratentorial localization [13] were analyzed in a single study each. In the largest included study on predictors of CVT-LS [13], the presence of a supratentorial localization was associated with a greater risk of developing late seizures, but this variable was not an independent predictor in multivariate analysis. In another study [14], the presence of cortical vein thrombosis was a predictor of CVT-LS. The same study identified symptomatic acute status epilepticus as a further risk factor for CVT-LS, with a hazard ratio of 7.0 [14].
Discussion
In this systematic review, we identified the following risk factors for CVT-LS: occurrence of acute symptomatic seizures, hemorrhagic lesions; prophylaxis with ASM, focal neurological signs, alterations of consciousness, and involvement of the superior sagittal sinus. These risk factors should be considered in clinical practice to identify patients who are at high risk of developing CVT-LS.
Across the included studies, 11% of patients with CVT developed one or more LS over an average period of 24 months. Although the practical definition of epilepsy by ILAE [6] does not explicitly list CVT among the conditions that allow formulating a diagnosis of epilepsy after a single LS, the largest study included in the present review found that 70% of patients with a first CVT-LS experienced a seizure recurrence over a median follow-up of 2.6 years. This risk is much higher than the cut-off proposed by ILAE; accordingly, the occurrence of a single CVT-LS may therefore be considered as structural epilepsy.
Patients with LS had more often focal neurological deficits, coma, and acute symptomatic seizures on initial admission for CVT. On baseline imaging, intracerebral hemorrhage, sulcal subarachnoid hemorrhage, and subdural hematoma were also more common. Furthermore, these subjects had more frequently a thrombosis of the superior sagittal sinus and cortical veins. Acute symptomatic (early) seizures were associated with a fivefold increased risk of CVT-LS; they should be considered a major risk factor for LS, a finding consistent with the literature on the occurrence of post-stroke epilepsy [15, 16]. Thus, although acute symptomatic seizures following a brain injury are not associated with a very high risk of relapse by themselves [17], it is appropriate to consider patients with early seizures as being at high risk of developing CVT-LS.
The treatment with ASMs in the acute phase was found more frequently in patients who later developed CVT-LS. This may reflect the attitude to prescribe ASMs after acute symptomatic seizures and the perceived high risk for recurrence in these patients. The high incidence of LS despite drug treatment confirms that ASMs do not have any anti-epileptogenic effect, as shown in animal models [18] and emphasized by expert opinions [19]. At the same time, on the basis of the available literature data, prophylactic therapy with ASMs in patients with CVT who have never presented seizures is not recommended [20]. The association between ASMs and increased risk of CVT-LS should be read with caution, as it could reflect variability in treatment strategies across studies and individual therapeutic considerations, often not explicitly reported difficult to judge. From a practical point of view, a patient with CVT who is deemed at high risk for CVT-LS should be followed up closely, but the caring physician should be reassuring on the relatively low risk of seizures and on the fact that a prophylaxis treatment is not necessary.
The presence of bleeding on admission imaging was a further risk factor for CVT-LS. In animal experiments, it has been shown that seizures can be induced by the extravasation of serum-derived components in the context of an altered blood–brain barrier [21, 22]. The association between hemorrhagic lesions and seizures is probably due to the “irritative” effect of the exudation of hemosiderin and its metabolites on the cerebral cortex [21, 22]. Hemorrhage (both primary intraparenchymal hemorrhage or, as in CVT, hemorrhagic transformation of ischemic infarction) is a known risk factor for post-stroke epilepsy, as confirmed by clinical studies [23].
Patients with CVT presenting with signs of encephalopathy, such as coma or impaired consciousness or with persistent focal neurologic deficits secondary to focal structural damage (e.g., aphasia, hemianopia, and hemiparesis), were more likely to experience CVT-LS. This finding may indicate that patients with diffuse structural brain lesions or injuries involving the cerebral cortex are at increased risk of developing LS. Similar results were observed also in a large study [24]. Moreover, the only predictor of late seizures among different anatomic locations of CVT was the superior sagittal sinus, which drains the blood from the supratentorial parenchyma, including most cortical regions. The presence of cortical venous infarcts, or supratentorial lesions per se, could not be analyzed in a metanalysis. However, data from a large study show that supratentorial involvement may be related to the occurrence of late seizures [14], a finding in line with other studies on post-stroke epilepsy. The presence of cortical lesions is indeed associated with a greater risk of epilepsy in patients with stroke of any nature [23, 25].
In our meta-analysis, age could not be evaluated as a possible predictor of LS, but both in the largest study included in the meta-analysis [14] and in other studies [7, 25], it does not seem to have a predictive role. Furthermore, although CVT occurs in great preponderance in the female sex, this meta-analysis did not identify gender as a predictor of LS.
Since the present study was planned before the outbreak of the Covid-19 pandemic, we did not analyze the presence of Sars-Cov-2 infection or a previous Covid-19 vaccination as a possible predictor of CVT-LS. Data from the existing literature are not conclusive on the incidence of early or late seizures in patients with CVT caused by Sars-Cov-2 infection [26] or by vaccination in the context of immune thrombotic thrombocytopenia [27].
This study has some limitations. Only four studies were eligible and included, and one of them contributed with the majority of data. The clinical and methodological heterogeneity across studies was partly mitigated by the adoption of a random-effects model. It was impossible to assess some variables due to the heterogeneity and scarcity of data. Lastly, the overall quality of studies was suboptimal, emphasizing the need for future high-quality research in this field.
The negative effects of LS on the independence and quality of life justify the planning of large and prospective studies with the aim of better characterizing the risk factors for the development of epilepsy due to CVT, its prevention, and the most appropriate drug treatment. Identifying risk factors for epilepsy following CVT would be important for individualized risk stratification and tailored therapeutic strategies to prevent seizure recurrence.
References
Silvis SM, de Sousa DA, Ferro JM, Coutinho JM (2017) Cerebral venous thrombosis. Nat Rev Neurol 13:555–565. https://doi.org/10.1038/nrneurol.2017.104
De Bruijn SF, Stam J, Kappelle LJ (1996) Thunderclap headache as first symptom of cerebral venous sinus thrombosis. Lancet 348:1623–1625. https://doi.org/10.1016/s0140-6736(96)07294-7
Beghi E, Carpio A, Forsgren L et al (2010) Recommendation for a definition of acute symptomatic seizure. Epilepsia 51:671–675. https://doi.org/10.1111/j.1528-1167.2009.02285.x
Ameri A, Bousser MG (1992) Cerebral venous thrombosis. Neurol Clin 10:87–111
Ferro JM, Correia M, Pontes C et al (2001) Cerebral venous thrombosis Portuguese Collaborative Study Group (Venoport). Cerebral vein and dural sinus thrombosis in Portugal: 1980–1998. Cerebrovascular Disease 11:177–182. https://doi.org/10.1159/000047635
Fisher RS, Acevedo C, Arzimanoglou A et al (2014) ILAE official report: a practical clinical definition of epilepsy. Epilepsia 55:475–482. https://doi.org/10.1111/epi.12550
Masuhr F, Busch M, Amberger N et al (2006) Risk and predictors of early epileptic seizures in acute cerebral venous and sinus thrombosis. Eur J Neurol 13:852–856. https://doi.org/10.1111/j.1468-1331.2006.01371.x
Ferro JM, Canhao P, Bousser MG, Stam J, Barinagarrementeria F (2008) Early seizures in cerebral vein and dural sinus thrombosis: risk factors and role of antiepileptics. Stroke 39:1152–1158. https://doi.org/10.1161/STROKEAHA.107.487363
Li H, Cui L, Chen Z, Chen Y (2019) Risk factors for early-onset seizures in patients with cerebral venous sinus thrombosis: a meta-analysis of observational studies. Seizure 72:33–39. https://doi.org/10.1016/j.seizure.2019.09.006
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2013) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 1 Apr 2022
Buccino G, Scoditti U, Patteri I, Bertolino C, Mancia D (2003) Neurological and cognitive long-term outcome in patients with cerebral venous sinus thrombosis. Acta Neurol Scand 107:330–335. https://doi.org/10.1034/j.1600-0404.2003.00031.x
Ferro J, Correia M, Rosas MJ, Pinto A, Naves G (2003) Seizures in cerebral vein and dural sinus thrombosis. Cerebrovasc Dis 15:78–83. https://doi.org/10.1159/000067133
Davoudi V, Keyhanian K, Saadatnia M (2013) Risk factors for remote seizure development in patients with cerebral vein and dural sinus thrombosis. Seizure 23:135–139. https://doi.org/10.1016/j.seizure.2013.10.011
Sánchez van Kammen M, Lindgren E, Silvis S et al (2020) Late seizures in cerebral venous thrombosis. Neurology 95:10–12. https://doi.org/10.1212/WNL.0000000000010576
Gasparini S, Ascoli M, Brigo F et al (2020) Younger age at stroke onset but not thrombolytic treatment predicts poststroke epilepsy: an updated meta-analysis. Epilepsy Behav 104:106540. https://doi.org/10.1016/j.yebeh.2019.106540
Merkler AE, Gialdini G, Lerario MP et al (2018) Population-based assessment of the long-term risk of seizures in survivors of strokE. Stroke 49:1319–1324. https://doi.org/10.1161/STROKEAHA.117.020178
Hesdorffer DC, Benn EK, Cascino GD, Hauser WA (2009) Is a first acute symptomatic seizure epilepsy? Mortality and risk for recurrent seizure. Epilepsia 50:1102–1108. https://doi.org/10.1111/j.1528-1167.2008.01945.x
Löscher W (2017) Animal models of seizures and epilepsy: past, present, and future role for the discovery of antiseizure drugs. Neurochem Res 42:1873–1888. https://doi.org/10.1007/s11064-017-2222-z
French JA, Perucca E (2020) Time to start calling things by their own names? The case for antiseizure medicines. Epilepsy Curr 20:69–72. https://doi.org/10.1177/1535759720905516
Ferro JM, Bousser MG, Canhao P et al (2017) European Stroke Organization guideline for the diagnosis and treatment of cerebral venous thrombosis- endorsed by the European Academy of Neurology. Eur J Neurol 24:1203–1213. https://doi.org/10.1111/ene.13381
Küçükkaya B, Aker R, Yüksel M, Onat F, Yalçin AS (1998) Low dose MK-801 protects against iron-induced oxidative changes in a rat model of focal epilepsy. Brain Res 88:133–136. https://doi.org/10.1016/s0006-8993(97)01544-8
Willmore LJ (1993) Post-traumatic seizures. Neurol Clin 11:823–834
Ferlazzo E, Gasparini S, Beghi E et al (2016) Epilepsy in cerebrovascular diseases: review of experimental and clinical data with meta-analysis of risk factors. Epilepsia 57:1205–1214. https://doi.org/10.1111/epi.13448
Uluduza D, Midib I, Duman T et al (2020) Epileptic seizures in cerebral venous sinus thrombosis: subgroup analysis of VENOST study. Seizure 78:113–117. https://doi.org/10.1016/j.seizure.2020.02.017
Ruiz-Sandoval JL, Chiquete E, Banuelos-Becerra LJ et al (2012) Cerebral venous thrombosis in a Mexican multicenter registry of acute cerebrovascular disease: the RENAMEVASC study. Journal of Stroke and Cerebrovascular Disease 21:395–400. https://doi.org/10.1016/j.jstrokecerebrovasdis.2011.01.001
Ostovan VR, Foroughi R, Rostami M et al (2021) Cerebral venous sinus thrombosis associated with COVID-19: a case series and literature review. J Neurol 268:3549–3560. https://doi.org/10.1007/s00415-021-10450-8
Sharifian-Dorche M, Bahmanyar M, Sharifian-Dorche A, Mohammadi P, Nomovi M, Mowla A (2021) Vaccine-induced immune thrombotic thrombocytopenia and cerebral venous sinus thrombosis post COVID-19 vaccination; a systematic review. J Neurol Sci 428:117607. https://doi.org/10.1016/j.jns.2021.117607
Acknowledgements
We thank the Epilepsy study group of the Italian Neurological Society (Amedeo Bianchi, Maria Sofia Cotelli, Fabrizio A. De Falco, Giovanni De Maria, Gian Luigi Gigli, Maria Adele Latella, Adriana Magaudda, Antonella Murroni, Leandro Provinciali, Antonio Siniscalchi, Flavio Villani).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
None.
Informed consent
None.
Registration and protocol
No separate protocol was previously developed or registered.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gasparini, S., Neri, S., Brigo, F. et al. Late epileptic seizures following cerebral venous thrombosis: a systematic review and meta-analysis. Neurol Sci 43, 5229–5236 (2022). https://doi.org/10.1007/s10072-022-06148-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-06148-y