Abstract
The Rivermead assessment of somatosensory performance (RASP) provides a quantitative assessment of somatosensory processing, suitable for brain-damaged patients suffering from stroke. It consists of seven subcomponents: Subtest 1 (sharp/dull discrimination), Subtest 2 (surface pressure touch), Subtest 3 (surface localization), Subtest 4 (sensory extinction), Subtest 5 (2-point discrimination), Subtest 6 (temperature discrimination), and Subtest 7 (proprioception). Overall, the RASP assesses 5 bilateral body regions: face (cheek), hand (palm and back), and foot (sole and back). This study aimed at providing normative data and cut-off scores for RASP subtests, for each body region, in a large Italian population sample. We present results from 300 healthy Italian individuals aged 19 to 98 years. Data represent a comprehensive set of norms that cover each subtest and each body region tested. Performance in Subtests 1, 5, and 6 decreased, for some body regions, with increasing age. Based on these results, norms were stratified for age (seven groups), with the pathological/non-pathological cut-off coinciding with the 5th percentile. Conversely, other results were not influenced by age; in such cases, a single error, in each body region, has to be considered indicative of pathological performance. This independent investigation of all subcomponents of the somatosensory system, for each body region, further confirms RASP’s potential in clinical practice, for neurological assessment, as well as in research settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The examination of somatic sensation requires the assessment of a range of different processes, including tactile detection, acuity, pain, proprioception, vibration, temperature sensitivity, and stereognosis [1]. Somatosensory dysfunctions occur in many neurological conditions, affecting both the central and the peripheral nervous system [2]. In stroke, about 6 out of 10 survivors suffer from some somatosensory impairment [3], with different incidence among studies [4] due to various factors, as severity and level of impairment [5]. Another important source of variability is related to the affected body region [4]. Noteworthy, in clinical practice, somatic sensation is commonly dichotomously determined as being “present” or “absent” [5].
Somatosensory deficits are considered a negative predictor of functional outcome after stroke [6]: their presence is associated with motor activity limitations and a longer length of stay in hospital or nursing home [7]. Furthermore, somatic sensation is functionally interconnected with motor performance [8]; hence, it largely influences motor recovery after stroke [9]. Somatosensory deficits after unilateral stroke primarily affect the side of the body contralateral to the hemispheric lesion (contralesional), sometimes extending to the ipsilesional side [5, 10, 11].
In clinical practice, the main standardized tools available include the Fugl Meyer Sensory Scale — FMSs [12], the Nottingham Sensory Assessment — NSA [13], the Quantitative Sensory Testing — QST [14], and the Rivermead Assessment of Somatosensory Performance — RASP [15]; for reviews, see [4, 16].
The RASP [15] developed at the Rivermead Rehabilitation Center in Oxford provides a quantitative examination of 5 bilateral body parts: face (cheek), hand (palm and back), and foot (sole and back). The RASP comprises seven subtests, divided into five “primary” (sharp/dull discrimination, surface pressure touch, surface localization, temperature discrimination, and movement and direction proprioception) and two “secondary” (extinction and 2-point discrimination) ones. The RASP features a precise and validated protocol and shows good psychometric properties: test-retest (r = .92), inter-tester (r = .92) reliability, and validity (s = .52–.54). Moreover, the RASP can be used to assess somatosensory performance of patients in the sub-acute stage after stroke, providing information regarding deficits and recovery of somatosensory functions [9]. The RASP was first validated in UK in a sample of 100 post-stroke brain-damaged patients and in 50 age-matched healthy participants [15] and then in Germany in 60 stroke patients, showing a good-to-excellent inter-rater reliability across subtests [17]. The battery has the advantage of being short (the assessment lasts about 25–35 min), easy to administer, and simple to score [18]. The use of the RASP has been also recommended, due to its interval scales, for statistical analyses [4].
The present study provides RASP normative data in a sample of Italian healthy participants.
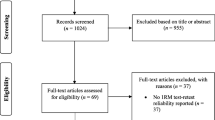
Materials and methods
Participants
Three-hundred Italian, neurologically healthy, individuals, with no history or evidence of neurological or psychiatric disorders, entered this study. The sample comprised 124 males (M) and 176 females (F), with a mean age of 50.8, standard deviation (SD) = ±21.1 years (M = 53.1 ± 20, F = 49.2 ± 22), and a mean schooling of 12.8 ± 4.3 years (M = 13 ± 4, F = 12.7 ± 4). Following a standardized interview [19], six participants were classified as left-handed (2% of the total), 2 ambidextrous (0.07%), and 298 (97.3%) right-handed. The study conformed to Declaration of Helsinki and was approved by the ethical committee of the IRCCS Istituto Auxologico Italiano.
Procedure
RASP tools
The RASP kit comprises three bespoke instruments: the Neurometer, the Neurotemp, and the Neurodisc, shown in Fig. 1. The Neurometer is a pen-shaped device that allows a given amount of pressure to be applied to an area. This instrument provides two different amounts of pressure (i.e., 15.5 or 67.5 g). On the top, a sterile single-use pin, called a Neurotip, can be inserted. Neurotips are either sharp or dull. The RASP kit provided 2 Neurometers in order to allow a double stimulation (see below). The Neurodisc is the tool used for testing 2-point discrimination, with three distances: 3, 4, and 5 mm.
RASP instruments. a Neurometer: a pen-shaped device that allows two amounts of pressure (i.e., 15.5 or 67.5 g) to be applied to the target body area. On its superior top, a single-use Neurotip (sharp or dull) could be inserted; b Neurodisc: 2-point discriminator with fixed distances of 3, 4, and 5 mm; there is also a single-point tip; c Neurotemp: LCD temperature devices
The Neurotemps (1 red and 1 blue) are simple temperature devices with liquid crystal display (LCD). The red Neurotemp is used to deliver a “warm” stimulation, of about 44–49 °C, brought by immerging the instrument in boiled water for around 30 s. The blue Neurotemp, after immersion in ice water for about 30 s, delivers a “cold” stimulation, of about 6–10 °C. Before testing, RASP tools are shown to the participant, along with a brief description of each subtest.
RASP subtests
The RASP was administered following the original instructions [15, 18], translated into Italian. The RASP comprised seven subtests, delivered to participants, who had received instructions to keep their eyes closed throughout the testing session. In each task, participants were encouraged not to worry if they did not feel a given stimulus, rather just to do their best to perform the task. The number of correct responses, for each region, was manually recorded on the scoring sheet. In the following, a brief description of each subtest is provided; stimulus order and randomization followed the original protocol [18].
Subtest 1: sharp/dull discrimination
Two Neurometers were used. On each Neurometer, a sterile, single-use Neurotip (one with a sharp and one with a dull end) was inserted. For this subtest, the sharp or dull stimulus was applied on each test region. Participants were instructed to report, for each trial, which kind of stimulation (“sharp” or “dull”) was felt. For each region, eight stimuli were presented: three dull (D), three sharp (S), and two sham (§) trials in the following order: S-§-D-D-S-S-§-D. In sham trials, the Neurometer was applied nearby the body (within 15 cm), emitting the same audible sound of the test stimulus, but avoiding any contact with the participant’s skin. Sixty trials (30 left, 30 right) and 20 § stimuli (10 left, 10 right) were administered to ten body regions: right and left face, right and left hand (palm and back), and right and left foot (sole and back).
Subtest 2: surface pressure touch
This subtest was administered using one Neurometer set to deliver a 15.5 g pressure. A series of single stimuli was applied, in a real (touch) or sham (non-touch) fashion, on each test region. The order and the type (touch or non-touch) of the stimulations were pseudo-randomized as in the original protocol. Sham trials consisted in non-touch stimuli applied as in Subtest 1. Participants were instructed to report, in each trial, whether or not they had felt the stimulation. For each region, six touch (T) and two sham (§) trials were delivered in the following order: T-§-T-T-T-T-§-T. Sixty trials (30 left, 30 right) and 20 § stimuli (10 left, 10 right) were administered to ten body regions: right and left face, right and left hand (palm and back), and right and left foot (sole and back).
Subtest 3: surface localization
This subtest required one Neurometer, set to deliver a 15.5 g pressure. Participants had to report, in each trial, on which body side (right or left) the stimulus had been applied. Sixty stimuli (30 left and 30 right) were administered to the face, palm and back hand, and sole and back foot. For each body area, 12 stimuli were presented (6 for each side), in a pseudo-randomized order.
Subtest 4: sensory extinction
Both Neurometers were used, set to a 67.5 g pressure. Participants were instructed to report, in each trial, on which body side (right or left or both) the stimulus was applied. Following a pseudo-randomized order, the evaluator applied the stimulus on the right, on the left, or on both sides, simultaneously, of the following regions: face and hands (on the back). For each region, six bilateral (B) and two unilateral (one left, L, and one right, R) stimuli were presented in the following order: B-L-B-B-B-B-R-B. For the two body parts, 12 bilateral and four single trials were given.
Subtest 5: 2-point discrimination
The Neurodisc was applied on the fingertip of the left and of the right index finger. In a pseudo-randomized order, the evaluator depressed the participant’s skin for approximately 1 mm before releasing, with either a single- or a 2-point tip. Participants were instructed to report which kind of stimulation (“single” or “double”) they had felt. On each index finger, eight trials were delivered: two single-point trials (1) and six 2-points trials (2) in the following order 2-1-2-2-2-2-1-2. The subtest started with the 2-point distance of 3 mm. If the participant was able to correctly report the 2 points in at least four out of six trials, the test was considered successfully completed and the 2-point discrimination threshold was considered to be 3 mm. If this was not the case, the test was repeated with a 4 mm distance; if the participant was able to correctly report the 2 points at least four out of six times, the threshold was considered to be 4 mm. If this was not the case, the test was repeated with the 5 mm 2-point distance; if the participant failed also at this distance, the subtest was considered failed.
Subtest 6: temperature discrimination
Both Neurotemps were used. Participants had to report which kind of stimulation, “warm” or “cold,” they felt. Sixty trials were administered to the 10 body regions: right and left face, right and left hand (palm and back), and right and left foot (plant and back). For each region, six stimuli were presented, three warm (W) and three cold (C), in the following order: W-C-C-W-W-C.
Subtest 7: joint movement and movement direction discrimination
The evaluator moved a participant’s joint either up or down in a pseudo-randomized sequence. Participants had to report whether they felt the movement (“Joint movement”) and in which direction (“up” or “down,” i.e., “Movement direction discrimination”). The score was the number of passive movements correctly reported (7a, “Joint movement”), and their direction (7b, “Movement direction discrimination”). The tested joints were in the right and left upper (elbow, wrist, and thumb) and lower (ankle and big toe) limbs; each joint was moved six times in the following order: up-down-down-up-up-down.
Statistical analysis
Statistical analyses were performed through IBM® SPSS® Statistics, version 25.0.
For each subtest (except Subtest 5, 2-point discrimination), the number of correct responses for each body region was considered. Specifically:
-
Subtest 1 (sharp/dull discrimination), Subtest 2 (surface pressure touch), Subtest 3 (surface localization), and Subtest 6 (temperature discrimination): right and left face, right and left hand (palm and back), and right and left foot (plant and back);
-
Subtest 4 (sensory extinction): face and (back) hands;
-
Subtest 7a (joint movement) and Subtest 7b (movement direction discrimination): right and left superior limbs (elbow, wrist, and thumb); right and left inferior limbs (ankle and big toe).
With respect to Subtest 5 (2-point discrimination), since a pass or fail scoring procedure was used, the outcome of passing (3 mm, 4 mm, 5 mm) or failing the subtest was scored.
To assess the role of demographic variables, each subtest was submitted to a Poisson linear model considering age, gender, and schooling, both independently and in interaction. Significant threshold was set at alpha = 0.05.
Scores in sham trials, which detect false positives, were not analyzed statistically, because no participant gave this kind of response in any task.
The Age variable was divided as follows: 1: ≤ 25 years (N = 42); 2: between 26 and 35 years (N = 47); 3: between 36 and 45 years (N = 43); 4: between 46 and 55 years (N = 40); 5: between 56 and 65 years (N = 36); 6: between 66 and 75 years (N = 44); 7: ≥ 76 years (N = 45).
The Schooling variable was divided as follows: 1: ≤ 5 years (i.e., elementary school, N = 30); 2: between 6 and 8 years (i.e., middle school, N = 50); 3: between 9 and 13 years (i.e., college, N = 111); 4: between 14 and 16 years (i.e., bachelor degree, N = 31); 5: ≥ 17 years (i.e., master degree, further specialization, or PhD, N = 78).
With respect to Gender, the sample was divided as follows: 1: male (N = 124); 2: female: (N = 176).
Results
For each subtest, and for each body region, chi-square (χ2) and P-values were calculated and a significant effect of Age on performance was found. Specifically, the mean correct responses, and the values corresponding to the 5th percentile for each body region, at different levels of the factor Age are provided. The pathological/non-pathological cut-off coincides with the 5th percentile. It should be noted that only the Age factor was considered, albeit the distribution of participants within Age and Schooling was not entirely independent (the two factors were correlated, with elderly participants presenting with lower schooling, and vice-versa); this option was adopted as Schooling was not expected to affect somatic sensation. The absence of significant Age × Schooling interactions (all Ps > 0.05) confirmed this prediction.
Conversely, in case of a non-significant effect of Age, the values of the mean correct responses were reported corresponding to the cut-offs, rounded to the nearest whole number.
With respect to Subtest 5, percentages of participants who successfully completed or failed the task, and the minimum distance at which they could perceive the 2 points as different, for each Age category, are presented. Then, the mean score and the value corresponding to the 5th percentile for each index finger are provided.
Subtest 1: sharp/dull discrimination
The Poisson linear model revealed a significant effect of Age with respect to the right [χ2(6) = 13.87, P = 0.031] and the left [χ2(6) = 28.66, P < 0.001] foot. Also, Schooling was significant for the same body regions: right [χ2(4) = 12.68, P = 0.013] and left [χ2(6) = 28.66, P < 0.001] foot, respectively. As no interaction Age × Schooling [P = 0.9] was found, in Table 1, values considering the variable Age only are reported.
For all the other body regions (i.e., right and left face, right and left hand) mean correct responses are reported in Table 2. This value was considered the cut-off.
Subtests 2–3–4: surface pressure touch, surface localization, sensory extinction
For each subtest, none of the models reached significance (all Ps < 0.05). Table 2 reports the values of the mean correct responses and the corresponding cut-off value: a single error, in each body region, was considered indicative of pathological performance.
Subtest 5: 2-point discrimination
The percentages of participants, who passed the subtest, are reported in Table 3 for the right and left index fingers.
In order to determine normative values, data were re-coded as follows: 3 = successful (at least 4 out of 6 correct responses) 2-point discrimination at 3 mm; 2 = successful 2-point discrimination (at least 4 out of 6) at 4 mm; 1 = 2-point successful discrimination (at least 4 out of 6) at 5 mm; 0 = failure, less than 4 (out of 6) accurate 2-point discrimination at 5 mm.
The Poisson linear model revealed a significant effect of Age for both the left [χ2(6) = 19.789, P = 0.003] and the right [χ2(6) = 21.072, P = 0.002] index. In addition, Schooling was significant for the left [χ2(6) = 9.656, P = 0.047] index, only. As no interaction Age × Schooling [P = 1] was found, Table 4 reports the mean correct responses, the 5th percentile, and the corresponding cut-off value (i.e., maximal distance to allow at least 4 out of 6 double stimuli), considering the variable Age.
Subtest 6: temperature discrimination
The Poisson linear model revealed an effect of Age for the left foot [χ2(6) = 18.173, P = 0.006]. Table 5 reports the mean correct responses, the value corresponding to the 5th percentile, and the cut-off for the left foot considering the independent variable Age.
For all the other body regions (i.e., right and left face, right and left hand, right foot), the values of the mean correct responses, which corresponds to the cut-off value, are reported in Table 2.
Subtests 7a–b: joint movement, movement direction discrimination
None of the models were significant (all Ps < 0.05); a single error, in each body region, reflected a pathological performance. Results are reported in Table 2.
Discussion
The aim of the present study was to collect normative data in a large Italian population for the RASP, providing normative values, along with cut-off scores, separately for body parts in all subtests. Validity, reliability, and test-retest and inter-rater variability had been evaluated in the original works, demonstrating good psychometric properties [15, 17].
Compared to the original study [15], the present study included a larger sample (N = 300) of neurological healthy participants (50 healthy controls in the original English version) and took into consideration the Age factor, provided cut-offs also for 2-point discrimination (Subtest 5), and scores for each tested body region.
In previous studies [15, 17], a single cut-off value was established for each subtest that did not consider potential sources of variation such as Age, Gender, and Schooling. The role of these variables was assessed in this study, both independently and in combination. Importantly, statistical analyses confirm a significant role of the factor Age, which influences performance in all the subtests assessing discrimination abilities: sharp/dull (Subtest 1), 2-point (Subtest 5), and temperature (Subtest 6). Progressive deterioration of somatosensory performance with advancing age has been reported by several investigators. For instance, tactile acuity has been shown to decrease with age, particularly over 60 years [20,21,22], as well as joint proprioception, which becomes less accurate [23, 24].
Conversely, neither Gender nor Schooling factors were found to affect somatosensory processing in healthy participants. The lack of gender effects is in keeping with previous evidence showing the absence of sex difference in the same sensory tasks used here, while it seems to influence more complex haptic tasks, but with some inconsistencies across studies [22, 25]. As regards schooling, no effects were expected, given the low-level sensory abilities assessed by RASP; in studies on haptic processing, putative effects of schooling are intermingled with those of development [25].
The present study also provides cut-off values, for both the left and the right index fingers and separately for age group, for 2-point discrimination (Subtest 5), not previously reported in the original work [15]. The availability of cut-off scores for this subtest is clinically useful when assessing body-specific somatosensory deficits in neurological disorders, such as stroke, but also for other diseases such as anorexia nervosa [26, 27] and cerebral palsy [28].
The original work [15] provided normative data from participants in the United Kingdom, also testing stroke patients with left (N = 50) and right (N = 50) cerebral hemispheric damage; results were reported separately for the contralesional and the ipsilesional sides of the body in stroke patients, but not in healthy participants, for which normative data referred to the sum of all five regions tested (face, palm and back of the hand, sole and back of the foot).
However, unilateral focal cerebral lesions may bring about body-part-specific somatosensory impairments. For instance, impairments of tactile localization have been shown to occur in more than the 50% of stroke survivors at the wrist level, but rarely present at the contralesional side of the face (~7% of incidence) [10]. Differences in proprioception and tactile processing were reported for arms and legs, with the lower limb being more impaired [29]. Indeed, the lower and upper limbs tend to follow different trajectories of recovery, with more improvement in upper-limb than in lower-limb sensation [10]. As a consequence, it is clinically important to have body-part-specific normative data that can be used in prospective observational studies, largely neglected in post-stroke management [29]. Moreover, the availability of unique cut-offs for each subtest also permits their administration to a given body region in isolation, thus avoiding the delivering of subtests, considered less relevant by the clinician, to some patients, all of which can be time-consuming and uninformative [10].
In conclusion, the present study provides the first Italian normative data for the RASP and cut-off values that can be used to identify somatosensory impairments. The study confirmed the RASP as a valid tool capable of measuring several different aspects of somatosensory sensation. Standardized and completed with normative values, the RASP provides clinicians and researchers with a valid instrument for both assessment and follow up protocols.
Availability of data and material
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
Hammond F, Grafton L (2011) Sensorimotor assessment. In: Kreutzer JS, DeLuca J, Caplan B (eds) Encyclopedia of Clinical Neuropsychology. Springer New York, New York, NY, pp 2257–2258
Dyck PJ, Herrmann DN, Staff NP, Dyck PJ (2013) Assessing decreased sensation and increased sensory phenomena in diabetic polyneuropathies. Diabetes 62(11):3677–3686. https://doi.org/10.2337/db13-0352
Ropper AH, Samuels MA, Klein J (eds) (2014) Principles of neurology, 10th edn. Mc-Graw Hill, New York 1664 p
Kessner SS, Bingel U, Thomalla G (2016) Somatosensory deficits after stroke: a scoping review. Top Stroke Rehabil 23(2):136–146. https://doi.org/10.1080/10749357.2015.1116822
Borstad AL, Nichols-Larsen DS (2014) Assessing and treating higher level somatosensory impairments post stroke. Top Stroke Rehabil 21(4):290–295. https://doi.org/10.1310/tsr2104-290
Dombovy ML, Sandok BA, Basford JR (1986) Rehabilitation for stroke: a review. Stroke 17(3):363–369. https://doi.org/10.1161/01.str.17.3.363
Sommerfeld DK, von Arbin MH (2004) (2004) The impact of somatosensory function on activity performance and length of hospital stay in geriatric patients with stroke. Clin Rehabil 18(2):149–155. https://doi.org/10.1191/0269215504cr710oa
Bolognini N, Russo C, Edwards DJ (2016) The sensory side of post-stroke motor rehabilitation. Restor Neurol Neurosci 34(4):571–586. https://doi.org/10.3233/RNN-150606
Meyer S, Karttunen AH, Thijs V, Feys H, Verheyden G (2014) How do somatosensory deficits in the arm and hand relate to upper limb impairment, activity, and participation problems after stroke? A systematic review. Phys Ther 94(9):1220–1231. https://doi.org/10.2522/ptj.20130271
Connell LA, Lincoln NB, Radford KA (2008) Somatosensory impairment after stroke: frequency of different deficits and their recovery. Clin Rehabil 22(8):758–767. https://doi.org/10.1177/0269215508090674
Carey LM, Matyas TA (2011) Frequency of discriminative sensory loss in the hand after stroke in a rehabilitation setting. J Rehabil Med 43(3):257–263. https://doi.org/10.2340/16501977-0662
Fugl-Meyer AR, Jääskö L, Leyman I, Olsson S, Steglind S (1975) The post-stroke hemiplegic patient. 1. A method for evaluation of physical performance. Scand J Rehabil Med 7(1):13–31
Lincoln NB, Jackson JM, Adams SA (1998) Reliability and revision of the Nottingham Sensory Assessment for stroke patients. Physiotherapy 84(8):358–365
Rolke R, Magerl W, Campbell KA, Schalber C, Caspari S, Birklein F, Treede RD (2006) Quantitative sensory testing: a comprehensive protocol for clinical trials. Eur J Pain 10(1):77–88. https://doi.org/10.1016/j.ejpain.2005.02.003
Winward CE, Halligan PW, Wade DT (2002) The Rivermead assessment of somatosensory performance (RASP): standardization and reliability data. Clin Rehabil 16(5):523–533. https://doi.org/10.1191/0269215502cr522oa
Connell LA, Tyson SF (2012) Measures of sensation in neurological conditions: a systematic review. Clin Rehabil 26(1):68–80. https://doi.org/10.1177/0269215511412982
Steimann L, Missala I, van Kaick S, Walston J, Malzahn U, Heuschmann PU, Steinhagen-Thiessen E, Dohle C (2012) Rivermead assessment of somatosensory performance: validierung einer deutschen version (RASP DT) [Rivermead assessment of somatosensory performance: validation of a German version (RASP-DT)]. Nervenarzt 83(12):1632–1637. https://doi.org/10.1007/s00115-012-3614-6
Winward CE, Halligan PW, Wade DT, RASP (2012) Rivermead assessment of somatosensory performance. In: Operator Manual, 2nd edn
Oldfield RC (1971) The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia 9(1):97–113. https://doi.org/10.1016/0028-3932(71)90067-4
Kaneko A, Asai N, Kanda T (2005) The influence of age on pressure perception of static and moving two-point discrimination in normal subjects. J Hand Ther 18(4):421–425. https://doi.org/10.1197/j.jht.2005.09.010
Woodward KL (1993) The relationship between skin compliance, age, gender, and tactile discriminative thresholds in humans. Somatosens Mot Res 10(1):63–67. https://doi.org/10.3109/08990229309028824
Dinse HR (2006) Cortical reorganization in the aging brain. Prog Brain Res 157:57–80. https://doi.org/10.1016/s0079-6123(06)57005-0
Ribeiro F, Oliveira J (2007) Aging effects on joint proprioception: the role of physical activity in proprioception preservation. Eur Rev Aging Phys Act 4(2):71–76. https://doi.org/10.1007/s11556-007-0026-x
Kalisch T, Kattenstroth JC, Kowalewski R, Tegenthoff M, Dinse HR (2012) Age-related changes in the joint position sense of the human hand. Clin Interv Aging 7:499–507. https://doi.org/10.2147/CIA.S37573
Fernandes AM, Albuquerque PB (2012) Tactual perception: a review of experimental variables and procedures. Cogn Process 13(4):285–301. https://doi.org/10.1007/s10339-012-0443-2
Gaudio S, Brooks SJ, Riva G (2014) Nonvisual multisensory impairment of body perception in anorexia nervosa: a systematic review of neuropsychological studies. PLoS One 9(10):e110087. https://doi.org/10.1371/journal.pone.0110087
Keizer A, Smeets MA, Dijkerman HC, van Elburg A, Postma A (2012) Aberrant somatosensory perception in anorexia nervosa. Psychiatry Res 200(2-3):530–537. https://doi.org/10.1016/j.psychres.2012.05.001
Tsao H, Pannek K, Boyd RN, Rose SE (2015) Changes in the integrity of thalamocortical connections are associated with sensorimotor deficits in children with congenital hemiplegia. Brain Struct Funct 220(1):307–318. https://doi.org/10.1007/s00429-013-0656-x
Tyson SF, Hanley M, Chillala J, Selley AB, Tallis RC (2008) Sensory loss in hospital-admitted people with stroke: characteristics, associated factors, and relationship with function. Neurorehabil Neural Repair 22(2):166–172. https://doi.org/10.1177/1545968307305523
Funding
Open access funding provided by Università degli Studi di Milano - Bicocca within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval
Approval was obtained by the local ethics committee. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Russo, C., Spandri, V., Gallucci, M. et al. Rivermead assessment of somatosensory performance: Italian normative data. Neurol Sci 42, 5149–5156 (2021). https://doi.org/10.1007/s10072-021-05210-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05210-5