Abstract
Objective
To report a de novo splicing mutation in the CSF1R gene in a patient with hereditary diffuse leukoencephalopathy with spheroids (HDLS).
Methods
A 42-year-old Chinese woman with constant weakness on her left lower extremity was recruited in the current study. Detail medical history and clinical characteristics were reviewed. Brain magnetic resonance imaging (MRI), whole-exome sequencing, and Sanger sequencing were performed with bioinformatics analysis.
Results
The Chinese HDLS patient with no HDLS family history exhibited a de novo splicing mutation (c.1754-10 T > A) in the CSF1R gene. This mutation was located at the splice site of intron 12 and resulted in the skipping of exon 13 from the CSF1R mRNA. This finding constitutes the first de novo splicing mutation ever reported in HDLS. Furthermore, MRI abnormalities had been reported at least 6 months prior to the onset of the patient’s clinical phenotype.
Conclusion
Our study indicates that the diagnosis of HDLS should be considered even in the absence of a family history and can help deepen the clinical and genetic understanding of HDLS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hereditary diffuse leukoencephalopathy with spheroids (HDLS) is a rare autosomal dominant inherited disease first described by Axelsson R et al. in a Swedish family in 1984 [1]. It is a neurodegenerative disease characterized by the adult onset of progressive cognitive impairment, stroke-like motor disorders, behavioral and emotional changes, sensory disturbance, epilepsy, and dizziness, among others [2, 3]. Brain magnetic resonance imaging (MRI) of patients with HDLS reveals asymmetric leukoencephalopathy, with the main involvement of frontoparietal deep white matter, as well as brain atrophy [3, 4]. Neuropathological features included degeneration of cerebral white matter (WM) and atrophy of the corpus callosum [5]. Histopathologic studies demonstrated loss of myelinated fibers and abundant axonal spheroids mainly containing aggregates of intermediate filaments or organelles that were predominantly vesicular and lamellar [6].
The diagnosis of HDLS is challenging owing to its significantly variable phenotypes [7]. It is easily misdiagnosed with other leukoencephalopathy, small vessel diseases, and neurodegenerative diseases such as frontotemporal dementia (FTD). In 2012, mutations in the colony-stimulating factor 1 receptor (CSF1R) gene, located on chromosome 5 (5q32), were identified as the cause of HDLS [8]. The CSF1R is a cell surface receptor which is crucial in development and innate immunity in the central nervous system [9]. In this study, we report a de novo splicing mutation (c.1754-10 T > A) in the CSF1R gene in a HDLS Chinese patient with no family history of the disease. The mutation was located at the splice site of intron 12, which resulted in the skipping of exon 13 from the CSF1R mRNA. Although more than 60 loci mutations in the CSF1R gene have been linked to HDLS [10, 11], de novo mutations were rarely reported [7, 12, 13]. Besides, we reported the MRI changes in the different stages of the patient and found that diffusion-weighted imaging (DWI) revealed abnormal hyperintense signals even in the presymptomatic stage of HDLS.
In this study, we report detailed clinical imaging features of a Chinese HDLS patient with no HDLS family history who exhibited a de novo splicing mutation (c.1754-10 T > A) in the CSF1R gene. Overall, our study can help deepen the clinical and genetic understanding of HDLS.
Materials and methods
Patient history and clinical data
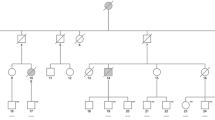
A 42-year-old Chinese woman with no medical history complained of a sudden onset of constant weakness on her left lower extremity for 2 months in October 2019. About 1 month later, her left upper limb also became weak. The patient was born at term to non-consanguineous parents following a normal pregnancy and delivery. At the age of 23, the patient gave birth to a healthy baby girl. The patient was admitted to the local hospital and administered platelet aggregation inhibitor, statins, and other drugs. Her condition gradually improved and she could walk normally when she came to our hospital for further examination.
Physical examination
At the time of admission to our hospital, the patient’s blood pressure was 122/71 mmHg, and her heart rate was 75 beats per minute. She had no significant deficits in memory, directive force, and learning or calculation abilities. Furthermore, no obvious deficits were observed in the cranial nerve examinations, and the muscle force of all the limbs was level 5. The muscular tension of her left limbs increased, which led to positive Babinski and Chaddock signs. Her mini-mental state examination (MMSE) score was 24 points, and her Montreal Cognitive Assessment (MoCA) score was 22 points.
DNA extraction
With the informed consent of the patient, 2 mL of blood was collected, and DNA was extracted by a genomic DNA extraction kit (Quan-Jin Biotech Co., Ltd., Beijing, China). Finally, DNA purity and integrity were assessed using spectrophotometry (Thermo Fisher Scientific, Waltham, MA, USA) and agarose gel electrophoresis, respectively.
Whole-exome sequencing (WES) and data analysis
WES was performed by Annoroad Genomics Co., Ltd. (Beijing, China) and the methods were based on previous studies [14, 15]. The AgilentV6 exon targeting sequence enrichment system was used to capture the whole-exome sequences, and the enriched sequences were double-ended sequenced by Hiseq sequencing platform (PE150). The coverage of the target area was more than 99%, and the average depth of the target area was higher than 20 × , accounting for 98% of all sequencing depths. The original sequencing data of the patients were mapped to the human reference genome UCSC HG19 through the comparison software BWA, and the comparison result file in BAM format was obtained. The mutation analysis software GATK was used to analyze all the mutation sites, and Annoroad software was used to make functional annotations for all the mutation sites.
Validation by Sanger sequencing
Sanger sequencing was performed in the protestors to validate identified pathogenic variants using whole-exome sequencing. CSF1R-F: GCTG CCCT GTCA CTGT GTA and CSF1R-R: TCGT TTCC CATC CCAG GA are based on the reference genome sequence of the human genome from NCBI GenBank by Primer 3 designed for the candidate locus and PCR under the following conditions: 95 °C/4-min initial denaturation, followed by 95 °C/30-s denaturation 30 cycles, 52 °C/30-s annealing, 72 °C/45-s extension, and 72 °C/5-min extension.
RT-PCR analysis
Total RNA was extracted from the peripheral blood of the patient and a healthy control. Reverse transcription of RNA into cDNA was performed using the TaKaRa RNA PCR Kit according to the manufacturer’s protocol. The cDNA was amplified with primers (F: CCGG ATGA GTTC CTCT TCAC, R: CATG ATCT TCAG CTCG GACA) spanning from exons 11 to 14. We then separated the RT-PCR products using 2% agarose gel. Sanger sequencing was also performed on the cDNA.
Results
MRI scan
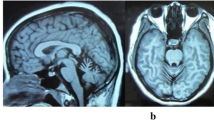
During a routine checkup in March 2019, DWI hyperintense signals were observed in the bilateral corona radiata, the splenium of the corpus callosum, the centrum semiovale, and the right basal ganglia region (Fig. 1A). The patient did not take these signs seriously and refused further examinations as she had no neurological symptoms. In October 2019, when she complained of the weakness of her left lower limb, brain MRI revealed multiple patchy high T1 and T2 signals in the splenium of the corpus callosum, the bilateral corona radiata regions (more significantly on the right side), the centrum semiovale, and the right basal ganglia region. T2 fluid-attenuated inversion recovery (FLAIR) and DWI revealed more hyperintense signals in the right corona radiata regions and the centrum semiovale than those in March 2019. Finally, contrast-enhanced MRI scan revealed no obvious abnormal intensification (Fig. 1B), and magnetic resonance angiography did not indicate vascular stenosis in the brain.
Magnetic resonance imaging (MRI) of the patient. A In March 2019, when the proband had no symptoms, the fluid-attenuated inversion recovery (FLAIR) and diffusion-weighted imaging (DWI) hyperintense signals were observed in the bilateral corona radiata, the splenium of corpus callosum, and the right basal ganglia region. B In October 2019, when the proband complained of the weakness of her left lower limb, MRI demonstrated more abnormal signals in the right corona radiata regions and the centrum semiovale than those in March 2019
Laboratory findings and cerebrospinal fluid (CSF) test
A blood routine test of the patient revealed a hemoglobin (Hb) concentration of 94 g/L, a hematocrit of 31.2%, a mean corpuscular volume of 78.4 fL, and an erythrocyte sedimentation rate of 42 mm/h. Other blood analyses, including hepatorenal function, C-reactive protein, vitamin B12, TORCH screening, tumor makers, anti-neutrophil cytoplasmic (ANCA) antibody, anti-extractable nuclear (ENA) antibody, thyroid function, adrenocorticotropic hormone, syphilis serology, and HIV test, were all normal/negative. The CSF pressure was 140 mmH2O. Moreover, the number of lymphocytes, the protein level, and the biochemical tests of the CSF were in the normal range. Finally, specific antibodies (AQP4/MOG/MBP) did not detect any signs of demyelinating diseases in the central nervous system (CNS).
Genetic tests
To identify the presence of inherited diseases, we extracted genomic DNA from the peripheral blood of the patient and performed WES. WES revealed a c.1754-10 T > A mutation in the CSF1R gene (Fig. 2A II-1). The presence of this mutation was confirmed by Sanger sequencing (Fig. 2B). The mutation was not observed in other family members (the patient’s parents and daughter) who exhibited no neurological symptoms. The mutation was absent in the Exome Aggregation Consortium database, the 1000 Genomes Project, and the Human Gene Mutation Database. The variant was highly conserved in different species (as observed using the MutationTaster software). Both the SIFT and PolyPhen-2 software predicted that this mutation was deleterious on the CSF1R protein structure and function. Subsequently, we extracted the total RNA from the peripheral blood of the patient and from a healthy control to determine the influence of the mutation on mRNA splicing. RNA was reverse transcript into cDNA, and then, cDNA was amplified with primers spanning from exons 11 to 14. Agarose gel showed only one 459-bp band in the sample of the healthy control and two bands in the patient’s sample, one with 459 bp and another smaller than 459 bp (Fig. 3A). This suggests that the mutation produced a truncated, alternatively spliced isoform. Sanger sequencing was also performed on the cDNA, confirming that the c.1754-10 T > A mutation on the CSF1R gene caused exon 13 skipping during mRNA splicing (Fig. 3B).
Diagnosis and prognosis
At first, the patient was diagnosed with acute ischemic stroke and treated with aspirin enteric-coated tablets (100 mg/day), clopidogrel (75 mg/day), and atorvastatin (20 mg/day). After a series of routine examinations, we considered that she suffered from “acute ischemic stroke due to unknown reasons,” possible “primary angiitis of the central nervous system (PACNS),” and “iron deficiency anemia.” She was then given diagnosis therapy consisting of a glucocorticoid and an immunosuppressor. Then, the genetic test revealed the mutation in the CSF1R gene. Based on the clinical symptoms, MRI characteristics, and genetic test, the proband was diagnosed with HDLS. One year later in October 2020, the patient suffered from recurrent weakness of the left limbs. At that time, brain MRI revealed more abnormal signals in the splenium and rostrum of the corpus callosum, bilateral corona radiata regions, centrum semiovale, and right corticospinal tract, which significantly progressed than in 2019 (Fig. 4).
Discussion
Here, we reported a de novo splicing mutation (c.1754-10 T > A) in the CSF1R gene in a Chinese HDLS patient with no family history of the disease. The age of the disease onset was 42 years old, which is consistent with the previous literature. HDLS often occurs in the age range of 40–50 years, but this has also been found to occur in the age range of 17–78 years [16, 17]. The pathological basis of HDLS is diffuse leukoencephalopathy with spheroids or demyelination [18]. Prominent clinical symptoms related with leukoencephalopathy include cognitive impairment as well as emotion and motor disorders, among others [19, 20]. In this case report, a female patient experienced stroke-like manifestations, and her hemiparesis was associated with an abnormality in the right corticospinal tract.
Like most HDLS patients, this patient went through a series of medical complications before being diagnosed, suggesting that HDLS should be differentiated from a number of diseases, especially other types of leukodystrophies, such as autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL), Alexander disease, X-linked adrenoleukodystrophy, and metachromatic leukodystrophy [7, 21]. CADASIL usually manifests itself through migraines, stroke-like episodes, and dementia, and the involvement of the temporal tip could be considered pathognomonic [22]. In the case of Alexander disease, MRI usually reveals that the brainstem, specifically the medulla region, is involved [23]. Conversely, enzymatic tests are helpful for the diagnosis of X-linked adrenoleukodystrophy and metachromatic leukodystrophy [24]. The case described here should also be differentiated from acute ischemic stroke. In HDLS, continuous hyperintense signals are observed in DWI, and in acute ischemic stroke, these signals are only detected in an early stage of the disease.
Brain MRI of HDLS patients is characterized by high, bilateral, symmetrical, or asymmetrical white matter T2 signals. The frontotemporal lobes, corpus callosum, and U-fibers are typically affected [25], whereas the involvement of the thalamus and basal ganglia is rarely reported [3]. Furthermore, DWI demonstrates a restricted diffusion of these lesions. Notably, in the case reported here, MRI abnormalities have been observed at least 6 months prior to the onset of the clinical symptoms, which indicates that the typical imaging changes in HDLS preceded the onset of the clinical phenotype. Our finding is in accordance with that of Van Gerpen et al. [26], who reported an asymptomatic imaging study with frontal white matter abnormalities detected 5 years before the onset of the clinical symptoms.
In 2011, Rademakers et al. [12] confirmed that a mutation in the CSF1R gene was the genetic basis of HDLS. The CSF1R gene includes 24 exons and encodes for the CSF1R protein, which contains 972 amino acid residues [27]. Until now, more than 60 CSF1R mutations, including missense mutations, point mutations, frameshift mutations, and splicing mutations, have been identified as the genetic cause of HDLS [28]. HDLS is an autosomal dominant disease, but the reported sporadic cases [7, 12, 13] suggested that the diagnosis of HDLS should be suspected even in the absence of a positive family history. It is worth noting that although dozens of mutations have been identified in HDLS, the occurrence of de novo mutations was very rare [7, 12, 13]. Here, we confirmed a de novo c.1754-10 T > A mutation in a proband with no family history of HDLS, as confirmed by paternity tests. This finding also constitutes the first de novo splicing mutation ever reported in this disease.
CSF1R is a cell surface receptor for the CSF-1 factor and contains five immunoglobulin-like, extracellular ligand-binding domains; one transmembrane domain; and one tyrosine kinase intracellular domain [29]. CSF1R plays significant roles in regulating proliferation, survival, and differentiation of mononuclear phagocytic cells [30]. In the CNS, CSF1R is particularly highly expressed in microglial cells [31]. Most of the pathogenic mutations are located in the tyrosine kinase domain (encoded by exons 12 to 21 [32]) and can abrogate the CSF1R kinase activity, which affects the phosphorylation of downstream targets [13]. Of note, the mutation reported here is located at intron 12 and thus within the tyrosine kinase domain. Similar to our results, Xiaodong Yang et al. [21] reported a splicing mutation (c.1858 + 1G > T) in intron 13, which led to exon 13 skipping. In that study, the proband manifested progressive memory loss, slurred speech, limb stiffness, and weight loss, which are different from the symptoms reported in the present study. This difference highlights the significant clinical and genetic heterogeneities in HDLS [7]. Even so, we guess cognitive impairment and other clinical symptoms will appear a few months or years later because extensive white matter was involved in this patient. The prognosis of the patient is not optimistic as the abnormality progressed rapidly and there is no specific treatment for HDLS.
Conclusion
In conclusion, we reported detailed clinical imaging features of an HDLS patient with no family history of this disease. In addition, we identified a de novo c.1754-10 T > A mutation in intron 12, which resulted in the skipping of exon 13 from the CSF1R mRNA. We also suggested that this skipping may further affect the normal function of the protein. This research indicated that HDLS should be taken into consideration even in the absence of family history. Persistent DWI hyperintense signals and genetic test are necessary to perform to differentiate HDLS from other diseases. Our study brings attention to the existence of a significant clinical heterogeneity in HDLS patients and contributes to the genetic understanding of this disease. Several limitations of this study must be addressed. First, the pathological examination of the proband’s brain tissue was unable to perform. Second, the specific function of CSF1R mutations was still unclear. We will perform functional experiments to elucidate the pathogenesis of CSF1R mutations in our future work.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Axelsson R (1984) Hereditary diffuse leucoencephalopathy with spheroids. Acta Psychiat Scand 314:1–65. https://doi.org/10.1136/jnnp.74.9.1345
Nicholson AM, Baker MC, Finch NA et al (2013) CSF1R mutations link POLD and HDLS as a single disease entity. Neurology 80:1033–1040. https://doi.org/10.1212/WNL.0b013e31828726a7
Stabile C, Taglia I, Battisti C et al (2016) Hereditary diffuse leukoencephalopathy with axonal spheroids (HDLS): update on molecular genetics. Neurol Sci 37:1565–1569. https://doi.org/10.1007/s10072-016-2634-6
Sundal C, Jönsson L, Ljungberg M et al (2014) Different stages of white matter changes in the original HDLS family revealed by advanced MRI techniques. J Neuroimaging 24:444–452. https://doi.org/10.1111/jon.12037
Sundal C, Lash J, Aasly J et al (2012) Hereditary diffuse leukoencephalopathy with axonal spheroids (HDLS): a misdiagnosed disease entity. J Neurol Sci 314:130–137. https://doi.org/10.1016/j.jns.2011.10.006
Baba Yasuhiko, Ghetti Bernardino, Baker Matthew C et al (2006) Hereditary diffuse leukoencephalopathy with spheroids: clinical, pathologic and genetic studies of a new kindred. Acta Neuropathol 111:300–311. https://doi.org/10.1007/s00401-006-0046-z
Karle KN, Biskup S, Schüle R et al (2013) De novo mutations in hereditary diffuse leukoencephalopathy with axonal spheroids (HDLS). Neurology 81:2039–2044. https://doi.org/10.1212/01.wnl.0000436945.01023.ac
Foulds N, Pengelly RJ, Hammans SR et al (2015) Adult-onset leukoencephalopathy with axonal spheroids and pigmented glia caused by a novel R782G mutation in CSF1R. Sci Rep 5:1–7. https://doi.org/10.1038/srep10042
Richard Stanley E, Chitu V et al (2014) CSF-1 receptor signaling in myeloid cells. Cold Spring Harb Perspect Biol 6:a021857. https://doi.org/10.1101/cshperspect.a021857
Adams SJ, Kirk A, Auer RN (2018) Adult-onset leukoencephalopathy with axonal spheroids and pigmented glia (ALSP): integrating the literature on hereditary diffuse leukoencephalopathy with spheroids (HDLS) and pigmentary orthochromatic leukodystrophy (POLD). J Clin Neurosci 48:42–49. https://doi.org/10.1016/j.jocn.2017.10.060
Miura T, Mezaki N, Konno T et al (2018) Identification and functional characterization of novel mutations including frameshift mutation in exon 4 of CSF1R in patients with adult-onset leukoencephalopathy with axonal spheroids and pigmented glia. J Neurol 265:2415–2424. https://doi.org/10.1007/s00415-018-9017-2
Rademakers R, Baker M, Nicholson AM et al (2012) Mutations in the colony stimulating factor 1 receptor (CSF1R) gene cause hereditary diffuse leukoencephalopathy with spheroids. Nat Genet 44:200–205. https://doi.org/10.1038/ng.1027
Kondo Y, Kinoshita M, Fukushima K et al (2013) Early involvement of the corpus callosum in a patient with hereditary diffuse leukoencephalopathy with spheroids carrying the de novo K793T mutation of CSF1R. Internal Med 52:503–506. https://doi.org/10.2169/internalmedicine.52.8879
Oosterhof N, Chang IJ, Karimiani EG et al (2019) Homozygous mutations in CSF1R cause a pediatric-onset leukoencephalopathy and can result in congenital absence of microglia. Am J Hum Genet 104:936–947. https://doi.org/10.1016/j.ajhg.2019.03.010
Nasirshalal M, Panahi M, Javanshir N et al (2021) Identification of a novel heterozygous mutation in the MITF gene in an Iranian family with Waardenburg syndrome type II using next-generation sequencing. J Clin Lab Anal 35:e23792. https://doi.org/10.1002/jcla.23792
Ikeda S (2012) Hereditary diffuse leukoencephalopathy with axonal spheroids (HDLS): its clinical concept and the review of the previously reported cases. Clin Neurol 52:1383–1385. https://doi.org/10.5692/clinicalneurol.52.1383
Wong JC, Chow TW, Hazrati L-N (2011) Adult-onset leukoencephalopathy with axonal spheroids and pigmented glia can present as frontotemporal dementia syndrome. Dement Geriatr Cogn 32:150–158. https://doi.org/10.1159/000331422
Eichler FS, Li J, Guo Y et al (2016) CSF1R mosaicism in a family with hereditary diffuse leukoencephalopathy with spheroids. Brain 139:1666–1672. https://doi.org/10.1093/brain/aww066
Sundal C, Baker M, Karrenbauer V et al (2015) Hereditary diffuse leukoencephalopathy with spheroids with phenotype of primary progressive multiple sclerosis. Eur J Neurol 22:328–333. https://doi.org/10.1111/ene.12572
Freeman SH, Hyman BT, Sims KB et al (2009) Adult onset leukodystrophy with neuroaxonal spheroids: clinical, neuroimaging and neuropathologic observations. Brain Pathol 19:39–47. https://doi.org/10.1111/j.1750-3639.2008.00163.x
Yang X, Huang P, Tan Y et al (2019) A novel splicing mutation in the CSF1R gene in a family with hereditary diffuse leukoencephalopathy with axonal spheroids. Front Genet 10:491. https://doi.org/10.3389/fgene.2019.00491
Liao N-Y, Liao K-K, Liao Y-C et al (2021) Mitochondrial DNA m. 3243A> G mutation rarely causes CADASIL-like phenotype. Neurobiol Aging 97:145-e145. https://doi.org/10.1016/j.neurobiolaging.2020.08.016
Namekawa M, Takiyama Y, Honda J et al (2010) Adult-onset Alexander disease with typical" tadpole" brainstem atrophy and unusual bilateral basal ganglia involvement: a case report and review of the literature. Bmc Neurol 10:1–6. https://doi.org/10.1186/1471-2377-10-21
Aicardi J (1993) The inherited leukodystrophies: a clinical overview. J Inherit Metab Dis 16:733–743. https://doi.org/10.1007/BF00711905
Granberg T, Hashim F, Andersen O et al (2016) Hereditary diffuse leukoencephalopathy with spheroids–a volumetric and radiological comparison with multiple sclerosis patients and healthy controls. Eur J Neurol 23:817–822. https://doi.org/10.1111/ene.12948
Van Gerpen JA, Wider C, Broderick DF et al (2008) Insights into the dynamics of hereditary diffuse leukoencephalopathy with axonal spheroids. Neurology 71:925–929. https://doi.org/10.1212/01.wnl.0000325916.30701.21
Shi T, Li J, Tan C et al (2019) Diagnosis of hereditary diffuse leukoencephalopathy with neuroaxonal spheroids based on next-generation sequencing in a family: case report and literature review. Medicine 98:e15802. https://doi.org/10.1097/MD.0000000000015802
Zhuang L-P, Liu C-Y, Li Y-X et al (2020) Clinical features and genetic characteristics of hereditary diffuse leukoencephalopathy with spheroids due to CSF1R mutation: a case report and literature review. Ann Transl Med 8:1–7. https://doi.org/10.21037/atm.2019.12.17
Pixley FJ, Stanley ER (2004) CSF-1 regulation of the wandering macrophage: complexity in action. Trends Cell Biol 14:628–638. https://doi.org/10.1016/j.tcb.2004.09.016
Sullivan AR, Pixley FJ (2014) CSF-1R signaling in health and disease: a focus on the mammary gland. J Mammary Gland Biol 19:149–159. https://doi.org/10.1007/s10911-014-9320-1
Ginhoux F, Greter M, Leboeuf M et al (2010) Fate mapping analysis reveals that adult microglia derive from primitive macrophages. Science 330:841–845. https://doi.org/10.1126/science.1194637
Lynch DS, Brandão R, de Paiva A, Zhang WJ et al (2017) Clinical and genetic characterization of leukoencephalopathies in adults. Brain 140:1204–1211. https://doi.org/10.1093/brain/awx045
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The project was approved by the ethics committee of Qilu Hospital of Shandong University.
Consent to participate
We obtained informed written consent from the patient and her family in this study and publication of their clinical data.
Consent for publication
All authors read and approved the final version of the present research manuscript and agreed to be accountable for all aspects of the work.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, X., Sun, C., Wang, X. et al. Identification of a de novo splicing mutation in the CSF1R gene in a Chinese patient with hereditary diffuse leukoencephalopathy with spheroids. Neurol Sci 43, 3265–3272 (2022). https://doi.org/10.1007/s10072-021-05755-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05755-5